Patients journey to diagnosis and treatment of oral mucosal lesions: A report on three cases
Key Clinical Message
Delays in diagnosis and management of patients with oral mucosal lesions have serious implications for the patients. Early referral and collaboration between HCPs and OM specialists are essential in improving patients' quality of life and outcomes.
1 INTRODUCTION
Oral medicine (OM) was recognized as a specialty by the American Board of Dental Specialties in 2015.1 OM is a subspecialty of dentistry that deals with oral and maxillofacial diseases as well as the dental care of medically complex patients.1 OM specialists are trained to provide nonsurgical care for a variety of conditions, such as oral ulcerative disease, orofacial pain, and soft tissue lesions, including potential malignant disorders. In addition, they provide dental care for medically compromised patients.
Often, OM specialists are consulted to provide dental clearance before cardiac surgeries, chemotherapy, and head and neck radiation.2 Although OM's scope of practice is closely related to other dental specialties like periodontology, oral maxillofacial surgery, and special care dentistry, it also has a strong relation with other medical specialties like dermatology, gastroenterology (GI), neurology, oncology, otorhinolaryngology, and rheumatology. Therefore, OM is considered an example of interdisciplinary cooperation between medicine and dentistry. Physicians frequently encounter oral lesions, especially in patients with systemic diseases, including diabetes, malignancy, and immunocompromised patients. From this perspective, the diagnosis of oral mucosal lesions as outlined in this case series is a challenge in real-world practice.
Many healthcare providers (HCPs) are unfamiliar with the scope of practice of OM specialists. Only half (52%) of HCPs interviewed were aware of OM as an independent specialty, and only 50% of them have referred to OM clinics.3 Moreover, 50% of referring HCPs were unable to make a clinical diagnosis of an oral mucosal lesion, and only 40% of the provisional diagnosis provided in the referring letter concurred with the diagnosis made by the OM.4 In another study, only 28.5% of referred patients to a university-based OM clinic had an accurate provisional diagnosis.5 These remarkable findings indicate HCPs lack of competency skill in diagnosing oral mucosal lesions, causing delay in patient care. This has been clearly highlighted in this manuscript.
In this case series, we report on the journey of three patients from symptom onset to the diagnosis and management of oral mucosal lesions. We emphasize the concept of the early recognition and referral of oral disease. We aim to highlight the importance of proper collaboration between medical HCPs and OM specialists for the sake of a better patient experience.
2 CASE 1
2.1 Case history and examination
A 28-year-old male patient was referred from the rheumatology clinic for the evaluation of multiple tongue lesions. The patient reported a history of asymptomatic tongue lesions over a period of 5 years that appear spontaneously and disappear after a few weeks to reappear in different sites of the dorsum or sides of the tongue only. The patient reported mild burning with spicy food and denied any severe pain or burning, discharge, bleeding, or change in shape of the lesions. No other similar intraoral lesions were noted. No lesions were present on the skin, nose, scalp, or genital areas. The patient denied concurrent symptoms, such as fever, sore throat, or lymphadenopathy.
His past medical history was significant for gastroesophageal reflux disorder, for which he was taking omeprazole, and a history of Helicobacter pylori infection. His social and family history was non-contributory, and he had no known food or drug allergies.
The patient reported that the tongue lesions started around 5 years ago when he also complained of concurrent heartburn. He was evaluated by a GI consultant who ordered a gastroscopy, which showed a normal esophagus and mild gastritis. The patient was prescribed omeprazole that improved his symptoms, except for tongue lesions. A few months later, he developed gastrointestinal symptoms and sought another GI specialist's opinion. An esophagogastroduodenoscopy (EGD) and colonoscopy with multiple biopsies were recommended to rule out Crohn's disease. The surgical report showed mild gastritis, and H. pylori was detected. In addition, anti-Saccharomyces cerevisiae (ASCA) antibodies were negative, and Crohn's disease was ruled out. The patient was treated with amoxicillin, clarithromycin, and metronidazole that cleared the H. pylori infection, and the patient noted the disappearance of the tongue patches. Soon after he finished the treatment course, the tongue lesions presented again, and they were not diagnosed or addressed by any of the medical specialists he had seen. The patient visited an allergist or immunologist to evaluate his tongue patches and rule out autoimmune diseases. The physician ordered multiple testing, including food allergy screening, antinuclear antibodies ANA, anticentromere antibody testing, antidouble-stranded DNA test, antineutrophil cytoplasmic antibodies (ANCA) test, rheumatoid factor, and human leukocyte antigen HLA B51, all of which were negative. Rheumatoid arthritis and Bechet's disease were excluded.
Meanwhile, the patient was referred to the oral and maxillofacial clinic by his allergist for a tongue biopsy. The histopathology report was nonspecific and only showed hyperplastic changes and chronic inflammation. Furthermore, the patient was seen by a dermatologist for the same chief complaint, and no diagnosis was made. However, he was prescribed topical antifungal and topical steroid cream for the tongue, but the patient only used the antifungal cream without benefit. Last, the patient consulted a rheumatologist, and he was started on colchicine for a few weeks, which improved the tongue lesions to some extent, but they never completely disappeared. The patient was then referred to the OM clinic by a rheumatologist for evaluation and management of his tongue.
Extraoral examination revealed a well-developed man with no evidence of lymphadenopathy, salivary gland enlargement, or thyromegaly. However, intraoral examination showed multiple asymptomatic small round erythematous atrophic patches surrounded by white keratotic regular, slightly raised borders that involve the lateral and dorsal aspects and the tip of the tongue (Figure 1).
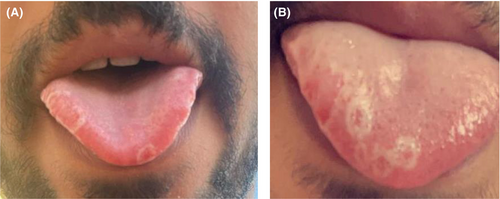
In our OM clinic, the patient was significantly stressed and concerned about tongue lesions. After reviewing the history of the chief complaint, full medical history, laboratory results, and correlation with the clinical presentation, the patient was diagnosed with beginning migratory glossitis (BMG), also called geographic tongue.
2.2 Conclusion and results
The nature of the disease was explained to the patient in detail, and he was assured of the nonmalignant nature of the disease. Given his lack of symptoms at the time of examination, no treatment was required, and follow-up visits were scheduled. The patient was followed up for a year and continued to show asymptomatic lesions.
3 CASE 2
3.1 Case history and examination
A 61-year-old female patient was referred to an OM clinic by a rheumatologist for the evaluation of multiple oral ulcers. The patient reported multiple ulcers on the tongue and buccal mucosa for a period of 4 years. She was evaluated by multiple HCPs, including a dermatologist and otolaryngologist. She sought the opinion of a general dentist who referred her to an oral and maxillofacial surgeon for further evaluation. Although a specific diagnosis could not be reached, she was given a prescription of topical oral gel and systemic antibiotics without benefit. She was then advised to see a gastroenterologist who, in turn, referred her to a rheumatology consultant. No previous oral or skin biopsy was performed.
The patient complained of generalized pain and a burning sensation related to multiple oral ulcers, which led to limited food intake. The patient denied any similar extraoral lesions on the skin, nose, scalp, or genital areas. The patient denied concurrent symptoms, such as fever, sore throat, or lymphadenopathy.
Her past medical history was non-significant, and she was not taking any medications. The patient denied having any food or drug allergies.
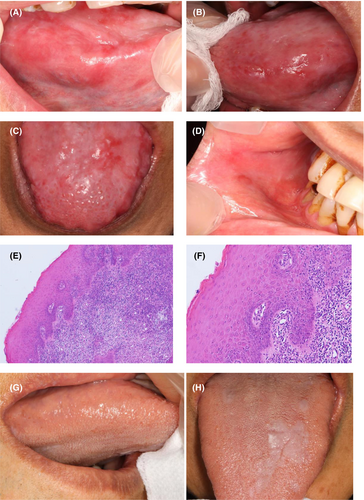
Upon oral clinical examination, the lower labial mucosa showed generalized mild to moderate erythema, and Wickham striae was noted. A shallow ulceration was detected in the left buccal mucosa. The tongue showed scattered areas of depapillation with Wickham striae on the lateral borders and dorsum side (Figure 2A–D).
3.2 Methods
Our initial diagnosis was erosive oral lichen planus (OLP). A tissue biopsy was obtained, and the histological report confirmed the clinical diagnosis (Figure 2E,F).
3.3 Results
The patient was assured and advised to follow the planned treatment. The importance of oral hygiene maintenance was explained. The patient was prescribed systemic steroids and topical antifungals for 2 weeks, and then she was changed to topical steroids and antifungals as needed after the lesions improved. Follow-up visits were arranged by teledentistry. The patient indicated that the burning sensation decreased, and she was able to eat, speak, and function without difficulty. In the last follow-up, a year after the first visit, the ulcers had significantly decreased in size, and the tongue lesions were resolved completely (Figure 2G,H). She was placed on regular follow-up visits with the OM clinic.
4 CASE 3
4.1 Case history and examination
A 71-year-old female patient with a chief complaint of multiple oral ulcerations of 2 months' duration. The patient reported that the lesions were spontaneous with mild lip swelling and denied any food triggers or recent changes to medications. She also denied a change in diet or dental treatment prior to the onset of ulcers. She reported severe oral pain and a burning sensation with eating difficulties. She denied similar lesions on the skin, nose, scalp, or genital areas. No concurrent symptoms were noted. She self-treated with herbal supplements without benefit. She consulted a general dentist and was prescribed a topical antifungal and topical hyaluronic acid without a specific diagnosis and without beneficial effects. She was then referred to a maxillofacial surgeon who did not give a diagnosis but prescribed 25 mg of prednisone for 2 weeks. Systemic steroids mildly improved the ulcerations as per the patient, but the lesions persisted. During that time, she had a follow-up visit with her rheumatologist, who referred her to our OM clinic for evaluation. Her past medical history was significant for rheumatoid arthritis, hypertension, and gastroesophageal reflux. She was on multiple medications, including angiotensin-converting enzyme, calcium channel blocker, pentazole, tizanidine, methotrexate, meloxicam, and multivitamins. She was on levothyroxine following a total thyroidectomy.
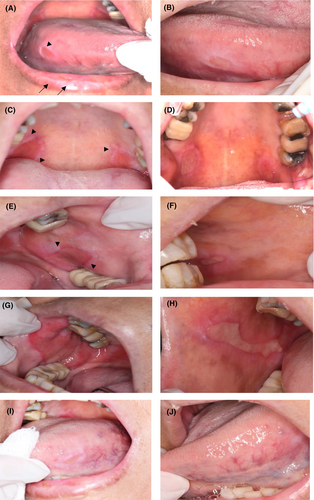
Extraoral examination showed a well-developed woman with no evidence of lymphadenopathy or salivary gland swelling. However, an intraoral examination revealed large ulcerations on the buccal mucosa bilaterally extending from the corner of the mouth posteriorly with a white striae. The right ulcer was larger in size than the left ulcer (Figure 3E,G). The tongue showed a few irregular, small ulcerations on the dorsum of the tongue and bilateral ulcers on the lateral sides (Figure 3A,I). In addition, relatively round ulcers were noted on the palate, specifically on the junction between soft and hard palate, with white lines at the peripheries (Figure 3C). Mild scattered crusting was seen on the lower lip.
4.2 Methods
The differential diagnosis included lichenoid reaction, oral erosive lichen planus, or healing erythema multiforme. An oral biopsy was recommended; however, the patient refused. Since the patient presented with severe pain, we elected to treat her with 40 mg prednisone for 10 days with prophylactic topical antifungal (Miconazole 20 mg) and recommended avoiding any food triggers.
4.3 Conclusion and results
Three weeks later, the patient presented to the clinic for follow-up, and she reported great improvement in her symptoms. The residual oral ulcers had significantly decreased in size but had not been resolved completely (Figure 3B,D,F,H,J). An oral biopsy was discussed again with the patient, but she refused. Due to the chronic course of the disease and considering the clinical presentation of the lesions, oral erosive lichen planus was highly suggested at that point; however, specimen taking was essential to confirm the diagnosis. Our patient continued to reject the biopsy, although she presented regularly to follow-up visits where her lesions completely resolved over time and her symptoms continued to improve. The decision was made to reevaluate her lesions periodically and revisit the idea of an oral biopsy in the coming appointments.
5 DISCUSSION
We report on three cases with oral mucosal lesions where the diagnosis was delayed for 5 years from the onset of symptoms. These patients visited an average of four medical doctors of different specialties and underwent numerous investigations and lab work in an attempt to reach a diagnosis. They also received several treatments that were inadequate. Although the patients were seeking medical advice, they were not directed to consult an OM specialist who was ultimately responsible for the diagnosis of oral mucosal lesions. This resulted in increased patient anxiety and distress due to a lack of diagnosis and treatment. This is in line with previous studies, which reported that patients with oral mucosal lesions underwent unnecessary tests and were not diagnosed or misdiagnosed despite being seen by multiple clinicians.5, 6 This resulted in diagnostic delays, which could worsen the prognosis for many conditions or at least affect the patients' oral health-related quality of life.5
The patient in the first case had only a mild burning sensation but was distressed by the recurrent nature of the lesions and the lack of diagnosis even after a biopsy. Most BMG lesions are asymptomatic, and despite being a benign lesion, BMG triggers concerns for patients and causes diagnostic difficulties for professionals, as the diagnosis is entirely based on the history and clinical presentation, and a tissue biopsy is unnecessary.7 The prevalence of BMG globally is 1%–2.5%, depending on the geographical area and the population studied.8 It has been associated with other medical conditions, but in general it requires conservative management only.9
Unlike the first patient, the other two patients suffered from pain, burning sensations, difficulty eating, speaking, and performing daily oral hygiene due to the extensive ulceration and erosion of the oral mucosa. OLP affects 1%–2% of the population of all racial groups. It shows a female predominance with a female-to-male ratio of 1.4:1.10 Erosive OLP is a clinical subtype of the broad category of OLP, a common chronic inflammatory disease that affects the skin and mucous membranes. Reticular OLP is characterized by white stria surrounded by well-defined erythematous borders, and it is the most common subtype and is usually asymptomatic. Erosive OLP, on the other hand, is extremely painful and refractory to therapies affecting the quality of a patient's life.11 Clinical features of OLP are very characteristic and usually help to establish the diagnosis, as in the case of both patients. However, biopsies of oral lesions are recommended to confirm the clinical diagnosis and exclude malignancy. A recent systematic review reported the rate of malignant transformation for OLP to be 1.37%,12 which signifies the importance of early diagnosis of the condition. One of our patients refused to undergo a tissue biopsy. In her case, the biopsy would be helpful to exclude other oral conditions, such as lichenoid reactions. However, clinically, the presentation fulfills the diagnosis criteria of OLP,10 and the patient responded well to the management plan.
Oral conditions affect patients' ability to eat and emotional status and have a significant effect on their quality of life.11, 13 A delay in diagnosis of oral and maxillofacial lesions and inappropriate treatment of lesions causes significant distress to patients. On average, patients have been evaluated by up to four specialists before being referred to OM specialist,14, 15 and the clinical diagnosis was delayed by an average of 16.8 months.16 Another study reported that the average diagnostic interval from the symptom's presentation to the clinical diagnosis for oral cancer was 70.2 days.17 This delay is a major clinical issue, as it could worsen the prognosis and affect the quality of the patient's life.
Oral disease accounts for 10% of healthcare costs in the United States.18 An increase in patients' age and the development of new treatment modalities with a wide range of side effects lead to increases in oral diseases.18 Interestingly, patients preferred to see a medical doctor instead of a dentist when having a non-healing oral ulcer.19 Unfortunately, this was a consistent finding in all our patients presented in this report. Despite this, medical practitioners do not include orofacial screening as a routine part of the patient's assessment.20
The perception of oral mucosal lesions among HCPs is probably “difficult and hard to diagnose.” It was reported that nonspecific oral ulcers were the most challenging for physicians to diagnose, followed by OLP or lichenoid reactions, graft-versus-host disease, potentially malignant oral lesions, and vesiculobullous diseases.18 The other concern among HCPs is when and what to refer? Some studies indicated that white-red lesions were the most common reason for referral and that the tongue was the most common site of concern.15 Others indicated that OLP and BMS were the most frequent conditions to be referred, followed by orofacial pain disorders, which is in line with the increase in the prevalence of chronic pain worldwide.5 However, specific guidelines and policies on referrals to OM are lacking among most healthcare systems.21
HCPs can improve access to oral healthcare for their patients, but this is dependent on HCPs receiving adequate training in oral diseases and oral manifestations of systemic diseases. One study showed that only 7% of family medicine specialists received oral health training during their residency.22 This could explain the lack of awareness and the low rate of referrals to OM from primary care specialists. On the other hand, dermatologists recognized OM as a specialty and made most of the referrals. This is likely because many dermatological diseases share many oral mucosal manifestations.18 Interestingly, all our referrals in these cases were from the rheumatology clinic.
Our patients were examined by many HCPs of different specialties who were focused on their specialty and did not consider referral to OM despite the lack of diagnosis or response to treatment. Pattern recognition is an acquired diagnostic strategy that is often utilized by clinical experts during routine practices to reach a diagnosis.23 This strategy should augment a comprehensive and systemic approach to medical problems to avoid diagnostic delays. These competencies should be developed during work-based training and assessments. However, most HCPs are not adequately trained or experienced in recognizing and diagnosing oral lesions.
To achieve the goal of reducing diagnostic delays and improving healthcare for patients with oral conditions, it is necessary to provide continued professional development courses in oral medicine to help physicians properly recognize and diagnose oral lesions.20 Incorporating a rotation in OM for residents, particularly in family medicine, dermatology, otolaryngology, and internal medicine training programs, will help enhance HCP competency in oral health.
In addition, OM specialists should promote their specialties and the diversity of services provided by them. The development of a standard referral guideline would be helpful in the management of patients with oral disease and would reduce the waiting time to reach a diagnosis or receive treatment.
6 CONCLUSION
Delays in the diagnosis and management of patients with common oral mucosal diseases have serious implications for patients. Healthcare requires well-trained specialists who work interprofessional to provide comprehensive and continuous care for their patients. Early diagnosis, referral, and collaboration between HCPs and OM specialists are essential in improving patients' outcomes and quality of life.
AUTHOR CONTRIBUTIONS
Lujain A. Homeida: Data curation; investigation; writing – original draft. Salwa A. Aldahlawi: Conceptualization; project administration; writing – review and editing.
FUNDING INFORMATION
The study had no financial support.
CONFLICT OF INTEREST STATEMENT
The authors report no conflict of interest.
CONSENT
Written informed consent was obtained from the patients to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.