Functional neurological disorder mimicking stroke: A case report
KEY CLINICAL MESSAGE
Even in the era of technology-guided medicine, the clinician must integrate into his daily practice a careful anamnesis and physical examination to be conducted within a close doctor–patient relationship. All these elements, together with tools such as teleconsultation and digitalized medical records, are able to significantly increase the effectiveness of health care action.
1 INTRODUCTION
Functional neurological disorder (FND), formerly known as “conversion disorder,” consists of neurological symptoms that usually involve sensory or motor function and that are inconsistent with known pathogenetic mechanisms of neurological disease or other known medical conditions.
Conservative estimates of its incidence hover around 12 cases per 100,000 per year.1 Emergency medicine also faces this problem with an estimated prevalence between 0.4% and 4% of all emergency room admissions.2
The onset, exacerbation, or maintenance of symptoms are commonly attributed to mental factors, such as stress or trauma in a general sense. The disorder tends to appear between late childhood and early adulthood, although it can occur at any age and is more common among women. Symptoms of this disorder often develop suddenly, and onset can sometimes follow a traumatic event. They usually consist of deficits in voluntary motor or sensory function, although they sometimes include coordination or balance problems and cognitive deficits or postural abnormalities of the limbs.
There may be single or repeated episodes, usually short lasting, but chronic symptoms have often been reported.
Diagnosis is based on medical history after excluding organic causes. Treatment begins with establishing a constant and supportive doctor–patient relationship and can be based on pharmacotherapy, psychotherapy but also on hypnosis or physiotherapy in selected cases.3
We present below a case of FND whose resolution was hindered by the finding of a vascular intracranial abnormality that could explain the onset symptoms but not all subsequent manifestations, leading to the prolongation of the patient's suffering and to unjustified medical services and costs.
2 CASE HISTORY/EXAMINATION
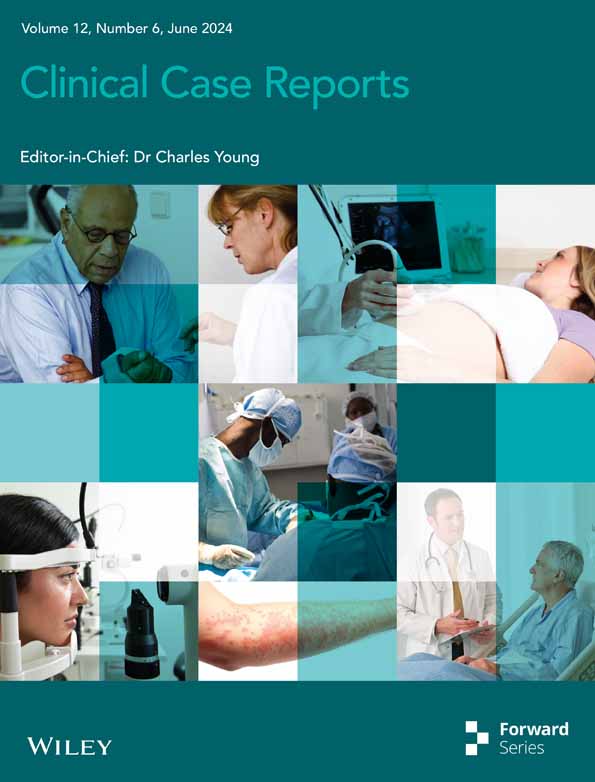
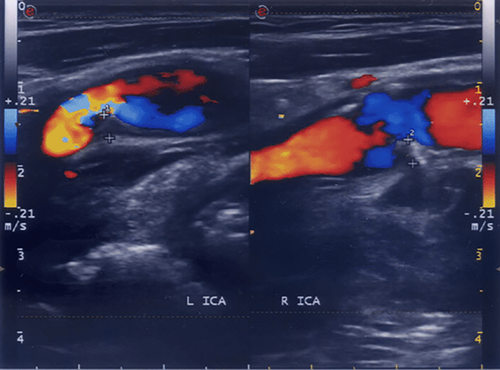
A 75-year-old woman, housewife, changed her general practitioner (GP) in June 2022. At the first visit she told him she had a stroke in April 2020 clinically characterized by slurred speech, imbalance, and confusion that lasted for 48 h without consequences. On that occasion, she performed brain MRI that showed chronic white matter disease (leukoaraiosis) (Figure 1), but no acute ischemic lesions, and brain CT angiography (CTA) (Figure 2) which showed the presence of carotid tortuosity and stenosis due to myointimal plaques. Home therapy consisted of barnidipine 20 mg (one tablet/day), clopidogrel 75 mg (one tablet/day), and atorvastatin 20 mg (one tablet/day).

After that she began suffering of recurrent dizzying attacks characterized by sudden onset, subjective vertigo (“I feel dizzy,” “my body feels like spinning”), absence of nausea and vomiting, unsteadiness of balance with wide-base walking, and the need to use supports while walking. Taking anti-dizziness drugs did not relieve the symptoms. The reported duration of the symptoms is variable from a few days to some weeks during which they slowly fade until disappearing. Due to recurrent attacks, she had been evaluated more than once in the emergency department and by several specialists that ascribed her symptoms to “recurrent minor strokes.”
Over the months, the number and the duration of the episodes had progressively increased until they became a permanent phenomenon leading to the loss of patient's autonomy.
At the time of the first visit, the general and neurological physical examination were normal and she reported a deflexed mood.
After a few days, her husband called the GP for the onset of a strong dizzying attack that prevented her from getting out of bed so that a home visit was arranged. At the visit, the vital parameters were normal (BP 140/80 mmHg, HR 70, RR 13, SaO2 98%), the patient was alert, oriented, and cooperative, even if she was suffering much, and speech was normal. She reported severe dizziness which she was not able to precisely characterize and which was heightened with every movement and change of position but not accompanied by nausea or vomiting.
With the help of her husband she sat up on the bed where she managed with great difficulty to maintain the control of the trunk. After reaching the upright position, she presented a precarious balance which was maintained with an enlarged support base. Walking was very uncertain and could only take place with the use of external supports and aids. Romberg's test was positive as the unsteadiness worsened considerably by asking the patient to remain upright with her eyes closed.
Continuing the physical examination, no strength and sensitivity deficits were found, the tendon reflexes were normal. There were no cranial nerve deficits. The index–nose test was weakly positive, especially on the right. The HINTS examination (head impulse, nystagmus, test of skew), used to assess an acute vestibular syndrome, was negative.
3 DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS, AND TREATMENT
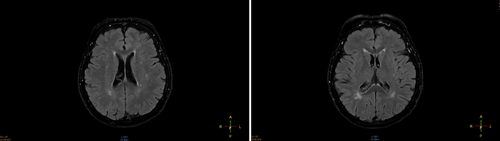
According to the dizziness diagnostic algorithm proposed by Muncie et al.4 (Figure 3), the probability that the disorder had a central or peripheral origin was very low. At this point, in the doctor's opinion, the most probable diagnostic hypothesis was that of FND.
Also a diagnosis such as persistent postural perceptual dizziness (PPPD), a chronic functional vestibular disorder, could be excluded considering its diagnostic criteria.5
To confirm his suspicions, the GP required a teleconsultation with a neurologist of the nearby university hospital during which he presented the case to his colleague deciding to send her the patient for a visit. As expected, the neurologist did not find neurological abnormalities.
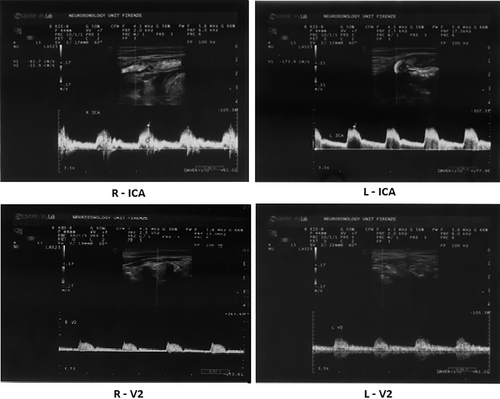
Moreover, when the patient was in Romberg position she had multidirectional oscillations that passed with distraction maneuvers. From the revision of the previously performed CTA, intracranial stenosis seemed not to be confirmed having probably been overestimated due to the presence of the marked tortuosity of the carotid vessels. The neurologist requested a transcranial Doppler (TCD) and a brain MRI to be compared with the one carried out in 2020 after the first stroke. Despite the confirmation of the tortuosity of the carotid vessels and the myointimal plaques (Figure 4) on TCD, the hemodynamic situation of the cerebro-afferent vessels was within normal limits (Figure 5) and, on MRI, there were, again, no signs of recent vascular lesions.
Taking together the clinical picture, the neurological evaluation, and the neuroimaging, the hypothesis of a “functional disorder” was confirmed. In addition to this, the previous diagnosis of stroke was questioned.
At this point the GP collected again the medical history in order to investigate the psychological field in more detail: the good doctor–patient relationship that was created in the previous months led the patient to reveal that about 20 years before she had lost a daughter following a serious illness. The tragic event had prompted her to attempt suicide and had been followed by admission to the psychiatric ward and by long months of psycho- and pharmacotherapy.
Following the recovery of psychic stability, the patient had decided not to talk about the event any more, imposing the same removal behavior on her family members until that day.
The GP, now definitely convinced that the patient was affected by FND, set a therapy with vortioxetine 5 mg to be increased to 10 mg once daily and proposed a psychotherapy intervention.
4 OUTCOME AND FOLLOW-UP
Within a few weeks, through a periodic follow-up carried out with outpatient visits and telephone interviews, the GP found a progressive improvement of the dizziness symptoms with a reduction in the intensity and frequency of the episodes.
5 DISCUSSION
- The careful anamnesis and physical examination that highlighted the discrepancy between the symptoms referred and the initial “diagnostic interpretation.” In fact the finding on CT angiography of a marked tortuosity associated with myointimal plaques in the carotid arteries induced an overestimation of the vascular stenosis. These elements, together with the symptoms complained by the patient, led to an incorrect diagnosis in the first phase.
- The close relationship established with the patient that allowed the GP to suspect the existence of “further elements” to be investigated in the psychological field overcoming the removal mechanism that led her to hide her tragic past.
- The possibility of direct interaction (via teleconsultation and digitalized medical record) between the GP and the specialist who reassessed the case which allowed a more precise presentation of the patient's disorder and medical history.
Functional neurological disorders (FND) frequently affects patients attending GP's clinics. These disorders are not easy to diagnose and can lead to long diagnostic and therapeutic paths because they often mimic other pathologies, leading the clinician to submit the patient to useless exams and visits.
The lack of precise diagnostic criteria makes the anamnesis, the clinical examination, and a close doctor–patient relationship three fundamental elements for reaching the diagnosis. All these elements are prerogatives of GP which can effectively reach an initial diagnosis and therapy to be confirmed if necessary by referring to the specialist.
In the described case, the initial diagnostic failure has been determined by a superficial taking charge of the patient and by a predominantly specialist management of the diagnostic therapeutic path.
A reduction in administrative burden and an improvement in the communication skills of GP could increase the average time dedicated to visiting and the quality of listening to patients; at the same time, the use of tools such as the teleconsultation and the digitalized medical record shared among all the professionals involved could facilitate their interaction increasing the effectiveness of health care action.6-9
AUTHOR CONTRIBUTIONS
G. Venturini: Conceptualization; data curation; writing – original draft; writing – review and editing. C. Sarti: Investigation.
FUNDING INFORMATION
The authors did not receive any funding for the publication of this article.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data on which this article was based are available on request from the corresponding author.