Successful management of gingival recession with creeping attachment: A case report
Abstract
Key Clinical Message
A successful management of a mandibular recession with creeping attachment using free gingival graft. This case highlights the “wait-and-see” approach in the treatment plan, emphasizing the root coverage.
This clinical report describes the case of a 23-year-old female patient with gingival recession of the mandibular left central incisor. The patient's symptoms included hypersensitivity and cosmetic improvements. After thorough examination, the patient was diagnosed with plaque-induced gingivitis on a reduced periodontium with acquired mucogingival deformities. Gingival recession was classified as Miller class II or Cairo Recession Type 1. The treatment plan consisted of a nonsurgical phase, followed by a surgical phase using a free gingival graft. The surgical procedure involved harvesting the graft from the palatal mucosa and placing it in the recipient site. Post-operative care and instructions were provided and a comprehensive follow-up schedule was established. At the 12-month evaluation, the patient exhibited healthy periodontal conditions with creeping attachment and complete root coverage. The success of the treatment approach demonstrates its effectiveness in addressing hypersensitivity and cosmetic concerns, while improving periodontal health. Factors influencing the achievement of creeping attachment are discussed, including recession width, graft position, bone support, tooth position, patient hygiene, graft thickness, and root surface treatment.
1 INTRODUCTION
Gingival recession, characterized by the displacement of the gingival margin below the cement-enamel junction,1 poses challenges in periodontology. This report presents the case of a 23-year-old female patient with gingival recession at the left mandibular central incisor, highlighting concerns regarding hypersensitivity and cosmetic improvement. The patient had no significant medical history and had undergone orthodontic treatment.
Clinical examination revealed plaque-induced gingivitis in the reduced periodontium, with acquired mucogingival deformities. The recession was classified as Miller Class II or Cairo Recession Type 1.
A two-phase treatment plan was implemented, starting with a non-surgical phase involving the establishment of optimal plaque control, use of desensitizing agents and periodontal debridement. Subsequently, a free gingival graft harvested from the palatal mucosa was used in the surgical phase.
At the 12-month evaluation, the patient demonstrated healthy periodontal conditions with a creeping attachment of 1.5 mm, indicating reattachment of the keratinized tissue to the root surface. Complete root coverage was achieved, accompanied by an increased in keratinized and attached soft tissues. This treatment approach effectively addressed the patient's concerns, resulting in improved periodontal health and overall satisfaction.
Various etiological factors contribute to gingival recession, including gingival inflammation, trauma from brushing, tooth malposition, inadequate attached gingiva, thin gingival biotype, frenum pull, and orthodontic treatment.2 Free gingival grafts were chosen because for their advantages of increasing keratinized tissue thickness and width, limiting future recession, and providing root coverage.3
Creeping attachment, characterized by coronal migration of the gingival margin and firm attachment to the root surface,4 was observed in this case. Factors such as recession width, graft position, bone support, tooth position, patient hygiene, graft thickness, and appropriate root surface treatment likely contribute to the successful achievement of creeping attachment.4 Periodontal maintenance and strict plaque control measures supporte healing and successful attachment.
In conclusion, this clinical report highlights the successful management of gingival recession with creeping attachment in a young female patient. A comprehensive treatment approach, including both nonsurgical and surgical interventions, achieved optimal results in terms of root coverage and patient satisfaction. Further research is needed to better understand the biological mechanisms of creeping attachment and refine treatment protocols for gingival recession management.
2 CASE PRESENTATION
By examining a 23-year-old female patient who presented with gingival recession at the mandibular left central incisor, we addressed her concerns of hypersensitivity and cosmetic improvement. The patient had no significant medical history and was a nonsmoker. She had previously experienced tooth baldness in the lower incisor-canine area and had undergone a 3-year orthodontic treatment.
An intraoral examination revealed a thin phenotype with a low full-mouth plaque score. There was no excessive tooth mobility, but narrow papillae, a shallow vestibule, a probing pocket depth of less than 3 mm, and a recession at the mandibular left central incisor with 3 mm depth and less than 3 mm of width. No attached or keratinized gingival tissues was found apical to the defect (Figure 1).

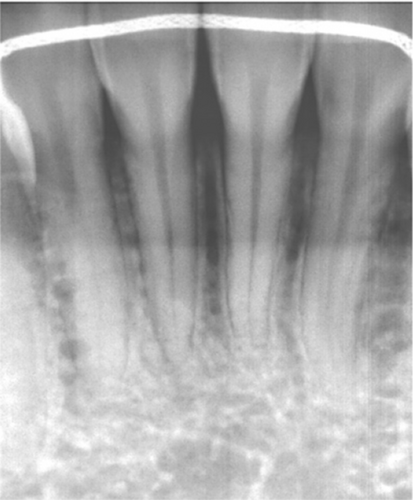
Radiographic examination of the anterior mandibular region revealed no interdental bone lysis (Figure 2).
3 METHODS
Based on the clinical findings, the patient was diagnosed with plaque-induced gingivitis on a reduced periodontium, with acquired mucogingival deformities around the teeth according to the American Association of Periodontology (2017) classification. Gingival recession at the mandibular left central incisor was classified as Miller class II or Cairo Recession Type 1 (RT1) (Figure 1).
The treatment plan involved a two-phase approach. First, a non-surgical phase was carried out, which included oral hygiene improvement, prescription of appropriate brushing equipment, use of desensitizing toothpaste as well as periodontal debridement. Subsequently, the surgical phase was scheduled by using a free gingival graft. Under local anesthesia, the exposed root surface was thoroughly instrumented using Gracey curettes. An intrasulcular incision was made on the buccal aspect of the affected tooth, extending mesially and distally, using 3 mm horizontal incisions to encompass the adjacent papillae.
From each horizontal incision, vertical releasing incisions were divergently placed and extended well into the alveolar mucosa. A thin partial-thickness flap was created, providing a smooth periosteal bed for the graft without excision. The dimensions of the recipient site were meticulously measured and outlined in the palate region, between the canine and second premolar (Figure 3).
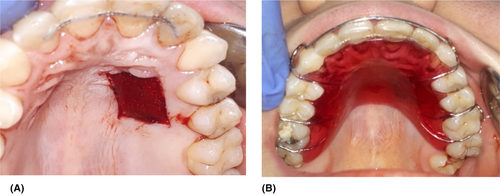
The graft, approximately 2 mm thick, was harvested using a #15C scalpel and placed in a damp compress soaked in physiological saline. To enhance postoperative comfort and accelerate healing at the palate site, a hemostatic sponge was inserted at the sampling donor site, and the palate was protected with a prefabricated resin plate, worn by the patient for 1 week after the surgery (Figure 3).
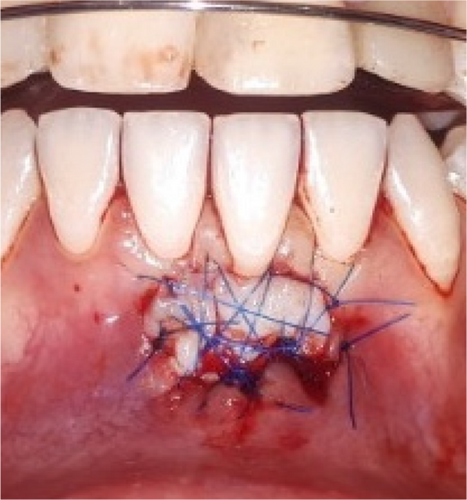
The free gingival graft was then stabilized at the recipient site and anchored to the periosteum using simple and suspended sutures, employing a 5.0 blue non-resorbable monofilament until complete graft stability was achieved. The graft-partial-thickness flap assembly was sutured primarily to promote the healing of the recipient site primarily (Figure 4).
Post-operative instructions were provided, emphasizing avoidance of mechanical trauma, tooth brushing, or excessive muscle traction in the surgical area. The patient was prescribed 200 mg of non-steroidal anti-inflammatory drugs twice daily for 3 days, along with a 0.12% chlorhexidine gluconate-based antiseptic twice daily for 2 weeks following the surgery.
4 RESULTS
After a 2-week healing period, the sutures were removed without any signs of necrosis (Figure 5).

A comprehensive follow-up schedule was established, with weekly appointments for the next 2 months. During this period, strict mechanical plaque control measures were implemented by using a soft toothbrush.
At the 2 months, the patient presented with stabilization of clinical results, with an increase in the thickness of the keratinized tissue, and a persistence of a narrow recession of 1.5 mm.
At the 12-month evaluation, the patient exhibited healthy periodontal condition. Notably, there was a creeping attachment of 1.5 mm, indicating the gradual reattachment of the keratinized tissue to the root surface. Complete root coverage was achieved, accompanied by an increased presence of keratinized and attached soft tissues (Figure 6). No signs of deep pocketing, bleeding on probing, or sensitivity were observed.

This successful outcome highlights the efficacy of the treatment approach, which involves a nonsurgical phase followed by a surgical procedure using free gingival graft. The patient's concerns regarding hypersensitivity and cosmetic appearance were effectively addressed, resulting in improved periodontal health and overall satisfaction.
5 DISCUSSION
Gingival recession is a commonly encountered issue, characterized by the displacement of the gingival margin below the cement-enamel junction, exposing the root surface to the oral environment.1 This condition can have adverse effects on aesthetics, increase susceptibility to root caries, and cause hypersensitivity problems. In our case, the patient's primary concerns were hypersensitivity and aesthetic appearance.
Research conducted by Albandar et al.5 has shown that gingival recessions ≥1 mm are most prevalent in the maxillary first molars and mandibular central incisors, which aligns with our case presentation.
The classification of gingival recessions is determined by the coronoapical extension (with or without involvement of the mucogingival junction) and the level of interproximal periodontal support.6 In our case, as the interproximal support was intact and the coronoapical extension involved the mucogingival junction, the gingival recession at the mandibular left central incisor was classified as Miller Class II and Cairo Recession Type 1 (RT1).
Several etiological factors contribute to gingival recession, including gingival inflammation, trauma from brushing, tooth malposition, inadequate attached gingiva, thin gingival biotype, frenum pull, and orthodontic treatment.2 In our case, the patient exhibited a thin gingival biotype, insufficient attached gingiva, a history of dental overlapping in the lower canine-incisor region, and a previous 3-year orthodontic treatment.
Gingival recession often leads to dentinal hypersensitivity, a condition characterized by brief, intense pain resulting from the exposed dentin. The prevalence of this sensitivity in patients with periodontal issues varies from 72.5% to 98%. Numerous theories have been proposed to elucidate the mechanism behind this occurrence, which involves the exposure of dentinal tubules. Nonetheless, the precise workings of this phenomenon remain incompletely understood.7
Different approaches are available for the treatment of dentinal hypersensitivity. The first step should include the use of a desensitizing agent, as described in our case. In the absence of cosmetic concerns, topical fluoride can be applied to the root surface to increase mineral precipitation and reduce pain. If pain persists, laser therapy, restorative treatments, and endodontics can be performed. When dentine hypersensitivity is associated with aesthetic discomfort, as in our study, treatment should include restorative methods and/or periodontal surgery.7
Periodontal plastic surgery encompasses a range of techniques that allow clinicians to address patient concerns and fulfill their expectations regarding the management of gingival recessions.
Over the years, various grafting techniques have been described for the management of gingival recessions, including free gingival grafts, connective tissue grafts, pedicular flaps, and guided tissue regeneration.8, 9 Tooth location has been identified as a crucial factor in predicting the root coverage success, as demonstrated by Zucchelli et al. Mandibular incisors, as in our case, are associated with less favorable outcomes because of the specific challenges presented by the mandibular anterior region.10
The major dilema of the mandibular anterior region is the high muscle attachments which may destabilize the graft's healing. The surgical approach's choice must be justified by the survival of the graft on the avascular root surface and the alternative to increase keratinized gingiva.11
With modern periodontal plastic surgery techniques as coronally advanced flap of tunnel techniques, the deep palate connective tissue and palate connective tissue graft without the overlying epithelium may not exactly induce keratinization of non-keratinized epithelial Cells.11
Free gingival grafts is a commonly preferred and easily applied surgical method when considering tissue grafts for the anterior mandibular region. It effectively increase the thickness and width of keratinized tissues, obtain keratinized gingiva and eliminate high muscle attachments in one surgical visit.11 In this case, we followed the technique described by Sullivans and Atkins.3
This therapy involves harvesting a portion of the soft tissue containing epithelial and connective tissues from a donor site, often the palatal mucosa. The graft is then placed in a prepared recipient bed,3 precisely at the left mandibular central incisor, as in our case. Proper immobilization of the graft is crucial to ensure successful revascularization. In our case, we used simple and suspended sutures until complete stability of the graft-partial-thickness flap was achieved.
However, it is important to note that free gingival grafts may be associated with discomfort and hemorrhage at the donor site, resulting in increased patient morbidity. Additionally, aesthetic alterations can occur because of color disparities between the palatal portion and the surrounding tissues.12
In this case, to overcome these disadvantages, we used a hemostatic sponge at the sampling donor site, covered by a resin plate. The slight color disparity at the final healing was not apparent, and was not displayed during mandibular functions; hence, it did not pose any aesthetic concerns.
The most challenging key in root coverage is the inadequate blood supply to the portion of the graft placed on the exposed avascular root surface.13 Histological healing studies have shown connective attachment in the inner part of the flap and a long junctional epithelium in the coronal part.13
Two ways of healing were mainly noted when using gingival graft: bridging and creeping. Studies over literature have not make the red line to differentiate the two mechanisms.
The main point of determination is the healing time. It was determined that bridging is the residuum of the original graft on the denuded root surface, resulting from the escape of necrosis from tissue remodeling. It took part in the early phase of healing up to the first month of healing, while the root coverage obtained later was described as creeping attachment.4
In literature, Goldman first described the creeping attachment in 1964.14 It has been defined as the coronal migration of the gingival margin after a mucogingival surgery in the coronal direction over portions of a previously denuded root. The newly formed gingival tissue is firmly attached to the root surface, and the sulcular probing shows no periodontal pocket.14 It has been described during the second month after surgery and continuing for 12 months and more.14 Recently, it has been reported around implants and restored teeth.15
Several studies have shown creeping attachments on the mandibular anterior teeth with narrow recessions (width less than 3 mm), as in our case, with an average coverage of 1 mm.14 Our findings are in accordance with the existing literature. At the 12-month follow up, we noted a coronal creeping attachment of 1.5 mm, with complete root coverage.
Matter described several factors that appear to influence the occurrence of creeping attachment, including recession width, graft position, bone resorption, tooth position, and patient hygiene.14 In our case, the presence of a narrow recession, intact interdental bone, absence of tooth malposition, and good plaque control likely contributed to the favorable outcome of creeping attachment.
The underlying biological mechanisms of creeping attachment have not been fully elucidated, but they may involve various parameters associated with gingival wound healing.14 The process of gingival wound healing involves the granulation phase, characterized by gingival thickening, followed by a maturation phase involving coverage of the root surface.16
The thickness of the harvested soft tissue graft plays a significant role in future root coverage and can impact creeping attachment. It has been observed that soft tissue thickness exceeding 0.8 mm results in complete root coverage, while thickness below 0.8 mm only achieves partial coverage.17 Therefore, in our case, the use of a 2 mm thick graft may have contributed to enhanced root coverage.
Wennström et al. demonstrated that the height and thickness of the periodontal tissue are interconnected. They reported a ratio of approximately 1.5:1 between the height and width of the free gingiva, suggesting that increasing gingival thickness can enhance gingival height.18
The use of conditioning agents, such as citric acid or tetracycline hydrochloride solution, for exposed root surfaces in coverage procedures has been described in various studies. These agents are believed to enhance the formation of new fibrous attachments and to promote root coverage. However, controlled studies have indicated that these protocols have no clinical benefit.19 In our case, no adjuvant was used for root surface treatment before placing the tissue graft. Instead, scaling and root planning were performed to facilitate the creeping attachment.
Periodontal maintenance is crucial for the healing of plastic surgery and the success of creeping attachment. In this particular case, the patient had a low plaque index and was motivated to maintain good oral hygiene through proper brushing techniques and regular maintenance sessions.
Overall, the combination of favorable factors such as recession width, graft position, bone support, tooth position, patient hygiene, graft thickness, and appropriate root surface treatment contributed to the successful achievement of creeping attachment in our case.
The successful management of gingival recession in this clinical report highlights the efficacy of a treatment approach involving a nonsurgical phase followed by a surgical procedure utilizing a free gingival graft. Achievement of complete root coverage, increased presence of keratinized and attached soft tissue, and creeping attachment demonstrated the positive outcomes that can be obtained.
Factors such as recession width, graft thickness, bone support, tooth position, patient hygiene, and appropriate root surface treatment significantly influence the treatment success. This case emphasizes the importance of considering multiple factors in the management of gingival recession and provides valuable insights for clinicians in their treatment planning and decision-making. In mucogingival plastic surgery, it might be wise to adopt a “wait-and-see” approach before considering the next step of surgery.
AUTHOR CONTRIBUTIONS
Sihame Assimi: Conceptualization; resources; validation; writing – original draft; writing – review and editing. Zouheir Ismaili: Writing – review and editing. Saloua Dghoughi: Writing – review and editing.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
This research received no external funding.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was conducted in accordance with the Declaration of Helsinki. The patient was treated in accordance with his clinical needing. Ethical review and approval were waived for this study due to this being one clinically-treated patient whose treatments was not originally intended to be the subject of a case report.
CONSENT
Written informed consent was obtained from the patient to publish this case report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data related to the study can be provided on reasonable request.