Decades of stability of conjunctival vascular malformations in two patients
Abstract
Key Clinical Message
Conjunctival hemangioma and lymphangioma are rare and their long-term follow-up description has been scarce. In our two patients, conjunctival vascular and lymphatic malformations remained stable in decades and could be observed without treatment.
A 65-year-old woman with diabetic retinopathy underwent glaucoma surgery to construct a filtering bleb adjacent to conjunctival hemangioma, and showed bleb function and stable hemangioma for a decade. A 1.5-year-old girl with right eye lid and cheek swelling by orbital to facial lymphangioma was followed for visual acuity development. Conjunctival lymphangioma was stable in 20 years.
1 INTRODUCTION
Hemangioma of the conjunctiva and eye lid is evident clinically as congenital anomalies on rare occasions.1-6 Recently, hemangioma and lymphangioma are all together designated as vascular malformations in the entity of vascular anomalies which contain the other sub-entity of vascular tumors, according to the International Society for the Study of Vascular Anomalies (ISSVA) classification.7, 8 Vascular tumors show proliferative changes of vascular endothelial cells while vascular malformations consist of structural vascular abnormalities. Based on the structural components of capillary blood vessels or veins, capillary and cavernous hemangioma are capillary and venous malformations, respectively. Lymphangioma is named as lymphatic malformations.
Here we present one patient with conjunctival and eye lid hemangioma and another patient with lymphangioma in the face, orbit and conjunctiva to show long-term stability in decades.
2 PRESENTATION OF CASE 1
A 65-year-old woman was referred to a University Hospital for high intraocular pressure in the right eye with congenital conjunctival hemangioma (Figure 1A,B). Three years previously, she had experienced femoral neck fracture on the right side and been diagnosed as diabetes mellitus and preproliferative diabetic retinopathy. She underwent panretinal laser photocoagulation in both eyes. At the time of the referral, she was healthy and physical examinations detected no particular findings. She had no other past history. The hemoglobin A1c was 6.5% by taking vildagliptin 50 mg daily, metformin 500 mg daily, and a combination tablet of mitiglinide 10 mg and voglibose 0.2 mg prior to every meal for diabetes mellitus. The intraocular pressure was 25 mmHg in the right eye and 18 mmHg by taking acetazolamide 500 mg daily and using 0.005% latanoprost once daily and combination eye drops of 1% dorzolamide and 0.5% timolol twice daily in both eyes, together with 0.1% brimonidine twice daily in the right eye. The best-corrected visual acuity in decimals was 0.3 in the right eye and 0.2 in the left eye. Slit-lamp examinations showed the clear cornea and posterior subcapsular cataract in both eyes. Fundus examinations revealed the stable retinopathy with laser scars in both eyes (Figure 1C,D). Gonioscopic examinations disclosed congestive trabecular meshwork (Figure 1E) in the temporal and inferior quadrants of the right eye and no neovascularization in the angle or iris of both eyes.
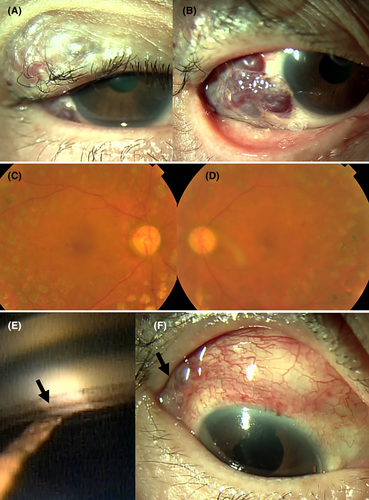
3 TREATMENT AND FOLLOW-UP IN CASE 1
She underwent trabeculectomy with sponge-applied 0.04% mitomycin C for 5 min combined with cataract surgery (phacoemulsification and intraocular lens implantation) in the right eye (Figure 1F). A week later, she underwent cataract surgery in the left eye. Two years later from the initial visit, she developed non-absorbing vitreous hemorrhage in the left eye and underwent vitrectomy with endo-laser coagulation. The diabetic retinopathy in both eyes was stable (Figure 2A–D), and the conjunctival filtering bleb kept the function in adjacent to stable conjunctival hemangioma (Figure 2E–H). She maintained the intraocular pressure in the right eye around 10 mmHg only with 0.1% betamethasone four times daily in the follow-up for 10 years from the initial visit. The intraocular pressure in the left eye was around 20 mmHg with 0.005% latanoprost once daily, 0.1% brimonidine twice daily, and combination eye drops of 1% dorzolamide and 0.5% timolol twice daily. The best-corrected visual acuity was 0.3 in the right eye and 0.9 in the left eye.
4 PRESENTATION OF CASE 2
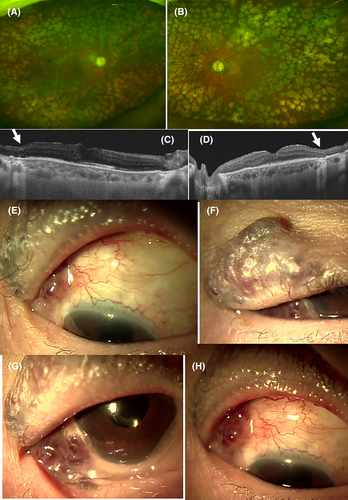
A 1.5-year-old girl was referred to an ophthalmologist for checking eye position and blepharoptosis. She had been noticed to have swelling of the upper eye lid and cheek on the right side from the birth, and was diagnosed as facial vascular (lymphatic) malformation. Magnetic resonance imaging (MRI) showed fluid-containing lobulated lesions in the nasal part of the right orbit and also in the cheek (Figure 3A). At the initial visit, the eye position was orthophoric, and showed good response to optokinetic striped drum rotation in both directions. She showed good eye tracking response and had no restriction in eye movement. Retinoscopic examinations showed no marked refractive error and funduscopic examinations showed normal retina and optic disc in both eyes. She had the same distance of the lid margin to the corneal light reflex in both eyes, indicating no blepharoptosis. At the age of 3.5 years, autorefraction showed no refractive errors in both eyes and the visual acuity in decimals measured with Landolt-C cards was 1.0 in both eyes. Afterwards, she was followed once or twice a year by an ophthalmologist and a plastic surgeon.

5 TREATMENT AND FOLLOW-UP IN CASE 2
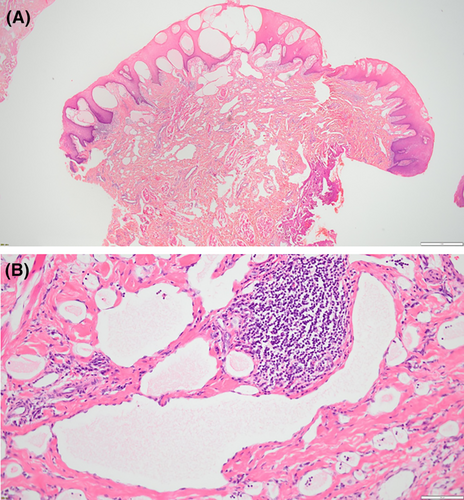
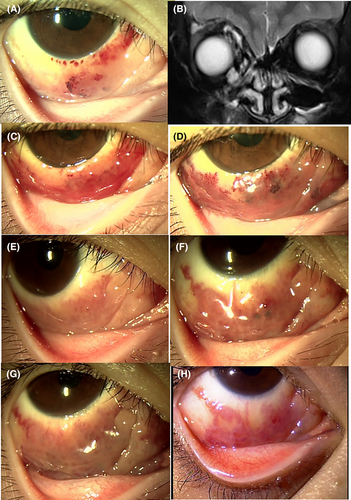
At the age of 5 years, she showed somewhat reduced lesions of lymphangioma on the nasal side in the right orbit on MRI (Figure 3C,D), in association with bumpy appearance of the bulbar conjunctiva on the nasal to inferior side of the right eye, which was caused by orbital lymphangioma (Figure 3B). At the age of 5 years and 8 months, she underwent lip lesion resection on the right side to reduce the deformation of the lip and cheek. The pathological examination showed vascular channels with no red blood cells in anomalous patterns which were surrounded by fibrous tissue beneath the stratified squamous epithelium of the lip (Figure 4A,B). The pathological diagnosis was lymphangioma.
At the age of 7 years, she developed hemorrhage in anomalous vascular channels in the bulbar conjunctiva in the nasal and inferior quadrants (Figure 3E) and she showed clear bumpy conjunctiva in a month (Figure 3F), indicating spontaneous resolution of hemorrhage. MRI showed no change in the orbital lesions (Figure 3G). She was stable in the following 4 years (Figure 3H,I) until the age of 11 years when she again developed hemorrhage in conjunctival vascular channels on the right side (Figure 5A) and MRI showed the further reduced lesions on the nasal side in the right orbit (Figure 5B). In the following years, she continued to show reddish bumpy conjunctival lesions (Figure 5C–H) which were covered by the lower eye lid until the age of 20 years at the last visit. She was cosmetically satisfied with the state of her face and eye. The best-corrected visual acuity was 1.2 in both eyes with the same degree of astigmatism at −1.0 diopter.
6 DISCUSSION
Conjunctival hemangioma and lymphangioma are rare and their long-term follow-up results are lacking in the literature. The aim of this study is to report the long-term outcome of conjunctival vascular malformations in the natural course. The first patient had stable manifestation of conjunctival and eye lid hemangioma since her youth. She underwent filtering surgery for glaucoma in the right eye with conjunctival hemangioma and was followed for 10 years. The second patient presented facial and eye lid swelling on the unilateral side from the birth and was followed as orbital and facial lymphangioma for 20 years. The present two patients showed the stable nature of conjunctival hemangioma and lymphangioma in decades and support observation without intervention as a treatment option.
The first patient (Case 1) was presented to us because of uncontrollable high intraocular pressure after panretinal laser photocoagulation for diabetic retinopathy. She did not show iris and angle neovascularization but did show congestion of Schlemm's canal in trabecular meshwork probably due to high venous pressure which could be attributed to the presence of hemangioma. Trabeculectomy as a glaucoma surgery was performed to construct a conjunctival filtering bleb adjacent to the conjunctival hemangioma. The filtering bleb had kept the function in a decade to maintain the normal level of intraocular pressure while the conjunctival hemangioma remained unchanged.
The second patient (Case 2) with facial and eye lid swelling on the right side from the birth was diagnosed by MRI as lymphangioma in the orbit to the cheek and lip. In terms of the lip swelling, she did not have any problem in sucking milk and in chewing food later. In terms of the eye lid swelling and the presence of orbital lesions, her pupillary area was not covered by the lid swelling on the right side and the eye movement had no restriction. She, therefore, did not have a risk for deprivation amblyopia. Under the circumstances, she did have a future risk for developing anisometropic amblyopia caused by corneal astigmatism as sequelae to thick upper eye lid,9 and was followed ophthalmologically to check the development of visual acuity.
In the course of this second patient, sclerotherapy to obstruct abnormal vascular channels was considered as a treatment option for the facial swelling. After all, we did not perform interventional radiology because there was a high risk for developing central retinal artery occlusion sequel to facial sclerotherapy, based on vascular anastomoses among facial vessels and orbital vessels.10 Instead, lip lesion was resected for cosmetic reasons and was proven pathologically as lymphangioma or lymphatic malformation. Thereafter, the conjunctival lesions became evident due probably to hemorrhage in lymphatic malformations in the anterior orbit, and gradually subsided to show stable nature of the conjunctival lesion.
From the cosmetic point of view, conjunctival hemangioma in the first patient was located in the superotemporal bulbar conjunctiva and was covered by the upper eye lid. In the second patient, conjunctival lymphangioma with vascular channel hemorrhage was located in the nasal and inferior bulbar conjunctiva and was covered by the lower eye lid. In contrast, lip deformation caused by subcutaneous lymphangioma was evident in this second patient, and her family wished for the child to have surgery to resect the lesions before entering an elementary school. The psychological impact of the facial lymphangioma should be thus considered to choose the observation or surgical intervention in the course.
In conclusion, conjunctival vascular and lymphatic malformations in the present 2 patients remained stable in decades and could be observed without treatment. Since the intraocular pressure would be influenced by the episcleral venous pressure, a risk for the elevated intraocular pressure in the presence of conjunctival vascular malformations remains a concern for ophthalmologists.
AUTHOR CONTRIBUTIONS
Toshihiko Matsuo: Conceptualization; data curation; investigation; methodology; resources; writing – original draft. Takehiro Tanaka: Investigation; methodology; resources; writing – review and editing. Yoshihiro Kimata: Investigation; methodology; resources; writing – review and editing.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
The authors receive no financial support for the research, authorship, and/or publication of this article.
CONFLICT OF INTEREST STATEMENT
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ETHICS APPROVAL
Ethics committee review was not applicable due to the case report design, based on the Ethical Guidelines for Medical and Health Research Involving Human Subjects, issued by the Government of Japan.
CONSENT
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Open Research
DATA AVAILABILITY STATEMENT
Additional data are available upon reasonable request to the corresponding author.