Small bowel obstruction in a 29-year-old male with congenital peritoneal bands: A rare case report from Syria
Key clinical Message
This case highlights the significance of maintaining clinical suspicion for CPBs in adults presenting with SBO. Early surgical intervention, offering both diagnosis and treatment, is essential for managing this rare cause of SBO. Increased clinical awareness of CPBs will help ensure they are considered in the differential diagnosis of adult patients with bowel obstruction.
1 INTRODUCTION
Small bowel obstruction (SBO) is an emergent condition that may be encountered by many physicians in their practice. There are many common causes and known risk factors that usually raise the clinical suspicion of bowel obstruction. However, one of the most enigmatic etiologies for this condition is congenital peritoneal bands (CPBs).
CPBs are intraperitoneal adhesions unrelated to abdominal procedures. In rare cases, infants and young children may suffer from bowel obstruction caused by CPBs but it is extremely infrequent in adults. The underlying pathophysiology is postulated to be due to abnormal adhesion of the peritoneal folds during fetal development. CPBs are responsible for between 7% and 12% of intestinal obstruction in people with no previous history of abdominal surgery and without a strangulated parietal hernia. Congenital bands have very infrequently been observed to compress the jejunum.1, 2
Radiography and computed tomography scans are valuable in distinguishing various diseases, but they do not provide a definitive diagnosis for intestinal obstruction resulting from a congenital band.3
When assessing CPBs, it's essential to consider Meckel's diverticulum, a congenital abnormality resulting from the improper absorption of the yolk sac in the intestine. Occasionally, the yolk arteries can turn into mesodiverticular bands (MDB), leading to symptomatic Meckel's diverticulum and subsequent intestinal obstruction.4 The only way for a definitive diagnosis is surgical exploration.2
In this case report of a 29-year-old man with SBO we highlight the importance of maintaining clinical suspicion for CPBs in adults with bowel obstruction.
2 CASE PRESENTATION
2.1 Case history
A 29-year-old male patient was admitted to the emergency department with a 10 day history of severe abdominal pain and bilious vomiting. Initially, the pain was described as tolerable and occasionally relieved by antispasmodic medications. The patient had no significant medical history, abdominal surgical procedures, or traumatic injuries in the abdomen. He had no history of diarrheal illness and he takes no medications. Blood pressure was 105\68 mm Hg with a heart rate of 82 beats/min. On physical examination, abdominal distention with severe diffuse tenderness and generalized rebound tenderness was evident. Bowel auscultation demonstrated hyperactive sounds. Rectal examination was normal.
2.2 Differential diagnosis, investigations, and treatment
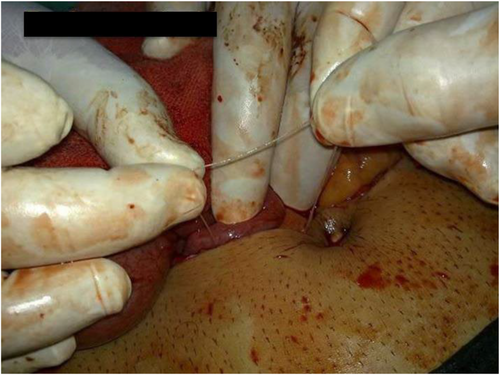
Laboratory results revealed a white blood cell count (WBC) of 10.1 × 103/L (77% neutrophils) and a normal amylase level. A chest X-ray was normal. Abdominal ultrasound revealed significant distention of the intestinal loops suggesting mechanical SBO and prompting surgical intervention. Electrolytes were within normal limits. Intravenous fluids were administered, and nasogastric tubes were placed. After that, an open laparotomy was performed and revealed a flaccid band with a broad mesenteric origin, constricting one of the jejunal loops and measuring approximately 20 cm in length (Figures 1 and 2). The band was excised and the affected loop was released. Additionally, an appendectomy was performed, and the abdomen was drained and closed. The Drainage was not indicated but was carried out as a preventative measure.

2.3 Outcome and follow-up
Post-operatively, the patient experienced a minor episode of vomiting but subsequently passed flatus and feces, indicating recovery. The patient was discharged with suture removal on the eighth day, and the patient remained in good condition. Follow-up examinations and monitoring were conducted to ensure the patient's ongoing recovery and well-being. The histopathological examination of the removed band revealed reactive fibrosis and chronic non-specific inflammation.
3 DISCUSSION
SBO is a well-known medical condition primarily attributed to postoperative adhesions. However, acute SBO in adults without a history of abdominal surgery, trauma, or clinical hernia is less common and can have various underlying causes.
Intestinal obstruction can result from atresia of the jejunum, ileum, duodenum, or colon; volvulus; annular pancreas; or congenital bands.5
The leading cause of intestinal obstructions, accounting for a substantial 60%, is adhesions resulting from prior laparotomy. Hernias contribute to approximately 25% of cases, while neoplasms are responsible for about 5%–10%. Less common factors include inflammatory bowel disease, midgut volvulus, and intussusception. Remarkably, it has been observed that in 95% of patients who have undergone previous abdominal surgeries, adhesions or bands can lead to obstructions, making them the most frequent causes of SBO. Internal hernias, although a relatively rare cause of SBO, make up only 0.2%–0.9% of cases.6
The presence of adhesive bands in patients without a history of penetrating abdominal trauma, surgery, or underlying inflammatory conditions is a notably rare phenomenon. Additionally, occurrences of SBO attributed to these congenital bands are exceptionally infrequent.7
Unlike other causes of bowel obstruction, such as postoperative adhesions or hernias, CPBs typically occur in patients without a significant history and risk factors. This lack of risk factors makes CPBs even more elusive because they are not often suspected in individuals who do not fit the typical profile of patients at risk for bowel obstruction.
CPBs originate from abnormal adhesions of peritoneal folds that form during the embryonic development of the gastrointestinal tract. These adhesions represent remnants of fetal vessels and/or ventral mesentery. Normally, these structures should resorb as the fetus matures, but in the case of CPBs, they persist into adulthood. The unusual origin of CPBs sets them apart from other causes of bowel obstruction.8
Occlusion due to these bands results either from compression of the small bowel or from trapping of the intestines between the band and the mesentery.1
In the differential diagnosis, Meckel diverticulum should be kept in mind. MDB, which is the remnant of a vitelline artery that perfuses the Meckel Diverticulum, exists in 5% of patients with Meckel Diverticulum. Meckel Diverticulum with symptoms of intestinal obstruction caused by bands like the omphalomesenteric band (remnant of the umbilical intestinal tract) and MBD has been found in childhood.9
CPBs can be found at various locations within the abdominal cavity, with common sites including bands between the ascending colon and terminal ileum, between Treitz's ligament and the terminal ileum, between the right lobe of the liver and the terminal ileum, and between the right lobe of the liver and the ascending colon.10
One of the primary reasons for the uniqueness of CPB-related bowel obstructions is the difficulty in diagnosing them. Diagnosing CPBs is often a process of exclusion, as clinicians need to rule out other common causes of bowel obstruction first. Thus, a careful patient history should be obtained. Additionally, because of their rarity, healthcare providers may not always consider CPBs as a potential cause when a patient presents with symptoms of bowel obstruction especially in the adult population.
A plain abdominal X-ray may show intestinal distension, air-fluid levels, and/or sub-diaphragmatic free air if perforation had occurred,11 but it can be also normal. Abdominal ultrasound could be also utilized and usually demonstrates intestinal loops distention.
A CT scan can identify the location, cause, and severity of obstruction-related complications including ischemia and peritonitis.9
However, because there are no particular imaging tests to identify intestinal obstruction caused by congenital bands, imaging investigations are not conclusive and may delay treatment.9
The final diagnosis usually depends on clinical suspicion followed by surgical exploration which will be both diagnostic and therapeutic intervention.
Concerning the management of a congenital band, surgical treatment is the cornerstone.1 Laparotomy has traditionally been recommended, but with the advent of minimally invasive surgery, laparoscopy has been proposed as an alternative. Wu et al. recently reported that laparoscopy in the diagnosis and treatment of a congenital band may be safe and feasible.3, 12-14 The treatment consists of resecting the band and if necessary, resecting a necrotic small bowel loop.15-17
By reporting this case, we emphasize the importance of considering CPBs in the differential diagnosis of bowel obstruction, particularly when patients lack typical risk factors. Physicians should maintain a broad differential diagnosis to avoid overlooking uncommon etiologies.
4 CONCLUSION
In conclusion, this rare case of SBO due to CPBs underscores the importance of maintaining clinical suspicion for CPBs in adult patients with bowel obstruction, especially when they lack typical risk factors or a history of abdominal surgery, trauma, or clinical hernia. Early surgical intervention, serving both diagnostic and therapeutic purposes, remains essential in managing this condition.
AUTHOR CONTRIBUTIONS
Mouhammed Sleiay: Writing – original draft; writing – review and editing. Bilal Sleiay: Writing – original draft. Douha Albaroudi: Writing – original draft. Hasan Alsmodi: Writing – original draft. Mohammad ali abshi: Writing – original draft. Mohammed Alaswad: Writing – review and editing. Abdulazez Sleiay: Writing – original draft. Osama Arabi: Investigation; supervision.
ACKNOWLEDGMENTS
We hope to thank SMSR Team Lab. for their efforts and bringing our team together.
FUNDING INFORMATION
Not applicable.
CONFLICT OF INTEREST STATEMENT
Not applicable.
ETHICS STATEMENT
Not applicable because all date belong to the authors of this article.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.