Bilateral endogenous Candida albicans endophthalmitis following COVID-19 infection and intravenous antibiotics use: A case report
Abstract
Key Clinical Message
Endogenous fungal endophthalmitis tends to occur in immunocompromised patients, including COVID-19 infection. For high-risk populations, timely tissue biopsy, fungal culture, and susceptibility testing can facilitate early diagnosis and treatment, thereby improving the prognosis.
While endogenous fungal endophthalmitis is a rare condition, its incidence has recently been on the rise. A 48-year-old male presented with complaints of acute visual loss in his right eye for 2 weeks. He had a history of COVID-19 infection, confirmed by a positive nucleic acid test, and was treated with intravenous antibiotics and glucocorticoids a week before the episode. A comprehensive eye examination revealed significant inflammatory cells floating in the anterior chamber and considerable cloudiness in the vitreous of the right eye, while few vitreous cells were visualized in the left eye. After pars plana vitrectomy (PPV) was performed in the right eye, a vitreous biopsy revealed an intravitreal infection of Candida albicans, which was susceptible to fluconazole. Endogenous fungal endophthalmitis occurs in patients with various underlying systemic conditions, such as those with diabetes, organ transplantation recipients, individuals undergoing chemotherapy, users of corticosteroids and immunosuppressants, AIDS patients, and those engaged in intravenous drug use. In high-risk populations associated with intravenous antibiotics, the timely identification of one or more well-defined oval yellow-white chorioretinal lesions, especially in the posterior pole of the retina, can contribute to an early diagnosis through tissue biopsy, fungal culture, and susceptibility testing. This approach enables targeted antifungal therapy, thereby improving the prognosis of visual function for the patient.
1 INTRODUCTION
Endogenous fungal endophthalmitis (EFE), a severe intraocular infection, arises from the hematogenous dissemination of fungi (fungemia). Typical signs of EFE include localized elevated white lesions on the retina or in the vitreous, sub-retinal abscess formation, or retinal detachment (RD) with visible fungal lesions on the retina.1, 2 Despite being rarely diagnosed, the incidence of this fungal infection has shown a recent increase. Early diagnosis and prompt, aggressive treatment are essential to avoid vision loss in patients with EFE.3 In the present clinical case, we reported a case of bilateral endogenous Candida endophthalmitis in a man with good clinical improvement after prompt therapy.
2 CASE PRESENTATION
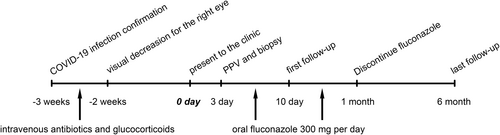
A 48-year-old male presented to our clinic due to a sudden visual decrease accompanied by shadows in his right eye over the past 2 weeks. Figure 1 illustrates the timeline of events, from the onset of symptoms to diagnosis and treatment for this patient. Notably, the patient had recently experienced a confirmed episode of COVID-19 infection, confirmed by positive nucleic acid testing, approximately 1 week before the onset of eye symptoms. During that time, he received treatment with intravenous antibiotics for 5 consecutive days and glucocorticoids for 3 consecutive days at another medical facility.
The patient's best corrected visual acuity (BCVA) was reduced to counting fingers for the right eye and 20/20 for the left eye. Intraocular pressure (IOP) measured 13 mmHg for the right eye and 18 mmHg for the left eye. Slit-lamp examination of the anterior segment of the eyes showed obviously floating cells in the anterior chamber and significant vitritis in the right eye. However, there were no apparent signs of inflammation in the anterior chamber or vitreous cavity of the left eye. Color fundus retinal photography of the right eye revealed a large chorioretinal abscess located in the macular region (Figure 2A). The vitreous cavity of the left eye was transparent, without any inflammatory cells. Importantly, a well-defined oval yellow-white lesion was discernible in the temporal-inferior macular region of the fundus of the left eye. This lesion originated from the choroid and extended into the outer retina (Figure 2B).
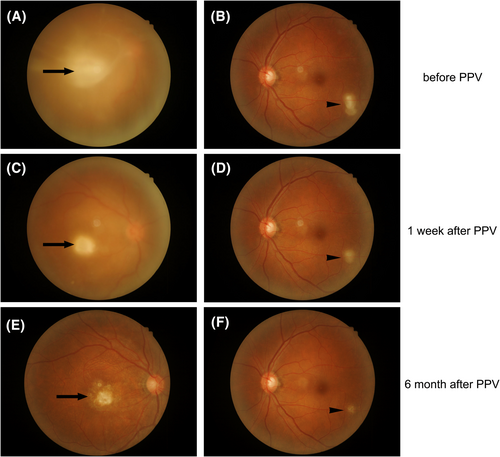
After admission, the patient underwent a thorough systemic examination, which ruled out diabetes and HIV infection. To address the vitreous opacity, restore optical clarity, and establish an accurate diagnosis, the patient underwent pars plana vitrectomy (PPV). During this surgical procedure, vitreous fluid and samples from the yellow-white retinal lesions were collected for bacterial and fungal culture as well as biopsy. Fungal culture and susceptibility testing confirmed the presence of Candida albicans, which was susceptible to fluconazole. Consequently, a diagnosis of endogenous Candida endophthalmitis was established, leading to the initiation of daily oral fluconazole therapy at a dose of 300 mg. One week after the surgery, the opacity in the vitreous cavity of the right eye had significantly reduced (Figure 2C), and the oval yellowish-white lesion on the left eye's retina was gradually decreasing in size (Figure 2D). During the latest follow-up examination conducted 6 months after the surgery, the final BCVA for the right eye had improved to 20/400. Importantly, the vitreous cavity of the right eye had achieved significant transparency, revealing a residual macular scar (Figure 2E). Simultaneously, the retinal lesion in the left eye had shown significant improvement, and no more lesions were observed (Figure 2F). The effectiveness of treatment is more convincing because the retinal lesion in the left eye is also a fungal infection, so the patient's diagnosis is bilateral endogenous C. albicans endophthalmitis.
3 LITERATURE REVIEW AND DISCUSSION
The presented case highlights bilateral fungal endogenous endophthalmitis, which is linked to the intravenous administration of antibiotics and glucocorticoids, along with a history of COVID-19 infection. It's worth noting that the suppression of the immune system due to glucocorticoid use and the broad-spectrum antibiotics seems to have contributed to the development of endogenous endophthalmitis.
Although EFE was once considered a rare condition, its incidence has progressively increased over time. There has been a noticeable surge in related literature published on PubMed since 2001. Various factors, such as the use of glucocorticoids,4 the presence of a central venous catheter,5 extensive burns,6 and COVID-19 infection,7-9 have been associated with immune system suppression and linked to the onset of EFE. Among the causative agents, C. albicans remains a primary contributor to fungal endogenous endophthalmitis, followed by Aspergillus species.10, 11 Recent in vivo research has indicated that systemic Candida albicans infection in mice triggers endogenous endophthalmitis by disrupting the outer blood-retinal barrier (oBRB).12
In previous studies, vitreoretinal findings were classified into stages: Stage I, characterized by chorioretinal changes without extension to the vitreous cavity; Stage II, where a fungal mass penetrates the inner limiting membrane and buds in the vitreous cavity; Stage III, associated with vitreous opacity leading to unclear fundal observation; and Stage IV, marked by the complication of retinal detachment (RD) concurrent with Stage III. This staging framework helps determine the optimal timing for surgical intervention.13 In the present case, the right eye was classified as stage III while the left eye was categorized as stage I. Consequently, a PPV was performed on the right eye, followed by systemic antifungal therapy featuring oral fluconazole administration. For patients with EFE who have not yet developed retinal detachment, that is, patients with EFE before stage IV, it has been reported that intravitreal injection is also an alternative treatment modality, including caspofungin,14 amphotericin B,15 and voriconazole.16
Endogenous fungal endophthalmitis poses a significant threat to ocular health and represents a rare yet serious complication of fungemia. In a recent retrospective case series focusing on EFE,17 diabetes emerged as the foremost risk factor, followed by recent hospitalization, urinary tract disorders, liver disease, and immunosuppressive therapy. Candida spp., notably C. albicans, were identified as the most prevalent fungal isolates. A noteworthy observation is that better initial visual acuity (VA) correlates with improved visual outcomes, highlighting the pivotal role of early diagnosis and aggressive treatment in enhancing vision prognosis.3
4 CONCLUSION
This clinical case emphasizes the importance of considering the diagnosis of EFE as a differential diagnosis of endophthalmitis in immunosuppressed patients such as previous history of COVID infection. It highlights the crucial role of early diagnosis and prompt intervention in preventing severe visual impairment. This underscores the importance of proactive management strategies.
AUTHOR CONTRIBUTIONS
Shuang Wu: Conceptualization; data curation; formal analysis; writing – original draft. Cunbo Wang: Data curation; investigation; writing – original draft. Yanbing Zhang: Writing – original draft.
ACKNOWLEDGMENTS
None declared.
FUNDING INFORMATION
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data underlying this case cannot be shared publicly due to the privacy of individuals who participated in the study.