Management and saving a traumatized poor prognosis maxillary central incisor for 18 years: A patient-centered treatment
Abstract
Key clinical message
With today's increasing desire to preserve natural teeth, managing teeth with a poor prognosis is a new challenge for clinicians. A dentist's attention to patient-centered care is essential, which improves dental outcomes.
Nowadays, patients' interest in preserving their natural teeth has increased. In the patient-centered care model, the clinician should consider the patient's preferences and values in the treatment plan. This strengthens the patient's responsibility toward his own body, resulting in more patient satisfaction and effective cooperation. Therefore, the skill of saving teeth with a poor prognosis, in which there was no other choice but to extract them, becomes essential in patients who want to preserve their natural teeth. This case report presents the successful 18-year treatment and management of a maxillary central incisor of a 17-year-old male with a horizontal root fracture, who was incompletely treated in another medical center when the trauma occurred. The patient presented to us after 6 months. Due to the short length of the root, the patient underwent regenerative endodontic treatment first, but he did not attend follow-ups. Finally, after 8 years, the patient returned with symptoms of infection and periapical radiolucency. The apical part of the root was resorbed during this time. Finally, it was decided to place an apical plug with MTA. MTA was extruded from the apical part of the root canal during the placement of the apical plug. In the 1-, 2-, 4-, and 10-year follow-ups, the patient was completely asymptomatic, and the radiolucent periradicular lesion had healed. However, the extruded MTA was still present in the radiographic images without interfering with the healing process. Finally, the tooth has remained functional for 18 years.
1 INTRODUCTION
Due to the growing desire to preserve natural teeth, a tooth in the poor prognosis category presents a new challenge for dentists. Deciding whether to put a tooth in the hopeless category is not easy, as there is always the possibility of making a mistake. With the proper treatment plan and patient support, teeth with unfavorable prognosis can continue functioning for years.1
During childhood and adolescence, people are prone to traumatic tooth injuries, which cause damage to the tooth and its supporting structures, including root fractures, bone loss, and tooth loss. Horizontal root fracture is caused by direct trauma.2 In adolescents aged 11–20, the most common root fracture occurs in the maxillary central tooth. Root fractures are relatively rare, with a prevalence between 1.2% and 7%.3 In luxation injuries, the neurovascular source of the pulp may be affected in the apical foramen region and at the fracture line. Horizontal root fracture is common between 0.5% and 7% among permanent tooth injuries.4 A horizontal fracture divides the root into two, coronal and apical parts; usually, the apical part is not displaced, the neurovascular bundles in the apical foramen remain undamaged, and the pulp in this part will be normal.5, 6 Also, infectious necrotic pulp can cause external inflammation and root resorption.7
Traditionally, traumatized teeth with horizontal root fractures that had infected necrotic pulp and inflammatory root resorption associated with necrotic pulp were treated with conventional root canal treatment, including chemomechanical debridement of the coronal part of the root canal space, and finally, obturation of the root canal. However, in recent years, regenerative endodontic treatment (RET) has been used to treat horizontal root fracture and resorption.8
RET, a biologically based treatment, is designed to restore the function of damaged and non-functional tissue.9 When the coronal part of the root is short, if the root length is increased with the RET, the problem of the high crown to root ratio can be solved. Several treatment options are available when the RET fails, such as the repeating RET, apical plug with calcium silicate base cement, and root canal treatment according to the present conditions.10
In deciding to choose a treatment plan among the available options, the patient's desire also plays a critical role in addition to the current scientific evidence and the clinician's skill. In 2001, the National Academy of Medicine (NAM) proposed the need for a patient-centered care (PCC) model to improve health outcomes for patients. This model respects and responds to patient preferences, needs, and values, and ensures that patient values guide all clinical decisions.11 It has been stated that these changes will lead to improved patient satisfaction.12 In this view, the clinician must consider the patient's desire in the treatment plan and strengthen the patient's responsibility toward his body and care. The result of this view will be more effective patient participation and cooperation.13 This case report described the long-term successful management of a tooth with an unfavorable prognosis based on a patient-centered approach.
2 CASE PRESENTATION
A 17-year-old male with pain in his Tooth #9 was referred in 2004. The patient's medical history was non-contributory. He reported a history of trauma to the maxilla in the past 6 months and underwent emergency treatment. The patient did not visit his dentist for the next visit. Previous medical centers had advised the patient to extract the tooth. In the clinical examination, the temporary filling of the tooth had fallen out, and the access cavity was filled with food debris and also had caries. There was a longitudinal crack on the buccal surface of the tooth crown, and in addition, the tooth had Grade I mobility. The periapical radiograph shows a horizontal root fracture in the mid-root, the coronal part had undergone pulpectomy, and the apical part was left without treatment. A periapical radiolucency was also evident. Due to the short length of the coronal part of the root and the high crown to root ratio, the questionable prognosis of Tooth #9 was discussed with the patient, but due to the patient's demand, it was decided to perform the treatment. The RET was selected among the available options to increase the root length. At that time, limited reports of successful RET had been published by Iwaya et al.14 and Banch et al.15
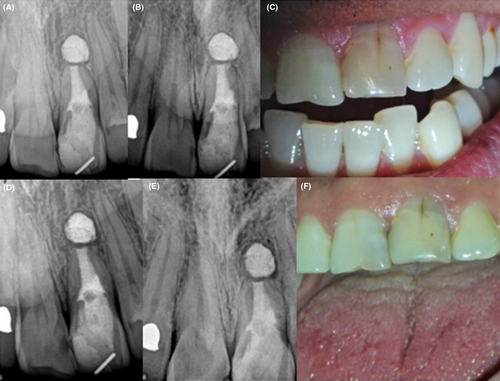
Based on the treatment performed in the studies, as mentioned earlier, a treatment procedure was adopted. In the first visit, anesthesia was applied using 2% lidocaine along with 1/80,000 epinephrine. The tooth was isolated with a rubber dam. Caries were removed, copious irrigation was carried out with 5.25% sodium hypochlorite, and the irrigant was agitated using a K-file #30 (Mani). After the final irrigation with normal saline, the canal was dried with a paper cone. A mixture of ciprofloxacin, metronidazole, and minocycline, as described by Hoshino et al.,16 was mixed with sterile saline. The paste with a creamy consistency was placed inside the root canal using a #40 paste carrier (Lentulo, Dentsply) and sealed coronally with reinforced zinc oxide eugenol cement (Zonaline, Kemdent). Four weeks later, the patient's symptoms resolved. Two percent lidocaine was injected along with 1/80000 epinephrine (Daroopakhsh). The tooth was isolated with a rubber dam, and the temporary filling was removed. The triple antibiotic paste (TAP) was removed from the root canal by copious irrigation. Sodium hypochlorite 5.25% was used as an irrigant, and then the final irrigation was carried out with normal saline. Then, the canal was dried, and apical bleeding was induced with a #40 K-file (Mani). After the blood clot reached the level of the CEJ, ProRoot MTA (Dentsply Tulsa) was placed on it. A wet cotton pellet was placed on the MTA, a temporary filling was made, and a radiograph was taken. One week later, the MTA setting was checked, and the patient was referred to the restorative dentistry specialist (Figure 1).

Unfortunately, the patient did not return for follow-ups. 8 years later, in May 2012, the patient complained of mild pain in the vestibule area of Tooth #9. The pain was evident by palpation on examinations, and Grade I mobility was seen. In the periapical radiograph, a radiolucent lesion was observed around the apex of the tooth. It is unclear whether the periapical lesion has healed and recurred in these 8 years or whether the lesion was present during this period. However, the patient stated that he had no symptoms during this period. Also, the apical part of the root faded entirely and could not be seen in the preapical radiograph. The RET was considered to have failed, again because of patient will, it was decided to perform the apical plug with MTA.
After preparing the access cavity, the tooth was isolated with a rubber dam, and then the MTA was scraped with a D14 ultrasonic tip on an ultrasonic device (NSK). After re-determining the length and, cleaning the canal, and irrigation with 5.25% sodium hypochlorite, the canals were dressed with calcium hydroxide, and temporary filling was performed. A week later, the patient's symptoms were resolved, and after removing the temporary restoration and removing calcium hydroxide with copious irrigation, the apical plug was placed using Root MTA L&S; some MTA extruded beyond the apex during plug placement as a larger mesial part and a minor distal part, finally moist cotton pellet was placed on it, and a temporary filling was made with reinforced ZOE cement (Zonaline, Kemdent). A radiograph was taken at the end of the treatment. Two weeks later, the MTA setting was checked, and the tooth was restored with Fuji II glass ionomer (GC Corporation) and composite resin (Filtek Z250; 3M ESPE). At this time, the extruded MTA was separated from the MTA inside the canal (Figure 2).

The patient had no clinical symptoms in the first-year follow-up, and the periapical lesion had also healed. The larger part of extruded MTA was visible without change, but the smaller distal part was more diluted and faded in the radiographic image. Grade I mobility was still visible, and a longitudinal line of cracks was observed on the buccal surface of the tooth crown. However, the patient did not want to receive esthetic restorative treatments. In the second-year follow-up, the tooth mobility was resolved, and the tooth was completely asymptomatic. In the periapical radiograph view, the larger MTA part was visible without change; the smaller distal part was completely absorbed. The patient had no signs or symptoms in the 4- and 10-year follow-ups. In the 10-year follow-up radiograph, the larger part of MTA was still visible and was surrounded by bone tissue (Figure 3).
3 DISCUSSION
RET has been proposed as a treatment strategy for teeth with necrotic pulp and open apex for several decades. As a result of this treatment, the length and thickness of the root can be increased, and the closure of the apex can occur.15 RET has also been used in teeth with horizontal root fracture or root resorption due to trauma.8 In the case discussed in this article, it was decided to do RET due to the short root length and high crown to root ratio. According to the successful case reports available at that time,14, 15 the treatment procedure is based on the protocol in the previous case reports.
The RET protocol has changed over the years; among other things, an antibiotic solution with a much lower concentration is used due to the toxic effects of TAP on stem cells. Also, sodium hypochlorite was not used in the second visit, and the root canal was irrigated only with 17% EDTA. It is proposed that irrigation with 17% EDTA causes the release of bioactive molecules from the dentine, which increases the survival and differentiation of stem cells. In addition, in today's protocol, in the second visit, the mepivacaine without a vasoconstrictor is used to facilitate bleeding induction.17, 18
Based on the Almutairi et al. review article, several reasons are considered for the failure of RET. Persistent infection is regarded as the main cause of RET failure, followed by fracture, discoloration, and coronal leakage. Twenty-four percent of failure occur in the first year, 24% between the first and second year, and 39% after 2 years showed signs of failure.19 In this case, 8 years after the RET, the patient presented pain sensation by periapical palpation. Also, a radiolucent lesion was observed in the periapical radiograph. The coronal seal had been maintained for these years, since the patient did not return for follow-ups, it cannot be determined whether there was a persistent infection during this period or whether it was healed first and then the symptoms of the infection appeared, but the patient was asymptomatic during this period. It was considered that in many reported cases, failure after RET occurred at least after 2 years; long-term follow-up is one of the requirements of this treatment.
In case of failure of the RET, based on the degree of the apical closure, the thickness of the root canal wall, and the length of the root, the treatment plan can include repeating the RET, apical plug with MTA, and conventional root canal treatment.10 In this case, during the placement of the apical plug, some of the MTA was extruded from the apex, but in the follow-ups, despite the presence of a large part of the extruded material, the patient was asymptomatic, and the periapical lesion was resolved. In several reports, healing of the periapical lesion was observed in the presence of MTA extruded beyond the apex, and it was without significant problems for the patient, probably due to this material's biocompatibility.20-23 Also, in several reports during follow-up, the absorption of extruded MTA has been seen simultaneously with the healing of the lesion. However, it is not a prerequisite for periapical lesion healing.20, 24
When he returned after 8 years, the apical part of the root, which was visible in the periapical radiograph at the first visit, had disappeared during the healing process. In a similar case, the apical part resorption of the root after horizontal root fracture was reported by Abbott et al.25 The cause of this phenomenon is probably the process of inflammation and subsequent repair, which caused the remaining apical part to be resorbed and replaced with bone.
The decision to save or extract a tooth with an unfavorable prognosis depends on various factors. In the cases of tooth extraction, depending on the patient's condition, replacement with an implant is one of the treatment options. Dental implant is the last treatment option; the subsequent treatment plan will be very complicated if it fails. Despite the high success rate of dental implants, there is always the possibility of causing problems such as implant failure, peri-implantitis, and prosthetic restoration problems, while the PDL and PDL sensory network is not present around the implant and cannot precisely reconstruct the conditions of a natural tooth. Therefore, these cases make preserving natural teeth a priority for clinicians.26-28
In this case, due to the patient's age and incomplete maxillary alveolar bone growth, if the tooth was extracted, it was impossible to place the implant until bone development was complete.29 Alveolar ridge resorption could be expected at the extraction site during this period, which made it difficult to place the implant and make a suitable restoration. The treatment performed on this tooth with a poor prognosis caused the patient's tooth to remain functional for 18 years, and the patient's esthetic concerns were addressed. In addition, according to the patient's request, no further restorative intervention was performed to cover the longitudinal crack on the buccal surface.
With the introduction of bioceramic cements and many successful reports on their use in RET, repair of root perforations, and their use as an apical barrier, due to the biocompatibility and bioactivity of these materials, today it is possible to save many teeth.30 It seems that with new treatment options and dental materials, the criteria for deciding whether to save or extract a tooth should be reconsidered.
According to the UK Institute of Medicine definition, PCC means respecting and responding to the patient's preferences, needs, and values and ensuring that the patient's values guide all clinical decisions. In this view, the patient is at the forefront of decision-making and treatment, and the result is the improvement of the physical and mental consequences of the treatment. Although PCC is well-defined and well-comprehended in the field of medicine but in the field of dentistry, specific and standard criteria still need to be defined for it.13 PCC contains a wide range of the most basic principles, including the need to behave with dignity, kindness, compassion, politeness, respect, perception, honesty, and patient's active participation in making decisions about the treatment plan and receiving care that cover the patient's demands and preferences.31
According to Azarpazhooh et al. study, most patients with symptomatic apical periodontitis prefer to save their teeth with root canal treatment instead of tooth extraction and replacement with a dental implant.32 Another study also found that most patients with apical periodontitis tend to participate in decision-making and treatment planning, indicating that the PCC model is now preferred over paternalistic approaches.33 In this case, even though the described tooth had an unfavorable prognosis, focusing on the demands of the patient and his parents to preserve the tooth along with informing him of the condition of the tooth and involving the patient to be responsible for the selected treatment plan for his tooth has increased his cooperation and responsibility. A person who had left the tooth, as mentioned earlier, with an open access cavity and without restoration for several months in the initial visit, after recognizing the value and need to preserve the mentioned tooth, became diligent in taking care of it.
As a result, a tooth with an unfavorable prognosis has remained functional for nearly 18 years, which highlights the message that increasing attention to PCC in dental treatments is essential, improving the outcomes of dental treatments and patient satisfaction. The development of endodontic treatments has improved patients' quality of life by affecting various variables such as functional limitations, physical pain, and psychological stress. It allows the clinicians to consider the patients' perceptions and preferences, as well as the prognosis and outcomes.34
4 CONCLUSION
New treatment strategies and clinician skills combined with the PCC approach can allow teeth with a poor prognosis to remain an active component in the dental system for a long time. It is suggested to revise guidelines emphasizing PCC regarding preserving or extracting teeth with unfavorable prognoses.
AUTHOR CONTRIBUTIONS
Mohsen Aminsobhani: Conceptualization; data curation; methodology; project administration; writing – review and editing. Kimia Hafezi Motlagh: Methodology; writing – original draft; writing – review and editing. Reza MahjourianQomi: Investigation; methodology; writing – original draft; writing – review and editing.
ACKNOWLEDGMENTS
The authors thank the patient for consenting to the case's publication.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted without any commercial or financial relationships construed as a potential conflict of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.