IL-8 and IL-1β in the Cerebrospinal Fluid of Patient With Creutzfeldt-Jakob Disease: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
Inflammatory cytokines play a crucial role in Creutzfeldt-jakob disease (CJD). We examined inflammatory cytokine levels in both blood and CSF in a CJD patient and an epileptic encephalopathy as a control case. Results showed that IL-6, IL-8, IL-1β, and TNF-α levels were elevated in blood, but only IL-8 and IL-1β levels, especially IL-8, were significantly elevated in Cerebrospinal fluid (CSF). This suggests that IL-8 and IL-1β are closely related to cognitive impairment and blood–brain barrier (BBB) damage in CJD, and IL-8 might be a key target in early cognitive impairment in CJD.
Summary
- We report IL-8 and IL-1β levels elevated in Cerebrospinal fluid (CSF) in a Creutzfeldt-jakob disease (CJD) patient who is an 83-year-old female with a 5-month history of cognitive impairment, suggesting that IL-8 and IL-1β are closely related to cognitive impairment and BBB damage of CJD and may serve as an early biomarker.
1 Introduction
Creutzfeldt-Jakob disease (CJD) is an extremely rare neurodegenerative disease. With an average life expectancy of about 6 ± 4 months, about 70% of CJD patients begin with rapidly progressive dementia [1]. Numerous studies have shown that microglia are activated by prion proteins (PrPsc) in CJD and produce cytokines such as IL-8, IL-1β, IL-10, etc. [2, 3]. These inflammatory cytokines are related to progressive dementia in patients with CJD and play an important role in the Blood-Brain Barrier (BBB) impairment and apoptosis of neuronal cells [1, 4, 5]. Importantly, inflammatory cytokines overexpression is also found in neurodegenerative disease [6, 7]. They contribute to astroglial proliferation and astrogliosis, and inflammatory reactions lead to synaptic atrophy and eventually neuronal cell death [8]. These pathological changes are a direct contributor to cognitive decline in neurodegenerative diseases including CJD [9].
Although several data have indicated that inflammatory cytokines play a crucial role in CJD, most of these studies have been conducted on animals, and it is not clear enough the levels and effects of different cytokines, especially CSF, in human patients with CJD. To further determine the levels of expression of different cytokines in CJD we examined inflammatory cytokine levels in both blood and CSF in a CJD patient, and an epileptic encephalopathy patient's CSF and blood are examined as the control case.
2 Case Presentation
2.1 Case 1
An 83-year-old female complained of a 5-month history of cognitive difficulty, and she had no previous history of cognitive impairment before the onset of illness. In the last 5 months, the patient gradually developed ataxia of both lower limbs and rapidly developed hypomnesia, and the cognitive difficulty was significantly aggravated. On physical examination, cognitive function declined, both eyes stared to the right, the left eye abduction was limited, and hypermyotonia of the upper extremities and ataxia of both lower limbswere presented.
2.2 Investigations and Results
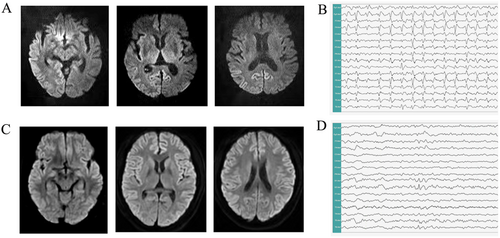
The DWI MRI scan shows that prominent diffusion restriction along the cortical ribbon (Figure 1A), and V-EEG indicates periodic release of sharp and three-phase waves (Figure 1B). Subsequently, the most important marker 14–3-3 protein showed positive in CSF. Finally, the patient was diagnosed with Probable CJD [10]. Firstly, we examined the CSF albumin and blood albumin of the patient (Table 1). Then, the different inflammatory cytokines in the CSF and blood of the patient were examined (Table 2).
| CSF (pg/mL) | Blood (pg/mL) | Reference values (pg/mL) | |||
|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 1 | Case 2 | ||
| IL-6 | 1.25 | 2.48 | 12.20** | 1.20 | 0–3.4 |
| IL-8 | 51.90* | 48.60 | 31.70** | 4.20 | 0–14 |
| TNF-α | 5.02 | 6.04 | 14.40** | 3.50 | 0–9.1 |
| IL-10 | 4.50 | 4.20 | 3.70 | 3.90 | 0–9.1 |
| IL-1β | 8.89** | 5.40 | 8.36** | 3.60 | 0–5 |
- * p < 0.05.
- ** p < 0.01 vs. Case 2.
2.3 Case 2
A 20-year-old male was diagnosed with epileptic encephalopathy for more than 15 years. His mother had a history of uterine bleeding when she gave birth to him. At the age of six, he was unable to speak, his intelligence performance gradually declined, and his memory and comprehension were significantly worse compared with those of the same age. In the last 1 year, seizures occurred 1–2 times per month despite treatment with anti-epileptic drugs. On physical examination, speech ability and comprehension were notably declined.
2.4 Investigations and Results
The DWI MRI scan shows that bilateral temporal lobe mild atrophy (Figure 1C); the V-EEG mainly shows the presence of slow and sharp waves (Figure 1D). Then, the patient's CSF and blood were examined for albumin and inflammatory cytokines (Tables 1 and 2).
3 Discussion
CJD is a rare neurodegenerative disease that presents with the rapid progression of cognitive dysfunction, ataxia, myoclonus, and death in less than 1 year. Early cognitive impairment is a prominent clinical feature, in which neuroinflammation plays a key role and elevated inflammatory factors accelerate cognitive impairment [11]. Our cases showed that IL-6, IL-8, IL-1β, and TNF-α levels were elevated in blood in the patient with CJD, but only IL-8 and IL-1β levels, especially IL-8, were significantly elevated in CSF.
IL-8 is a chemokine associated with immune response properties [12]. Several studies have shown that IL-8 levels are significantly higher compared to other inflammatory cytokines like IL-6, IL-1β, and TNF-α in various dementia diseases, such as Alzheimer's disease and vascular dementia et al. [6, 13]. Our cases also have shown that IL-8 levels obviously increased in the CSF of the CJD patient and the epileptic encephalopathy patient. In addition, IL-8 is significantly higher in the CSF of the CJD patient compared with the epileptic encephalopathy patient, which is roughly normal in the blood of the epileptic encephalopathy patient. Statistical analysis showed a marked difference in two cases (p < 0.05), which is different from a previous study [6]. Previous studies have shown that during the early stages of CJD, microglia are stimulated to secrete IL-8, and the action of IL-8 leads to apoptosis of neuronal cells, resulting in cognitive impairment [1]. Based on these results, we presume that IL-8 might be associated with the severity of cognitive impairment and suggest that IL-8 is the most sensitive inflammatory cytokine in the early stages of the inflammatory pathological reaction in CJD. Meanwhile, our cases have shown that IL-1β levels elevated in the CSF both in the CJD patient and the epileptic encephalopathy patient, but they were normal in the blood of the epileptic encephalopathy patient. Numerous studies have shown IL-1β could increase BBB permeability and participate in processes of cognition, learning, and memory [14]. In Table 1, results also showed that the C/B albumin index in the CJD patient is higher compared with the epileptic encephalopathy patient, indicating the BBB impairment. We considered that these results indicated that there is more obvious BBB damage in CJD than in the epileptic encephalopathy patient [15].
4 Conclusion
In summary, our observations showed that the levels of IL-8 and IL-1β notably increased in the CSF of CJD patients, suggesting that these two cytokines are closely related to cognitive impairment and BBB damage in CJD. Particularly, IL-8 might be a key target in early cognitive impairment in CJD. Furthermore, more studies are needed to study the role of these inflammatory factors in cognitive impairment in CJD.
Author Contributions
Liu GuoYan: data curation, writing – original draft. Zhan ShuQin: investigation. Qu HuiYang: data curation, investigation. Chen MengYing: formal analysis, writing – original draft. Ren HongWei: investigation, writing – original draft. Sun Hong: writing – review and editing.
Acknowledgments
We would like to thank the patients for their consent to this case report.
Consent
Written consent was received from patients prior to the publishing of this case report and its related photographs.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.