Neuropsychological Aspects of a Patient With Intracranial Rosai-Dorfman Disease: Case Report
Funding: The authors received no specific funding for this work.
This study was conducted by the Psychology Department of Pontifícia Universidade Católica do Rio de Janeiro (PUC-Rio).
ABSTRACT
Intracranial Rosai-Dorfman disease (RDD) is rarely reported in the literature. Up to the present date, there are no documented studies regarding the neuropsychological aspects of a patient with this diagnosis. This study fills this gap, reporting a case of a patient with petroclival RDD, emphasizing the importance of cognitive investigation.
1 Introduction
Rosai-Dorfman Disease (RDD) is a rare, benign, and idiopathic lymphoproliferative disorder. It predominantly affects males, and its etiology remains elusive [1-3]. In rare instances, 5% of the cases [4], RDD involves the central nervous system (CNS) without displaying the typical clinical features of the disease. Although RDD cases in the CNS have been reported, petroclival RDD is extremely rare [4], with only eight cases documented in the published research [4] and no reference to cognitive outcomes. Therefore, the present study intends to pave the way in the scientific literature for neuropsychological investigation in cases of intracranial RDD.
This condition can present with various symptoms, including headache, seizures, numbness, plegia, cognitive and cranial nerve deficits, and visual disturbances, contingent upon the location of the lesion [2, 3]. This variability in presentation often overlaps with other intracranial pathologies, particularly brain tumors, such as meningiomas, which share significant radiological similarities [5].
RDD lesions in the central nervous system (CNS) typically present as well-circumscribed dural masses with dural tails on imaging, closely resembling meningiomas [5, 6]. Additional imaging features, such as homogeneous enhancement on MRI and hypovascularization on cerebral angiography, further complicate the differentiation [6]. Accurate differential diagnosis is crucial, as treatment strategies for RDD may differ from those for meningiomas, often involving chemotherapy or radiotherapy in addition to surgical resection [6].
Brain tumors can cause cognitive, sensory, and motor deficits depending on the affected brain regions [7]. To address cognitive issues, neuropsychological assessments play a fundamental role. These evaluations are valuable tools for identifying preserved and impaired cognitive functions, aiding surgical planning, and supporting intraoperative decision-making by pinpointing critical brain areas to avoid. Additionally, they contribute to minimizing cognitive impairments, preserving essential functions, and guiding the entire rehabilitation process [8-11].
Beyond the surgical context, neuropsychological assessments address cognitive symptoms, helping maintain or improve patients' quality of life and supporting effective daily functioning. They also assist in managing concomitant issues, such as behavioral disturbances and depression, thereby enhancing overall well-being [12, 13].
Although numerous studies have documented cognitive outcomes in patients with meningiomas [14-17] no articles specifically address cognitive outcomes of petroclival meningiomas, which likely share similarities with the present case. Existing research on petroclival meningiomas primarily focuses on surgical, neurological, and functional outcomes [18-20]. Nevertheless, a few studies explore the cognitive aspects of skull base and posterior fossa tumors [8, 15, 21].
In summary, as mentioned above, to date, no reports in the literature describe neuropsychological findings in patients with intracranial RDD. Thus, the objective of this study is to contribute to the scientific understanding of this condition by presenting a case report based on the neuropsychological aspects of a patient with a petroclival lesion, hoping that the present study will encourage more researchers to explore the cognitive context of patients with intracranial RDD in greater depth.
2 Case History/Examination
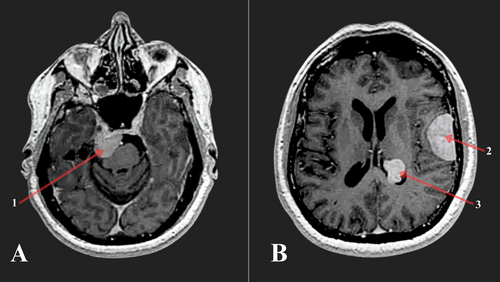
The patient is a 63-year-old right-handed male with 12 years of education, formerly a taxi driver. His medical history dates back to January 2020 when he was initially admitted to the hospital with complaints of a progressively worsening headache unresponsive to analgesics, accompanied by dysarthria. Magnetic Resonance Imaging (MRI) (Figure 1) revealed multiple extraaxial brain lesions located in the right petroclival, left ventricular atrium, and left opercular regions, along with significant edema associated with the opercular lesion (convexity). Subsequently, in February 2020, the patient underwent surgical excision of the opercular mass via left frontotemporoparietal craniotomy. He was discharged from the hospital in good general condition, without apparent deficits, and without any ongoing complaints. The histopathological examination confirmed the diagnosis of RDD. During this period, no neuropsychological evaluation was conducted.
In September 2021, the patient returned to the institution presenting symptoms including left eyelid ptosis, dysphagia, diplopia, memory, and emotional complaints. He also reported more intense drowsiness in the month prior to hospitalization.
After case discussion, the neurosurgical team decided to address the petroclival mass via right retrosigmoid approach. During the preoperative phase, a neuropsychological assessment was performed with the aim of conducting a follow-up evaluation 3 months postneurosurgery.
Following neurosurgery, the patient developed peripheral facial palsy on the right side, abducens paresis, and dysphagia, with minimal improvement. Upon discharge, he was prescribed an anticonvulsant and corticosteroid. At the postsurgical neuropsychological evaluation 3 months later, the patient continued to exhibit these symptoms, along with difficulty hearing in the right ear and mild dizziness.
3 Methods
A battery of neuropsychological tests and standardized scales (Table 1) [22-33] was designed to evaluate verbal and visuo-spatial episodic memory, language, attention, executive functions, visuoconstruction abilities, working memory, and processing speed. Additionally, two inventories were administered to assess the patient's mood.
| Neuropsychological functions | Z score, pre-evaluation | Z score, postevaluation | Z score, difference | ||
|---|---|---|---|---|---|
| Global cognitive functioning | Mini-mental state examination (MMSE-30) [22-24] | −0.48 | −0.88 | −0.40 | |
| Attention and executive functions | Wechsler adult intelligence scale (WAIS-III) [25] |
|
−0.33 | 0.00 | 0.33 |
|
0.00 | 0.00 | 0.00 | ||
|
−0.33 | −0.66 | −0.33 | ||
|
−0.33 | −0.33 | 0.00 | ||
|
−0.33 | −0.53 | −0.20 | ||
| Wechsler abbreviated scale of intelligence (WASI) [26] |
|
−0.33 | −0.66 | −0.33 | |
| Clock drawing test [23, 24, 27] | −4.27 a | −3.36 a | 0.91 | ||
| Rey complex figure test (copy) [28] | −1.18 | −2.57 a | −1.39 | ||
| Verbal fluency Test (FAS form) [29] | −1.58 a | −0.16 | 1.42 | ||
| Memory (episodic and semantic) | Rey auditory- verbal learning test (RAVLT) [30] |
|
−3.03 a | −0.53 | 2.50 a |
|
−2.88 a | −2.88 a | 0.00 | ||
|
−2.46 a | −3.23 a | −0.77 | ||
|
−0.89 | −2.74 a | −1.85 a | ||
|
2.04 a | −2.13 a | −4.17 a | ||
| Figure memory test (FMT) [23, 24] |
|
−1.81 a | −1.81 a | 0.00 | |
|
−1.06 | −3.32 a | −2.26 a | ||
|
0.31 | −3.14 a | −3.45 a | ||
| Rey complex figure test (5 min. recall) [28] | −1.31 | −1.55 a | −0.24 | ||
| Verbal fluency test (animals form) [23, 24] | −0.88 | 0.65 | 1.53 a | ||
| Language | Figure memory test [23, 24] |
|
0.27 | 0.27 | 0.00 |
| Verbal fluency Test (FAS form) [29] | −1.58 a | −0.16 | 1.42 | ||
| Verbal fluency Test (animals form) [23, 24] | −0.88 | 0.65 | 1.53 a | ||
| Visuoconstruction | Rey Complex Figure Test (copy) [28] | −1.18 | −2.57 a | −1.39 | |
| Clock Drawing Test [23, 24, 27] | −4.27 a | −3.36a | 0.91 | ||
| Emotional aspects | Geriatric Depression Scale (GDS – 15) [31, 32] | −1.70 a | −3.03 a | −1.33 | |
| Beck depression inventory (BDI – II) [33] | 0.75 | 0.87 | 0.12 |
- Note: The bold values in Table 1 were used for visual emphasis only and do not reflect statistical significance, as no inferential analysis was performed for these variables. It simply indicates that any z-score equal to or greater than 1.5 standard deviations reflects cognitive impairment.
- a Z Score indicate impairment ≥|1.50| standard deviation.
The results are illustrated through both Raw and Z scores.
Initially, the subject's performance on the tests was compared to normative data. This approach allowed for an exploratory analysis of his cognitive functioning at each testing moment, incorporating qualitative observations in specific cases.
For more elaborate analyses, an intragroup comparison was conducted. It concerned identifying significant and meaningful differences between the initial test application and the subsequent evaluation following the neurosurgical intervention. To investigate these differences, we employed paired t-test models, aiming to identify any significant variations contingent upon the timing of application. Given the inherent limitations of inferential statistics in studies with only one participant, we also evaluated the magnitude of pre- and postdifferences through Cohen's D as an effect size measure. We set the threshold for statistical significance at a p-value of < 0.05.
The proposal to use the paired t-test was intended to complement effect size measurements and visual analyses, providing an additional perspective on the behavior of the data at different assessment points (pre- and postintervention).
This study was approved by the Ethics Committee (CAAE 42541521.5.1001.5279) and informed written consent was obtained from the patient.
4 Conclusion and Results
Regarding the assessment process, in both test application moments, emotional lability and a depressed mood were observed. Nonetheless, the patient exhibited high levels of cooperation and demonstrated a strong interest in completing the assigned tasks.
The results are shown in Table 1. The patient's performance before neurosurgery falls within the average range (normative data) in global cognitive measure, visuospatial memory, semantic verbal fluency (animals), naming, processing speed, working memory, and cold executive functions (Rey Figure Copy) [28]. In contrast, difficulties are observed in verbal episodic memory (RAVLT) [30], visuoconstructive abilities (Clock Drawing Test) [23, 24, 27], attention, and phonemic verbal fluency. His mood was also markedly lowered, with Z scores indicating mild to moderate depressive symptoms.
Analyzing his performance after neurosurgery, notable changes were observed (Table 1). First, a decline was observed in executive functions, visuoconstruction, and mood (GDS-15) [31, 32]. Visuospatial memory in the Figure Memory Test (FMT) [23, 24] which was not impaired before the surgery, exhibited a considerable deficit compared to normative data and pre-evaluation (delayed recall Z score difference = −2.26; recognition Z score difference = −3.45), as well as recognition (Z score difference = −1.85) and forgetting speed (Z score difference = −4.17) of verbal episodic memory in RAVLT [15]. Delayed recall of RAVLT was lower in both pre (Z score = −2.46) and post (Z score = −3.23) assessments. These processes demonstrate difficulty in the storage and recall stages of information after surgery. Conversely, verbal episodic immediate memory (RAVLT Total Score) showed significant improvement (Pre Z score = −3.03; Post Z score = −0.53), indicating an enhancement in the information encoding process, which is mediated by attention. Similar to the encoding process, semantic and phonemic verbal fluency also demonstrated remarkable progress. Furthermore, results remained within the average range for naming, processing speed index, working memory, and global cognitive measure (MMSE) [22-24].
Calculating the significance and relevance of the differences between the pre- and postsurgical assessments, well observed in Table 2, it can be noted that only two measures showed significant (p < 0.05) results: immediate verbal memory (RAVLT) and mood (GDS-15). One of the measures of verbal episodic memory (RAVLT total score) demonstrated a significant improvement after the surgery. In the precondition, Z scores across all sections of the RAVLT test revealed lower results, indicating difficulties across all stages of verbal episodic memory (encoding, storage, and recall). In the postcondition, a notable improvement was observed in immediate memory (encoding process = Total Score), with Z scores falling within the expected range, indicating a better performance compared to the pre-evaluation (p = 0.003). The effect size was substantial and remarkable (Cohen's D = −1.66). Regarding the patient's mood, in both inventories, he exhibited depressive symptoms. In the BDI-II [33], his score indicates mild depression during both instances of assessment. In the GDS-15 [31, 32], his score suggests moderate symptoms before the intervention and severe symptoms after the intervention, with a significant difference (p = 0.041) and a moderate effect (Cohen's D = −0.66).
| Instrument | Raw score (Pre) | Raw score (Post) | T test | p | Cohen's d |
|---|---|---|---|---|---|
| MMSE-30 | 25 | 24 | 2.10 | 0.716 | 0.06 |
| Naming (FMT) | 10 | 10 | — | 1.000 | 0.00 |
| Incidental memory (FMT) | 7 | 3 | 2.26 | 0.104 | 1.21 |
| Immediate memory (FMT) | 6 | 5 | 2.26 | 0.726 | 0.20 |
| Learning (FMT) | 6 | 6 | — | 1.000 | 0.00 |
| Delayed recall (FMT) | 6 | 2 | 2.26 | 0.796 | 0.41 |
| Number-letters series (WAIS-III) | 6 | 6 | 4.30 | 1.000 | 0.00 |
| Digit span (WAIS-III) | 13 | 11 | 2.31 | 0.169 | 0.29 |
| Symbol search (WAIS-III) | 11 | 14 | 2.14 | 0.189 | −0.53 |
| Matrice reasoning (WASI) | 20 | 16 | 2.04 | 0.292 | 0.25 |
| Total score (RAVLT) | 21 | 40 | 2.78 | 0.003 a | −1.66 |
| Rey complex figure test (copy) | 23 | 15 | 2.11 | 0.060 | 0.61 |
| Rey complex figure test (recall) | 4 | 2.5 | 2.11 | 0.260 | 0.34 |
| GDS-15 | 8 | 12 | 2.14 | 0.041 a | −0.56 |
| BDI-II | 15 | 16 | 2.09 | 0.748 | −0.06 |
- Note: The bold values indicate an inferencial analysis conducted with a paired t test, the significance is set at p ≤ 0.05.
- a The significance threshold for the p-value is set at ≤ 0.05.
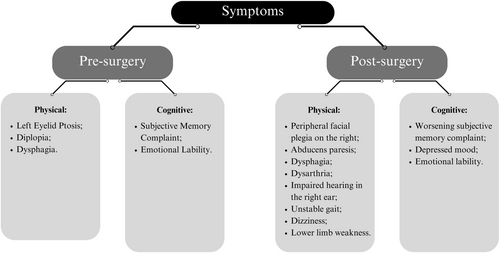
In addition to cognitive findings, Figure 2 illustrates the symptoms reported by the patient pre- and postsurgery. These cognitive, neurological, and behavioral difficulties led to mild dependency in some activities of daily living. It became essential for him to be always accompanied when leaving the house due to visual and auditory impairments, as well as persistent dizziness and unstable gait.
The present study delineated the patient's neuropsychological profile, comparing pre- and postsurgery assessments. This investigation addresses a critical gap in the literature, given the absence of neuropsychological reports on petroclival tumors and intracranial RDD. The findings contribute to understanding the unique characteristics of this condition and pave the way for developing medium- to long-term intervention strategies.
5 Discussion
Multiple intracranial RDD is extremely rare [34]. Conducting a search in the scientific literature on the disease, none of the articles found addressed neuropsychological aspects. This already justifies the significance and relevance of this report. Furthermore, to the best of our knowledge, only 8 cases of petroclival RDD have been reported so far [4], which makes this case report even more pertinent. The resection of a mass in the petroclival area is quite challenging and associated with a high risk of neurological deficits due to its highly vascularized area, surrounded by cranial nerves, and its compression and adhesion to the brainstem [18, 35].
It is common for intracranial RDD to be confused with meningiomas in MRI [4-6, 34] due to characteristics of the lesions on the imaging exam. Brain tumors in the skull base, like petroclival meningiomas, frequently cause complaints such as headache, seizure, weakness, dizziness, cranial nerve deficit, cognitive decline, focal neurological deficit, emotional, and behavioral changes [36]. Before the resection of the petroclival mass, our patient presented with dysphagia, diplopia, left eyelid ptosis, and memory and mood complaints. These clinical manifestations were also observed in a case study reported by Nobrega et al. [3] in a patient with intracranial RDD.
Still concerning clinical symptoms, after the resection of the lesion, our patient retained some deficits and also acquired some additional ones. There are studies in the literature of patients with petroclival tumors who also underwent resection via the retrosigmoid approach and also experienced facial paralysis, hearing loss, dizziness, and other manifestations similar to our patient after neurosurgery [19, 35]. These symptoms occur precisely due to the challenges posed by the tumor's location, affecting cranial nerves, vascularization, and cognition. Studies on patients with petroclival meningiomas also frequently describe hearing loss, dizziness, and imbalance as consequences of cranial nerve impairment [18, 37].
The neuropsychological assessment in patients with brain tumors aims to evaluate the nature and extent of cognitive deficits, guiding treatment and minimizing potential future consequences [8, 38]. Cognitive deficits can be attributed to various factors, including tumor duration and location, brain edema, and the concomitant neuroinflammation [39]. Furthermore, cognitive impairment can be influenced by treatment approach, such as surgery, chemotherapy, and radiotherapy [40].
As shown in Table 3, in accordance with the results of the presurgical neuropsychological assessment of the patient, deficits were evident in verbal episodic memory, attention, visuoconstruction, phonemic verbal fluency, and mood. These deficits can be attributed to the two lesions that remained in the patient's brain (petroclival and ventricular atrium region), in addition to potential sequelae from the removal of the opercular mass (frontal lobe convexity) the previous year. The petroclival region lies in the skull base, where patients with meningiomas often exhibit significantly lower performance in verbal memory compared to those with convexity meningiomas [14]. Additionally, the mass effect on the brainstem and prepontine cistern compression likely contributed to impairments in attention, thereby compromising verbal fluency. The unresolved lesion in the left ventricular atrium, located in close proximity to structures of the limbic system, may further contribute to the observed memory impairment. Furthermore, the presence of depressive symptoms, which were evident in both pre- and postsurgical evaluations, may exacerbate these cognitive deficits [41].
| Neuropsychological functions | Pre-evaluation | Postevaluation | |||
|---|---|---|---|---|---|
| Preserved functions | Compromised functions | Preserved functions | Compromised functions | ||
| Global cognitive functioning | ✓ | ✓ | |||
| Attention and executive functions | Cold executive functions | ✓ | ✓ | ||
| Hot executive functions (Emotional Lability) | ✓ | ✓ | |||
| Attention | ✓ | ✓ | |||
| Memory (episodic and semantic) | Encoding | ✓ | ✓ | ||
| Storage | ✓ | ✓ | |||
| Delayed recall (Auditory-verbal episodic) | ✓ | ✓ | |||
| Delayed recall (Visuospatial episodic) | ✓ | ✓ | |||
| Semantic memory | ✓ | ✓ | |||
| Language | Naming | ✓ | ✓ | ||
| Phonemic oral production | ✓ | ✓ | |||
| Semantic oral production | ✓ | ✓ | |||
| Visuoconstruction | ✓ | ✓ | |||
| Emotional aspects | Depressed mood | ✓ | ✓ | ||
As mentioned above, extraaxial lesions such as our patient's RDD can be easily confused with meningiomas [4, 34]. According to a systematic review in patients with meningiomas, it is quite common to observe cognitive impairment before surgical resection of the tumor, particularly in memory, attention, and executive functioning [15] as well as after neurosurgery [39, 42]. Another point regarding studies on tumors in general, including meningiomas, is that most of them lack baseline preoperative neurocognitive assessments [43]. This limitation hinders our ability to compare findings with previous studies, making it more challenging to draw more accurate conclusions about our results.
Taking into consideration the postoperative aspect, patients with extraaxial benign brain tumors, such as this case, may exhibit improvement in certain cognitive aspects [44] 6 months postsurgical resection [16]. In the present study, the postsurgical assessment took place 3 months following the surgery, revealing a decline, conversely, in cognition. An impairment in cognitive domains after surgery, with no consistent results, was also related by a systematic review with meningioma patients [15]. Our patient exhibited below-expected outcomes in verbal and visuospatial memory, visuoconstruction, and executive functions, well observed in Table 3. Some studies report cognitive decline in these domains following surgical intervention [15, 42] even noting a higher correlation between preoperative edema and worsened cognitive functioning postsurgery [17]. Despite these deficits, our patient presented a significant (p = 0.03) improvement in the postsurgical assessment at the encoding stage of RAVLT [30] (immediate memory-‘Total Score’), but not in the storage and recall stages of information. Thus, it is possible that there has been an improvement in his attentional process following mass removal. This phenomenon can be attributed to the removal of the mass itself and to the decrease in edema following the removal of the lesion [11]. The same improvement in attention postsurgery was also related by Steinvorth et al. [21] with skull base meningioma patients. Attention, as a diffuse cognitive function, can be impaired in the presence of brain edema [43]. The attention domain permeates the information encoding process and also plays a role, along with language skills and executive functions, in verbal fluency tasks, which in our patient's case, had a great improvement in the post op [16].
The patient's latest lesion, which was not surgically addressed, is located in the left ventricular atrium region, in close proximity to the fornix. The fornix, in turn, has a direct connection with the hippocampus, which could explain the patient's difficulty in verbal episodic memory that persisted in both assessment periods.
Evidence shows that most patients with intracranial tumors have emotional and/or behavioral changes [38, 41]. Depressive symptoms were identified in both pre- and postsurgical evaluations; however, in the postassessment, the symptoms worsened, maybe attributable to some physical and neurological sequelae that persisted postsurgery [40].
Impairment in cognitive function may impact an individual's intellectual abilities, daily activities, social relationships, as well as their educational and professional endeavors [29]. Identifying and addressing cognitive dysfunction in patients with intracranial RDD is crucial considering the ongoing advancements in treatment modalities, which have led to an increased life expectancy and managed morbidity for these individuals.
The present case highlights how neuropsychological assessment is a critical component in the comprehensive management of brain lesions—whether common or rare, such as intracranial Rosai-Dorfman Disease (RDD). Regardless of the etiology or prevalence of the condition, any brain lesion may result in cognitive and emotional alterations that significantly affect patients' quality of life and functional independence. Therefore, cognitive evaluation should be regarded as a standard element in the diagnostic and therapeutic process. In rare disorders like RDD, neuropsychological assessments are also essential to identify specific cognitive-behavioral patterns, support differential diagnosis, guide surgical planning, and define individualized rehabilitation strategies. Moreover, they can reveal subtle deficits not always captured through neurological or imaging evaluations.
Given the clinical complexity and rarity of intracranial RDD, structured neuropsychological follow-up is highly recommended. This should involve periodic cognitive and emotional monitoring to capture disease progression, treatment effects, and neuroplastic changes over time. Interdisciplinary collaboration—among neurosurgeons, neurologists, neuropsychologists, and rehabilitation professionals—is essential to ensure a holistic approach. Follow-up care should also include support for emotional well-being and functional autonomy, with timely referral to psychotherapy, physiotherapy, or occupational therapy when needed. A longitudinal approach may also contribute to the scientific understanding of rare intracranial conditions and the development of targeted care strategies.
Some limitations of this study stem from our inability to trace the neuropsychological progression of the patient since the initial hospitalization with the resection of the first lesion (left opercular), precluding a direct comparison with the second admission and removal of the second mass (right petroclival). Nevertheless, we intend to maintain longitudinal monitoring, primarily due to the presence of a residual lesion. It is also important to highlight that inferential analyses were conducted using tests designed for group comparisons, which may introduce discrepancies and reduce result reliability when applied to a single subject. For this reason, the inferential results cannot be generalized beyond the analyzed case. The intention is not to achieve statistical generalization but rather to identify consistent indications of change.
For the future, it is crucial for the researchers to conduct and report additional longitudinal studies or multicase reports investigating the neuropsychological aspects of intracranial RDD, which could validate our findings and further enhance the scientific knowledge in this field. Future case reports similar to this one may enable further comparisons and, consequently, lead to more robust conclusions, offering valuable insights for managing patients with this rare condition.
Author Contributions
Carolina Veras: conceptualization, data curation, formal analysis, investigation, methodology, writing – original draft, writing – review and editing. Danielle Soares de Oliveira: data curation, formal analysis, investigation, methodology, resources. Samara Rufino Zampil dos Santos: data curation, formal analysis, resources, validation. Luiz Felipe Lobo Ferreira: data curation, resources, validation. César Augusto Ferreira Alves Filho: resources, supervision, validation, visualization. Bruno Alexandre Côrtes: resources, supervision, validation. Helenice Charchat-Fichman: conceptualization, project administration, supervision, validation, writing – review and editing.
Acknowledgments
We thank the patient who agreed to share data from his medical record and signed a consent for publication about his case.
Ethics Statement
This study was approved by the ethical committee (CAAE 42541521.5.1001.5279) and informed written consent was obtained from the patient.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.