Severe Actinomycotic Discitis Osteomyelitis and Bacteremia in an Immunocompetent Adult Following Dental Cleaning: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
Actinomycotic vertebral osteomyelitis is a rare but severe condition, even in immunocompetent individuals, following routine dental procedures. Prompt recognition, multidisciplinary management, and tailored antibiotic therapy are crucial for optimizing outcomes. Clinicians should maintain a high index of suspicion for Actinomyces in patients with unexplained spinal infections and recent dental interventions.
1 Introduction
Actinomyces, a Gram-positive anaerobic bacterium predominantly found in the oral cavity, typically causes cervicofacial infections [1]. Vertebral osteomyelitis, also known as spondylodiskitis, is a serious infection of the vertebrae, accounting for approximately 3% to 5% of all osteomyelitis cases annually, and often presents with nonspecific symptoms, making early diagnosis challenging. Commonly, it arises from hematogenous spread from infections, post-surgical complications, or trauma to the spine. The lumbar spine is the most frequently affected region, followed by the thoracic and cervical areas. If left untreated, vertebral osteomyelitis can result in severe complications such as spinal deformity, neurological deficits, and even death [2]. The management of vertebral osteomyelitis primarily involves antibiotic therapy and, in certain cases, surgical intervention. Empirical therapy usually starts with broad-spectrum intravenous antibiotics tailored to cover common pathogens such as Staphylococcus aureus, including methicillin-resistant strains (MRSA). A typical regimen might include vancomycin combined with a third-generation cephalosporin or a beta-lactam/beta-lactamase inhibitor. Treatment duration generally spans about 6 weeks; however, the duration may vary based on clinical response and culture results. Surgery is indicated in cases where there is significant vertebral destruction, neurological compromise, or failure of medical management. Surgical options may include debridement of infected tissue and stabilization of the spine to prevent further complications [2].
While hematogenous dissemination to distant sites is uncommon, it is exceptionally rare in immunocompetent individuals. Actinomycotic osteomyelitis is an infrequent clinical entity, with only a handful of cases reported in the literature, with notable instances such as the one reported by L. Grach et al. (2020) where the primary source of the infection was Actinomyces viscosus, which is a member of the Actinomyces species typically found in the human oral cavity and gastrointestinal tract. The patient had a history of hypertriglyceridemia, basal cell carcinoma, severe lumbar stenosis, and left total knee arthroplasty [3]. These conditions, particularly the severe lumbar stenosis and the recent knee arthroplasty, were identified as risk factors that may have contributed to the development of vertebral osteomyelitis [3].
While cases such as Actinomyces israelii presenting as lumbar vertebral osteomyelitis following surgery have been documented [4], highlighting the indolent nature of Actinomyces infections, we present a distinctive case of extensive vertebral osteomyelitis caused by Actinomyces in a middle-aged, otherwise healthy patient, with a recent dental intervention as the sole identifiable risk factor. Our case underscores the rarity and diagnostic challenges of Actinomycotic osteomyelitis, particularly when originating from seemingly innocuous dental procedures. It highlights the critical importance of multidisciplinary care in managing severe osteomyelitis cases and the exploration of diverse management strategies to optimize patient outcomes.
2 Case History
A 46-year-old woman with a past medical history of congestive heart failure presented to the Emergency Department with severe back pain, difficulty in ambulation, and fever. She had chronic back pain, which got worse 2 days before the presentation, prompting her hospital admission on April 6, 2024. Notably, she had undergone a colonoscopy and a routine dental cleaning approximately 3 weeks before the admission. Her maximum recorded temperature was 37.9°C. Physical examination revealed full alertness and orientation, reactive pupils, and a supple neck. Tender vertebral points were identified at the L5 –S1 level, while her abdomen was soft and non-tender. Because of clinical suspicion of lumbosacral spondylodiscitis, magnetic resonance imaging (MRI) taken on April 8, 2024, indicated disc protrusion and findings suggestive of right L4 –L5 septic facet and L5 –S1 discitis [Figure 1]. Laboratory investigations over the first week of hospitalization revealed white blood cell counts fluctuating but remaining within the normal range of 4.2 to 5.3 k/uL, and platelet counts showed an increase from 433 to 657 k/uL.
3 Methods
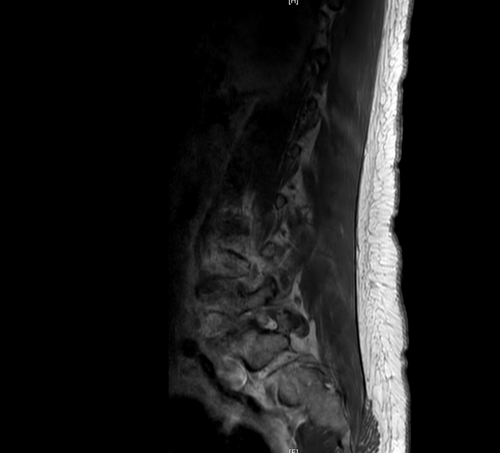
Due to the temporal association of back pain and inflammatory changes observed in the vertebrae on MRI, discitis osteomyelitis was suspected, prompting blood cultures that confirmed Actinomyces odontolyticus bacteremia. Subsequently, she was treated with IV penicillin G at 4,000,000 IU every 4 h. Four days later, she underwent a fluoroscopy-guided biopsy and aspiration sampling of the L4 –L5 region to confirm lumbar discitis and osteomyelitis, assess abscess formation, and identify potential polymicrobial infections. Tissue pathology showed clotted blood, and Karius testing was negative. Due to the ongoing penicillin therapy the patient received for 13 days, blood cultures returned negative for Actinomyces; however, a repeat MRI conducted on April 19 showed continued progression of discitis osteomyelitis, primarily at L4 –L5, as well as involvement of L5 –S1 and T7 –T8, accompanied by epidural phlegmon. Additionally, severe bilateral L4 –L5 neuroforaminal narrowing was seen [Figure 2]. Due to the progressive infection seen on MRI, her antibiotic regimen was switched to 2 g IV ceftriaxone every 12 h. A repeat Interventional Radiology (IR)—guided biopsy was taken on April 25 and sent to the Mayo Clinic for broad-range PCR. The pathology report from this biopsy was consistent with osteomyelitis, with negative infectious stains. Nevertheless, the patient's clinical condition continued to deteriorate. Computed tomography (CT) of the abdomen revealed bilateral trace pleural effusions and adjacent small atelectasis in the lungs, along with consolidation in the posterior sulci of the thoracic cavity, which is consistent with the findings of discitis and osteomyelitis identified on prior MRI.

The patient had a history of congestive heart failure, managed medically with no recent exacerbations. Given her worsening back pain and systemic signs of infection, echocardiography was performed to rule out infective endocarditis as a source of hematogenous dissemination. The results showed normal cardiac function with no detected abnormalities. As the patient had recently undergone dental cleaning, it was suspected that the source of her spinal infection could be oral bacteria seeding into the bloodstream. However, the patient noted that no problem was found during the dental cleaning and reported no dental complaints at the time of her presentation. During her hospitalization, the patient developed neutropenia, which was later attributed to ceftriaxone. Based on a review of the antimicrobial susceptibilities of the isolated organism, in consultation with infectious disease pharmacists, her antibiotic regimen was switched to IV ertapenem on May 2, 2024, which the patient has to take to a tentative end date of June 12, 2024.
4 Conclusion and Results
The patient's condition started to gradually stabilize, with a stable temperature and blood pressure, along with improvement in white blood cell count and neutropenia. Reduced tenderness at the L5-S1 level and improved ambulation ability were noted, leading to her discharge from the hospital. Follow-up arrangements comprised a repeat MRI of the lumbar spine after 4–6 weeks, weekly laboratory assessments, and outpatient parenteral antibiotic therapy.
5 Discussion
Actinomyces are a genus of Gram-positive, filamentous bacteria that are part of the normal flora of the human mouth, gastrointestinal tract, and female genital tract. While typically non-pathogenic in these locations, Actinomyces can cause infections when they invade deeper tissues, often following disruption of mucosal barriers [5]. Actinomycosis classically presents with cervicofacial manifestations characterized by swelling, abscess formation, and sinus tracts [6]. This typically occurs after dental procedures that breach the oral mucosa and is associated with male sex, poor oral hygiene, immunosuppression, and diabetes [7]. The infection can spread to distant sites via contiguous spread or, rarely, through hematogenous dissemination. Spread to the vertebrae is exceptionally rare and typically occurs via hematogenous spread [8]. Notably, there are no reported cases of vertebral osteomyelitis secondary to A. odontolyticus in the literature.
Osteomyelitis typically presents in immunocompromised adults or individuals receiving immunosuppressive medications. S. aureus remains the primary etiological agent for both acute and chronic hematogenous osteomyelitis, with Methicillin-resistant Staphylococcus aureus (MRSA) accounting for over one-third of staphylococcal-related cases [9]. Additionally, coagulase-negative staphylococci, streptococci, enterococci, and various aerobic bacilli such as Pseudomonas species, Enterobacter species, and Escherichia coli are also implicated [10]. Anaerobic infections are relatively uncommon and usually associated with complex bone fractures and chronic medical conditions, although a discernible underlying cause is almost always identifiable [11]. Our case study presents a departure from this conventional understanding, as the patient, with no prior history of bone infection, is suspected of having disseminated infection to the spine following a colonoscopy and a dental cleaning approximately 3 weeks before admission, with the dental procedure being particularly suspect due to Actinomyces' presence in the oral cavity. This is noteworthy, as there have been a few reported cases of osteomyelitis following dental procedures [12]. In these cases, contiguous spread is largely implicated; however, distant spread to the vertebra has also been reported in the literature [8].
The diagnosis of such patients is challenging due to the non-specific symptoms, indolent course, and rarity. Patients may exhibit acute or chronic back pain, mild fever, and weight loss, which are common sequelae of multiple disorders including typical bacterial vertebral osteomyelitis, tuberculosis, or malignancies. Non-specific symptoms and slow progression may delay the need for medical attention and given its rarity; necessitating a high index of suspicion among clinicians when evaluating patients with recent dental procedures who present with unexplained spinal symptoms. This case highlights the need for increased awareness and understanding of Actinomyces infections to facilitate timely diagnosis and appropriate management strategies.
Diagnosis requires microbiological culture and histopathological examination of tissue samples obtained via biopsy; however, these organisms are slow-growing, taking several weeks to appear in culture, and need specific anaerobic conditions. Furthermore, cultures may be negative in cases of antibiotic use prior to obtaining the specimen, infections with concomitant organisms, or inefficient methodology. Imaging studies like MRI or CT scans help in the localization of the infection but yield nonspecific findings of abscess or phlegmon, lacking specificity for Actinomycotic infections [7]. Clinicians should consider employing advanced imaging techniques earlier in similar presentations to facilitate timely diagnosis for actinomycotic infections. Multidisciplinary approaches are essential, involving infectious disease specialists, radiologists for advanced imaging interpretations, and orthopedic surgeons for surgical interventions when necessary.
In managing vertebral osteomyelitis caused by A. odontolyticus, a comprehensive approach is essential to address the multifaceted nature of the infection. Initial treatment typically involves high-dose intravenous antibiotics, with penicillin G being the first-line choice due to its efficacy against Actinomyces species. In this case, the patient's therapy was adjusted to include ceftriaxone and subsequently ertapenem based on antimicrobial susceptibility testing, highlighting the importance of tailoring antibiotic regimens to the specific organism and considering potential resistance patterns. Actinomycosis is considered a polymicrobial infection; therefore, the addition of beta-lactam antibiotics is recommended. The need for surgical intervention, such as debridement or drainage of abscesses, should be considered due to the presence of epidural phlegmon and potential abscess formation. Although not performed in our case, surgical management is often necessary in cases where conservative treatment fails or when there is significant neurological compromise [13]. Recent studies suggest that surgical intervention does not necessarily increase the risk of adverse outcomes compared to conservative management in appropriately selected patients [14]. Furthermore, supportive care measures, including pain management and physical therapy, are vital in enhancing patient recovery and mobility. Rehabilitation programs focusing on restoring muscle strength are also recommended post-treatment [2].
The clinical management of this case adhered to standard protocols as it did not have severe complications leading to extensive necrosis. However, this case provides insights into the potential for A. odontolyticus to cause complications, such as epidural and psoas abscesses, following dental procedures, an area not extensively documented in existing literature, emphasizing that early recognition and intervention are critical to prevent progression to severe complications. In cases complicated by abscess formation and significant tissue ischemia, incorporating hyperbaric oxygen therapy (HBOT) could offer additional benefits in the treatment of Actinomycotic osteomyelitis. HBOT enhances oxygen delivery to hypoxic tissues, which is particularly beneficial in infections involving anaerobic bacteria like Actinomyces. By promoting a more favorable environment for antibiotic efficacy and facilitating wound healing, HBOT may contribute to better outcomes [15].
Clinicians should adopt a proactive and nuanced approach to managing actinomycotic osteomyelitis; it is essential to implement rapid diagnostic protocols that include not only standard cultures but also advanced molecular techniques such as PCR to expedite the identification of Actinomyces species, as conventional cultures may yield negative results due to their slow-growing nature. Additionally, clinicians should consider utilizing serum biomarkers such as procalcitonin or C-reactive protein levels to aid in distinguishing between infectious and noninfectious causes of back pain in patients with a history of dental work. Furthermore, establishing standardized imaging protocols can enhance the detection of subtle changes associated with actinomycotic infections. Further research and documentation of similar cases are warranted to enhance our understanding of the optimal management strategies for rare presentations of osteomyelitis. Additionally, evaluation of the potential role of HBOT as an adjunctive therapy, particularly in patients presenting with severe infections and associated complications, is essential.
Author Contributions
Malik W. Z. Khan: conceptualization, investigation, methodology, project administration, supervision, writing – original draft, writing – review and editing. Abdul Moeez: investigation, methodology, resources, software, writing – original draft, writing – review and editing. Sameen Farooq: methodology, project administration, resources, software, writing – original draft, writing – review and editing. Touba Azeem: methodology, project administration, resources, software, writing – original draft, writing – review and editing. Muhammad Ahmad: resources, software, writing – original draft, writing – review and editing. Aizaz Ali: resources, software, writing – original draft, writing – review and editing. Faheemullah Khan: resources, software, writing – original draft, writing – review and editing.
Acknowledgments
The authors have nothing to report.
Ethics Statement
Consent to publish has been obtained.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images, following the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data associated with this work is reported in the article.




