Presacral Lipoblastoma Presenting With Urinary Retention
Funding: The authors received no specific funding for this work.
ABSTRACT
Lipoblastoma is a rare fatty tumor that can uncommonly arise in the presacral space. When the lesions attain sufficient size, they can cause a multitude of infiltrative and obstructive symptoms. In this report, we present the case of a 1-year-old infant who presented with recurrent urinary retention for 4 months due to a large presacral lipoblastoma, which was successfully resected. This case is unique as it highlights the lesion's rare location in the presacral space and the possibility of such lesions presenting with urinary retention.
Abbreviations
-
- CT
-
- Computed tomography
-
- MRI
-
- magnetic resonance imaging
1 Introduction
Lipoblastoma is a rare benign tumor predominantly found in the pediatric population, with the majority of cases identified in children under 3 years of age and more commonly in males [1]. It usually presents clinically as a painless, rapidly expanding soft tissue mass [2]. However, when the growth compresses adjacent structures, symptoms may develop [1, 2]. Various diagnostic imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are crucial in diagnosing this condition, as these modalities reveal the main fatty consistency leading to the consideration of differential diagnoses [2-4].
Lipoblastoma typically originates in the subcutaneous tissues of the extremities and trunk, though occurrences in the sacral area are comparatively rare [3, 5]. The case described here involves a biopsy-confirmed presacral lipoblastoma in a child who experienced urinary retention due to the tumor's location and growth. This presentation highlights the importance of recognizing the potential for lipoblastoma to manifest in less common locations and the implications this has for symptom development and treatment planning.
1.1 Clinical History
A 1-year-old male patient presented with a 4-month duration of intermittent difficulty with urination that progressively worsened, leading to multiple episodes of acute urinary retention that required catheterization multiple times before he was referred to our center. The family also complained of constipation. Otherwise, the patient was free of fever or surgical interventions.
He is the fifth child in his family and was born by caesarian section for an indication of prolonged labor. He cried immediately after birth and did not require neonatal intensive care. He is vaccinated according to the Ethiopian national immunization program. No prior health concerns or hospital admissions were reported. The family's medical history is non-contributory. On physical examination, the child appeared comfortable and had stable vital signs (respiratory rate: 26/min, pulse rate: 96/min, and temperature: 36.5°C). His middle upper arm circumference (MUAC) was 12 cm, corresponding to moderate acute malnutrition. An abdominal examination revealed only a distended bladder. No signs of ascites or organ enlargement were present.
1.2 Investigations
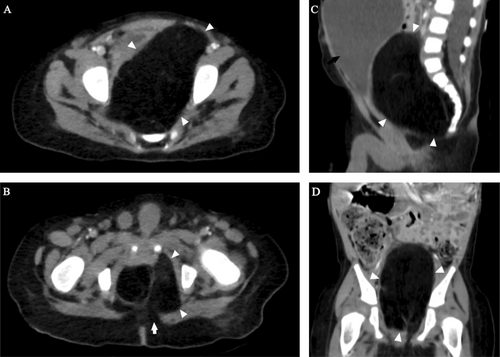
Pertinent laboratory examinations, including complete blood count and urinary analysis, were within normal ranges. An ultrasound examination identified a fat-containing tumor in the retrovesical space. For a better assessment, a post-contrast CT was ordered. Although MRI was our first choice for imaging, the family could not afford the cost. The CT examination (Figure 1) revealed a large non-calcified fat attenuating presacral mass, measuring 12 × 7 × 6 cm in the longest CC × TR × AP dimensions, with internal enhancing linear strands. The lesion blended with the perineal fat inferiorly. The mass had compressed the bladder outlet and pushed it anterosuperiorly. This was the reason for the child's urinary retention. The mass completely effaced the rectal lumen, making it impossible to identify.
1.3 Outcome and Follow-Up
Next, after nutritional rehabilitation, an anterior (or abdominal) surgical approach achieved a complete open resection of the mass. Post-operatively, the patient convalesced smoothly without any acute complications. On the 18th post-operative day, the child was stable with a well-healed transverse abdominal scar. Symptoms of urinary retention had also resolved.
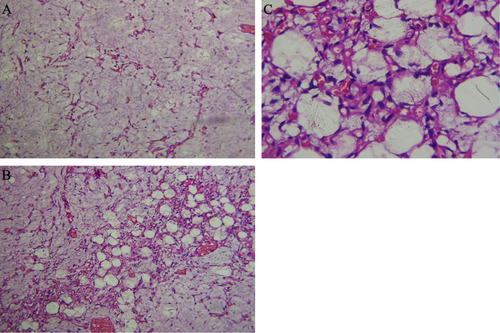
The resected specimen had typical pathologic features of lipoblastoma (Figure 2). It showed sheets of mature adipocytes separated by fibrous septa and abundant myxoid substance. Pleomorphic changes or invasion of adjacent structures were not seen. Follow-up imaging, preferably with MRI is planned after 12 months.
2 Discussion
Lipoblastoma is a rare, fat-containing mesenchymal tumor that lacks mature adipocytes [2, 6]. Despite the lack of fundamental pathological differentiation, patients might present with a lipoblastoma, an encapsulated superficial focal lesion, or an infiltrative aggressive lesion known as lipoblastomastosis, which often tends to be deep and infiltrative [3-5]. Lipoblastoma accounts for 1% of all childhood tumors [6], and 90% of cases are diagnosed in children under the age of 3 years [3]. Lipoblastoma has a male predominance with a ratio of 4:1 [1]. It primarily affects the trunk and extremities due to their high immature fat content [3, 5]. Patients can develop symptoms following compression of nearby nerves, blood vessels, and airways [2, 7, 8]. However, asymptomatic growth leading to large size is more likely to occur in accommodating compartments, such as the deeper retroperitoneum [9], including the rare presacral location. In a retrospective case review by Spătaru et al. [10], among 8 patients, only 1 was located in the presacral region.
Lipoblastomas are derived from embryonic white cells, and unlike lipomas, they lack mature adipocytes [6]. Macroscopically, lipoblastomas are usually soft and well-defined lesions with yellow-white cross sections [2, 6]. Microscopy identifies multi-vacuolated adipocytes, fibrous septa, and myxoid stroma [2, 6].
A wide variety of imaging modalities reflect the lesion's primary fat-containing nature [2, 3]. Lipoblastoma displays hyperechogeneity on ultrasound, hypodensity on CT, hyperintense signal on T1 and T2 sequences, and low signal on fat sat-MRI [2, 3]. However, an immature lipoblastoma can appear on a T1-weighted image with an average signal intensity, and the intensity of T2-weighted images varies depending on the amount of myxoid and fibrous components [5]. The lesion shows enhanced septas and solid components in post-contrast images [7]. Despite being a benign tumor, lipoblastoma can appear aggressive locally and present with features like neurovascular encasement, compartmental invasion, diffuse infiltration, and intraspinal involvement [10].
When a young pediatric patient has a mesenchymal soft tissue fat-containing mass, lipoblastoma, lipoma, teratoma, and liposarcoma are among the possible differential diagnoses [6]. Teratomas are a less likely candidate when other elements of the germ cell tissue, such as calcifications, are absent [3, 11]. The possibility of lipoma is also less likely, owing to the presence of non-fatty soft tissue components and its rare occurrence in a very young patient [6, 11, 12]. Although the diagnosis of liposarcoma, particularly the myxoid form, is consistent with the presence of a non-fatty soft tissue component in a primarily fatty lesion, it is important to note that liposarcomas are extremely uncommon in children under the age of five [11, 12].
Although lipoblastoma and lipoblastomatosis are benign tumor with no potential for metastases or malignant transformation, they carry a non-negligible risk of recurrence. A systemic review by Dao et al. [13] reported a pooled recurrence rate of 16.8%, which was higher for incompletely resected tumors as well as in lipoblastomatosis when compared to lipoblastomas. This makes a complete surgical tumor excision the ideal treatment of choice [3, 8]. Especially for infants, such aggressive radical surgery can be mutilating; therefore, we prefer non-mutilating wide local excision whenever possible [4]. Given the risk of recurrence, follow-up for a minimum of 5 years is advised [9].
3 Conclusion
A child with obstructive urinary symptoms and a large, predominantly fatty mass in the presacral region can represent a lipoblastoma. Ultrasound, CT, and MRI can determine the fatty nature of the lesion, and histopathologic examination can provide a definitive diagnosis. The preferred course of treatment is a complete resection with a serial follow-up MRI for at least 2 years.
Author Contributions
Samuel Sisay Hailu: writing – review and editing. Misiker Gebremariam Waktola: supervision. Mulugeta Temesgen Bonger: writing – review and editing. Henok Dessalegn Damtew: writing – original draft. Isa Salo Abdo: data curation, investigation, writing – original draft. Atiklet Zerihun Zewdie: conceptualization, visualization. Hidaya Yahya Mohammed: methodology, writing – review and editing. Abubeker Fedlu Abdela: conceptualization, writing – review and editing. Yodit Abraham Yaynishet: writing – original draft, writing – review and editing. Michael Teklehaimanot Abera: conceptualization, data curation, project administration, visualization, writing – original draft, writing – review and editing.
Ethics Statement
This authors have nothing to report.
Consent
Written informed consent was obtained from the parents of the patient for anonymized patient information to be published in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data openly available in a public repository that issues datasets with DOIs.




