Microsurgical Semilunar Bilaminar Technique Halts Progression of Marginal Tissue Recession by Soft Tissue Phenotypic Modification—A Case Report With 3-Year Follow-Up
Funding: The authors received no specific funding for this work.
ABSTRACT
Phenotype modification therapy using the novel semilunar flap with xenogeneic collagen matrix improves gingival phenotype, root coverage and increased keratinized tissue width. It also halts the progression of recession, enhances tissue resilience and improved plaque control sustainable over 3 years. Collagen matrix avoids second site surgery and hence less morbidity.
1 Introduction
The occurrence of marginal tissue recession (MTR) in different degrees is a prevalent phenomenon observed in a significant proportion of individuals with periodontal disease. Over the years, numerous ways have been developed to effectively manage MTR as our comprehension of soft tissue biology and wound healing has advanced. In recent times, there has been a shift in focus from achieving root coverage to surgically altering the gingival soft tissue phenotype [1]. This approach has demonstrated its effectiveness in preventing further clinical attachment loss (CAL) and the progression of MTR. Currently, autogenous soft tissue grafting using connective tissue graft (CTG) obtained from various donor sites, in combination with a coronally advanced flap (CAF) or tunneled flap, continues to be widely regarded as the most effective method [2]. When autogenous soft tissue transplantation cannot be performed due to anatomical constraints or the patient's refusal to undergo additional surgery, the use of soft tissue alternatives that involve replacements becomes a viable alternative. A unique modification of semilunar CAF employing a bilaminar microsurgical method with xenogeneic collagen matrix (XCM) is presented in this case report. The aim of this case report was to evaluate the progression of MTR following the use of soft tissue phenotype modification therapy. The unique aspect of this case report lies in its novel approach to managing marginal tissue recession MTR by combining soft tissue phenotype modification therapy (PMT) with a semilunar flap design and XCM. Unlike traditional treatments that primarily focus on root coverage with soft tissue grafting, this case integrates a strategy to modify the gingival phenotype itself, improving both gingival thickness and keratinized tissue. This modification potentially impedes or decelerates the progression of MTR, which is a novel concept in periodontal therapy. The achievement of long-term plaque control and the prevention of MTR progression are key highlights of this unique intervention. These combined factors make this case report unique, offering a promising alternative to traditional MTR management strategies by addressing both the mechanical and biological aspects of soft tissue regeneration and phenotype improvement.
2 Case History/Examination
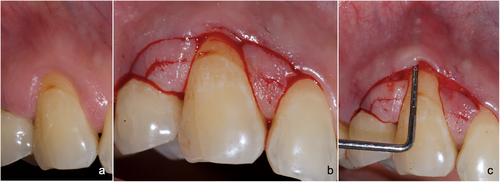
The reported case was performed in a tertiary care teaching institution in the year 2021. The reporting is in accordance with CARE—CAse REport 2017 guidelines [3]. A 50-year-old man reported with complaints of pain and discomfort in his upper right teeth when brushing. His medical history was deemed non-significant, and he was classified as ASA-I in terms of his physical status. The patient appeared to be in good dental health until he began experiencing sensitivity while brushing his maxillary right anterior sextant for more than 3 months and recently noticed bleeding from the gingival region with respect to tooth number 13 (FDI Notation). The maxillary right canine (tooth number 13) had marginal tissue recession (MTR) with a recession height (RH) of 3.0 mm, a recession width (RW) of 5.0 mm. The width of the attached gingiva (WAG) was 2.0 mm and the width of the keratinized tissue (WKT) was 3.0 mm. There was no loss of papillary soft tissue or interdental attachment, but the facial soft tissue was classified as “thin” based on probe visibility. Based on clinical findings, a definitive diagnosis of Cairo's Class I A (-) MTR with thin soft tissue phenotype in tooth no# 13 was made (Figure 1a). After receiving written informed consent for the planned treatment as well as publication along with clinical photographs, the patient was treated under an 8X magnification of an operating microscope.
3 Methods (Treatment)
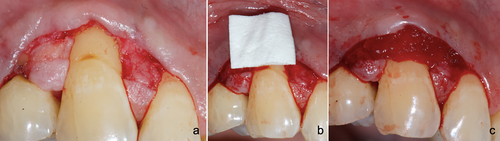
Following profound local anesthesia with infiltration (2% Lignocaine with 1:800,000 Epinephrine) and pre-emptive analgesia with Iboprufen 600 mg orally 30 min prior to the procedure, the patient was treated to modify the soft tissue phenotype of the facial gingiva in tooth number 13. A commercially available XCM (Mucograft, Geistlich Pharma, Geistlich Pharma India Pvt. Ltd) was used as a soft tissue substitute in this case. All the surgical procedures were carried out using split thickness preparation with a microsurgical knife (SB004, MJK instruments, France). In this semilunar flap design, the coronal microsurgical incision (CSM) and apical microsurgical incision (ASM) were made at the interdental papillae on both sides of the affected tooth (Figure 1b). Both micro-incisions were made superficially at a depth of no more than 1 mm, avoiding the interdental papillary thickness in their entirety. After placement of ASM and CSM (Figure 1c), the intervening papillary tissue was de-epithelialized using Castroviejo blade (Figure 2a). A sulcular connecting incision was completed between the two mesial extremities of ASM, and a split-full-split flap was prepared 5 mm beyond the mucogingival junction (MGJ). The XCM (12 × 10 × 2 mm) was secured at the recipient site slightly coronal to the CEJ with cross-mattress 5/0 polyglactin sutures (Figure 2b,c). The split-full-split semilunar flap apical to ASM was passively advanced over the de-epithelialized portion of the papillae in order to accomplish edge-to-edge adaptation of the incision ends of ASM and CSM. The flap was secured with an “approximation suture” consisting of a single interrupted 5/0 Prolene suture on each side that merged the extremities of ASM and CSM (Figure 3a). Additionally, the flaps were secured with “coaptation sutures” using 8/0 polyamide and multiple interrupted sutures adjacent to approximation sutures on either side, which passively brought the flap margin 1 mm coronal to CEJ (Figure 3b—facial view and 3c—occlusal view). The patient was restricted from mechanical plaque control over the surgical site for 2 weeks and given 0.12% chlorhexidine for chemical plaque control. Following surgery, the sutures were removed 2 weeks later and oral hygiene measures were reinstated. The patient received supportive periodontal therapy with a 6 monthly follow-up appointments and was observed for a total of 3 years.

4 Conclusion and Results
There were no intra- and postoperative complications reported. The numerical rating scale (NRS) pain score was 2 out of 10 within the first 24 h. The patient experienced least post-operative morbidity as a result of the absence of a second surgical site for harvesting autogenous soft tissue grafts. The probe tip was completely invisible, indicating the shift in soft tissue phenotype from “thin” to “thick” with stable gingival margin. A 3-year follow-up showed the position of the coronally advanced gingival margin to be at the CEJ and stable over 3 years (Figure 4a—facial view and 4b—occlusal view). The patient was able to demonstrate significant improvement in self-performed plaque control measures. The pre- and post-periodontal parameters are presented in Table 1.

| Pre- and post-comparison of periodontal parameters | ||||||||
|---|---|---|---|---|---|---|---|---|
| Timeline | RH (in mm) | RW (in mm) | WKT (in mm) | WAG (in mm) | Step deformity | CEJ | PD (in mm) | CAL (in mm) |
| Baseline | 3.0 | 5.0 | 3.0 | 2.0 | Absent | Present | 1.0 | 4.0 |
| 6 months | 1.0 | 0.0 | 4.0 | 3.0 | Absent | Present | 1.0 | 2.0 |
| 12 months | 0.0 | 0.0 | 4.0 | 3.0 | Absent | Present | 1.0 | 2.0 |
| 18 months | 0.0 | 0.0 | 4.0 | 3.0 | Absent | Present | 1.0 | 2.0 |
| 24 months | 0.0 | 0.0 | 4.0 | 3.0 | Absent | Present | 1.0 | 2.0 |
- Abbreviations: CAL, clinical attachment loss; CEJ, cementoenamel junction; PD, probing depth; RH, recession height; RW, recession width; WAG, width of attached gingiva; WKT, width of keratinized tissue.
5 Discussion
Semilunar CAF is not novel in periodontal plastic surgery and is frequently recommended for treating single-tooth recessions [4]. The inherent problem with the semilunar CAF is its compromised vascularity, which relies exclusively on the papillary blood supply, which is only a supplementary vascularity [5], and the major vasculature, which runs in the distomesial and apico-coronal directions are completely severed in the conventional semilunar CAF [6]. When the same semilunar flap must be considered for microsurgical approaches, the fundamental idea of maintaining vasculature integrity is contested. Therefore, in the present case, a microsurgical approach with modified semilunar microincisions and edge-to-edge closure was performed in conjunction with a bilaminar approach. This surgical technique provides exceptional access to subgingival tissues while preserving the integrity of the papillae, thereby enhancing vascularity at the surgical site. The combination of ASM and CSM with a split-full-split approach increases tissue volume not only in the region apical to MTR but also in the papillary zones, thereby altering the soft tissue phenotype three-dimensionally (apical, mesial, distal) to MTR, particularly when combined with a bilaminar technique as done in the presented case. The position of ASM is modifiable based on RH, and it can be parallel when MTR is symmetrical or non-parallel when MTR is asymmetric. The placement of CSM is guided by the CEJ or where the graft has to be secured coronally. The split-full-split method additionally provides sufficient room for the graft material. As the graft or its substitute is entirely covered by the advanced flap, the dual vascularity from the underlying periosteum as well as the under surface of the flap compensates for the higher demands of graft nutrition over an avascular root surface [7], resulting in improved surgical outcomes (Figure 4).
It is well established that inadequate attached gingiva, especially combined with a thin soft tissue phenotype, causes clinical progression of MTR which renders maintaining oral hygiene even more difficult [8, 9]. It is best understood that connective tissue graft (CTG) has the ability to trigger keratinization of the overlying epithelium and is still the gold standard in periodontal plastic microsurgical operations as it is an autogenous graft [10]. However, when CTG is covered by a flap containing the majority of non-keratinized mucosa, the ability of CTG cells to interact with the overlying epithelium may or may not induce keratinization [11]. After 3 months, the ground-breaking research with histological evidence of healing in an animal model suggested that CTG had been partially destroyed [12]. Due to ethical issues, there has been minimal human research on integration of CTG and its influence on the overlying epithelial keratinization [13]. In addition, it is now better understood that despite the inherent potential of CTG, epigenetic factors play a significant role in epithelial keratinization [14]. In the case presented here, the soft tissue substitute (porcine collagen matrix) exhibited alterations in soft tissue phenotype. The increase in WKT, which may be attributed to the genetically determined process of “mucogingival junction (MGJ) reversal phenomenon” over time, as there is at present less evidence of collagen matrix inducing keratinization of overlying epithelium [15, 16].
In such situations, it is crucial to recognize the immense benefits of microsurgical treatment. By utilizing a microsurgical approach in periodontal plastic surgeries, post-operative morbidity can be reduced and extremely high rates of clinical success can be achieved. One of the primary reasons for improved angiographic outcomes after root coverage procedures is the early revascularization in microsurgical approaches as early as 7 days post-operatively, which occurs in close to 95% of cases [17]. There was no statistically significant difference in root coverage outcomes (96% vs. 91%) in a controlled clinical trial that compared microsurgical method using CTG and macrosurgical approach with semilunar CAF [18]. In the reported case, however, both the semilunar CAF and CTG have been combined with a microsurgical technique, potentially doubling the benefits of surgical outcomes. For CTG harvesting, whether the procedure is performed macroscopically or microscopically, the viability of the grafted tissue depends on the ability of recipient bed to maintain sufficient blood supply to restore early graft circulation. Periodontal microsurgery necessitates a different frame of mind; as it is technique-sensitive and more demanding than conventional surgery, because it is less invasive and less traumatic. The operating microscope enables surgeons to perform precise, and delicate surgical procedures with vital impacts on wound healing.
The emergence of periodontal microsurgery can be perceived as a logical progression within the realm of periodontics. The alteration of soft tissue phenotype plays a crucial role in the attainment of stable soft tissues and the prevention of MTR advancement, as opposed to its mere management. When the thin soft tissue phenotype is combined with the existence of precipitating and predisposing variables, it results in the breakdown of the epithelial layer and subsequent CAL, ultimately leading to progressive MTR. Nevertheless, extensive evidence has unequivocally shown that augmenting the soft tissue phenotype using PMT can effectively withstand the inflammatory process and the potential deterioration of soft tissue attachment, ultimately resulting in MTR. The modification of phenotypic traits can be achieved by the utilization of soft tissue grafts and substitutes, leading to successful outcomes. The utilization of microsurgical procedures in the process of wound healing results in more than a twofold rise in advantages, as it ensures the adherence to sound biological and vascular principles.
This case highlights the importance of considering the gingival phenotype in the management of MTR. While the observed improvements in root coverage and WKT are promising, the significant change in gingival phenotype underscores the need for routine assessment of soft tissue characteristics before and after treatment to completely evaluate the impact of PMT and other interventions in management of MTR. Though promising, these findings of this case study require validation through larger sample size with longer follow-up to confirm the long-term efficacy of PMT with this novel semilunar flap design and XCM compared to autogenous soft tissue grafts in management of MTR.
Author Contributions
Saravanan Sampoornam Pape Reddy: conceptualization, resources. Delfin Lovelina Francis: formal analysis, methodology. Manish Rathi: formal analysis, investigation. Ruchi Harish: methodology, resources. Ravikiran Narayana: writing – original draft. Balaji Manohar: writing – review and editing. Shaili Pradhan: writing – review and editing.
Acknowledgments
The authors would like to thank Havildar Ram Kumar, of the Army Dental Centre (Research and Referral) Delhi, India, for his assistance throughout the management of this case.
Consent
A written informed consent form was obtained from the patient reported in this case report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
There is no data generated from this case report.




