Primary Leiomyosarcoma of the Kidney: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
Primary renal leiomyosarcoma is a rare but highly aggressive tumor with a poor prognosis. Early detection and surgical excision provide the most effective initial treatment. However, vigilant postoperative surveillance is critical due to the elevated risk of tumor recurrence and metastasis, as seen in this case.
Summary
- All healthcare providers should be familiar with the clinical signs and diagnostic characteristics of primary leiomyosarcoma of a kidney.
1 Introduction
Primary sarcomas comprise 0.8%–2.7% of all renal tumors in adults [1]. Among renal sarcomas, leiomyosarcoma (LMS) accounts for 50%–60% of all cases. It occurs more frequently in females and typically manifests between the 40s and 60s. The signs and symptoms are like those of renal cell carcinoma (RCC), mainly pain, palpable mass, and hematuria, all of which are indicators of an extensive local disease [1].
Imaging may not always differentiate between leiomyosarcomas and renal cell carcinomas in all patients [2]. LMS has a significant propensity for local recurrence and often metastasizes to distant organs [3].
Adhering to Surgical CAse REport (SCARE) guidelines, we report a case of primary renal LMS extending into the renal vein in a 31-year-old woman patient managed with nephrectomy and adjuvant chemotherapy [4].
2 Case History/Examination
A 31-year-old woman with history of sudden onset, dull, and intermittent type right-sided flank pain presented to emergency. She did not give history of hematuria, burning micturition, urinary frequency, urgency, or fever, history of prior surgeries, smoking, and alcohol use. She was diagnosed to have a right renal mass on radiological examination. She underwent a right radical nephrectomy, and histopathology confirmed renal leiomyosarcoma, showing a sarcomatoid tumor with positive smooth muscle actin and desmin markers.
3 Methods
Physical examination was normal. Routine blood investigations were within normal limits. Ultrasonography of the abdomen revealed a right-sided renal mass. Contrast-enhanced computed tomography (CECT) of the abdomen revealed an enhancing mass 11.2 × 10 × 12.3 cm involving the mid and lower pole of the kidney in its entirety along with an extension to the right psoas muscle, pelvic–ureteric junction, and renal vein.
A provisional diagnosis of right RCC with inferior vena cava thrombus was made. The patient underwent an elective right radical nephrectomy with inferior vena cava thrombectomy and the specimen was sent for histopathological examination.
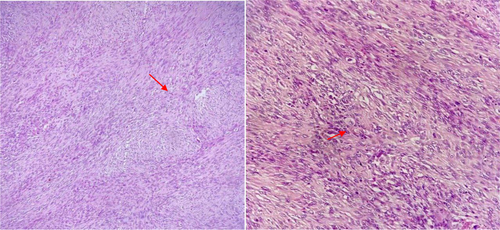
On gross examination, the cut section of the right kidney showed a heterogeneous mass measuring 13.0 × 11.5 × 10.5 cm involving the entire kidney. The mass was gray-white with large friable dark brown areas of necrosis and hemorrhage. Focally, a gray-white area was noted which showed a whorling pattern (Figure 1). The ureteric resection margin was grossly free of tumor.

Microscopically, the tumor was composed of spindle-shaped cells arranged in interlacing fascicles, bundles, and whorls (Figure 2). The tumor cells were moderately pleomorphic with a moderate amount of eosinophilic cytoplasm, oval to elongated nuclei, vesicular chromatin, and inconspicuous nucleoli. Mitotic figures were frequent, constituting a 19/10 high-power field. Large areas of necrosis and hemorrhage were noted. The mass involved the renal sinus and perirenal fat, however, Gerota's fascia was free of tumor. The lymphovascular invasion was noted. Extensive sampling failed to reveal any epithelial component resembling renal cell carcinoma. Microscopic examination of the inferior vena cava thrombus revealed a tumor with similar morphology as in the kidney.
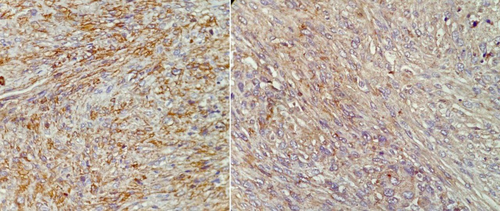
Immunohistochemistry was done and tumor cells showed diffuse positivity with smooth muscle actin (SMA) and focal positivity for desmin (Figure 3). Cytokeratin was negative. A final diagnosis of renal leiomyosarcoma, high grade, (Grade 2) using the French Federation of Cancer Centers System, was made. The renal leiomyosarcoma was staged as Stage III (T2bN0M0), meaning the tumor had extended into the renal vein without evidence of lymph node involvement or distant metastasis at the time of diagnosis.
The patient underwent two cycles of adjuvant chemotherapy with doxorubicin (IV 75 mg/m2 every 3 weeks). Four months post-surgery, she developed pulmonary complications, and computed tomography (CT) of the chest confirmed the presence of lung metastases, which ultimately contributed to her death.
4 Discussion
LMS is a malignant tumor originating from smooth muscle cells and ranks among the most prevalent subtypes of soft tissue sarcomas. It typically occurs in older individuals, particularly those in their 60s and 70s. The tumor primarily develops in the extremities, abdomen, retroperitoneum, and uterus. Primary LMS of the kidney is a rare tumor [5].
Previous studies have shown that primary renal LMS is more common in older individuals, typically in their 60s. However, our patient was relatively younger, presenting in her 40s [6]. The clinical presentation of renal LMS is variable and mostly overlapped with that of other renal neoplasms like RCC. Symptoms typically manifest with the expansion of the tumor, leading to the compression of surrounding structure. These symptoms include the presence of abdominal mass, lumbar pain, and hematuria, as well as systemic symptoms like nausea, vomiting, and abdominal pain [1]. A prior case series of 10 patients with renal LMS reported lumbar pain as the most common symptom (60%) [1].
Radiologically, renal leiomyosarcomas appear as well-circumscribed, expansile, and heterogeneously enhancing solid masses on CT scans. These tumors usually project from the kidney in an exophytic fashion. However, these findings are not specific, and a definitive histopathological diagnosis is essential to rule out renal cell carcinoma and other tumors [7].
Grossly, LMS resembles leiomyoma, presenting as a well-defined tumor with a whorled appearance on the cut surface. However, LMS is fleshier and typically shows areas of necrosis, hemorrhage, and cystic changes. At a microscopic level, frequent mitoses, necrosis, and increased nuclear pleomorphism are more indicative of LMS [8].
Histologically, renal LMS must be distinguished from sarcomatoid RCC, leiomyoma, and angiomyolipoma (AML). Sarcomatoid differentiation in RCC lacks the typical alternating fascicles seen in LMS and predominantly comprises pleomorphic cells, while LMS exhibits a cellular resemblance to smooth muscle cells [8]. Immunohistochemistry plays a crucial role in distinguishing between sarcomatoid RCC and LMS. LMS exhibit myoid marker expression and lack cytokeratin positivity. Previous studies have reported immunohistochemical positivity rates of 100% for vimentin, 90% for desmin, and 80% for SMA [1]. However, sarcomatoid renal cell carcinomas may not consistently exhibit cytokeratin positivity and could express SMA. Similarly, some leiomyosarcomas may display cytokeratin and epithelial muscle antigen (EMA) expression [9, 10]. In the latter situation, the presence of desmin aids diagnosis as it is positive in leiomyosarcoma but not in sarcomatoid carcinoma [11]. In our case, a typical spindle cell tumor arranged in interlacing fascicles in conjunction with immunohistochemistry made diagnosis possible. Renal angiomyolipoma should also be included in the assessment of smooth muscle tumors of the kidney. In renal angiomyolipoma, fascicles of smooth muscle cells are interspersed with mature adipose tissue and thick-walled blood vessels [12]. Furthermore, angiomyolipoma shows positivity for melanocytic markers, including HMB-45, which can aid in diagnosis of challenging cases [13, 14].
Sarcomatoid RCC responds to tyrosine kinase inhibitors (TKIs) such as sunitinib and immune checkpoint inhibitors like nivolumab. Malignant AML is treated with mTOR inhibitors such as everolimus. Sarcomatoid UC, on the other hand, benefits from immune checkpoint inhibitors targeting PD-1/PD-L1, such as atezolizumab or pembrolizumab. In contrast, renal LMS, as a soft tissue sarcoma, is primarily managed with radical nephrectomy. Adjuvant chemotherapy, particularly with doxorubicin-based regimens, may be considered in high-grade or metastatic cases, although its role remains controversial [15].
Renal LMS is an aggressive tumor with the most common site for distant metastasis being liver, lung, and bone [16]. The prognosis of renal LMS is generally poor as compared to other renal neoplasms with a median overall survival of 25 months and a 5-year overall survival rate of 25% [1]. The tumor grade and the effectiveness of the operative treatment are the independent prognostic factors for long-term survival [1]. Radical nephrectomy is the preferred treatment for renal LMS. The use of adjuvant/neo-adjuvant chemotherapy/radiotherapy remains controversial, although sporadic reports suggest potential benefits in reducing tumor recurrence and achieving long-term survival [17].
5 Conclusion
Renal leiomyosarcoma is a rare tumor, and it should be differentiated from the sarcomatoid variant of renal cell carcinoma, leiomyoma and angiomyolipoma. It behaves aggressively and has an unfavorable prognosis. An accurate diagnosis and subsequent management of the tumor requires careful histological analysis and interpretation of immunohistochemistry markers.
Author Contributions
Srijana Khati: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing. Sagar Rana Magar: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft. Ankita Simkhada: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft. Ramesh Paudel: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing. Surendra Khanal: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft. Bishal Panthi: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft. Sadmarg Thakur: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing. Sujan Paudel: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing. Prajjwol Luitel: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing.
Consent
A written consent has been collected from the next of kin for publication of this report and is available upon request by the editor of the journal.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data supporting the conclusions of this report are contained within the report. Additional non-relevant patient data are protected under patient privacy regulations and policies.




