Cardiac MRI prior to liver biopsy in a Fontan patient: A case report
Abstract
The management of adults with complex congenital heart disease requires a multidisciplinary team (Heart Team).
1 INTRODUCTION
The Fontan procedure may be applied in the treatment of complex congenital heart disease featuring a single functional ventricle. Congestive hepatopathy is a medium and long-term complication of this surgery. We report the case of a 27-year-old man with a single ventricle anatomy, corrected by means of an extracardiac Fontan procedure, who underwent liver biopsy for suspected advanced hepatic fibrosis at fibroscan. A transjugular approach was selected in view of the presence of concomitant anticoagulant therapy and lower risk of bleeding compared with standard ultrasound-guided percutaneous needle biopsy. A cardiac angio-MRI clarified the highly complex anatomy of the patient. The involvement of a multidisciplinary team of Cardiologists and Radiologists (Heart Team) played a pivotal role in promoting a safe and successful outcome of the transjugular procedure. The procedure described may also be performed in this specific and potentially more challenging clinical setting characterized by a complex anatomy and potential risk of life-threatening arrhythmias.
The Fontan repair, first described in 1971 by the French surgeon Francois Marie Fontan, is a palliative surgical intervention performed in subjects with univentricular heart. It implies diverting venous blood from inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries with or without interposing a conduit and without passing through the hypoplastic ventricle.1 The Fontan procedure can be considered for complex congenital heart disease (CHD) with a single functional ventricle, mostly because of the absence of an adequate atrioventricular valve or pumping chamber, such as in tricuspid valve atresia, pulmonary valve atresia with intact interventricular septum, double inlet ventricle, and hypoplastic left heart syndrome.2 Complications after Fontan procedure are common and mainly related to increased venous pressure and congestion, and to chronic low cardiac output.2 Liver involvement is one of the most important extracardiac manifestations of the late Fontan patient and includes progressive development of congestive hepatopathy, cirrhosis, hepatocellular carcinoma, and liver failure.3
This is the first case report illustrating a liver biopsy carried out in a Fontan patient by means of a transjugular approach supported by prior cardiac MRI imaging to provide in-depth delineation of his complex venous anatomy.
2 CASE PRESENTATION
A 27-year-old man was admitted to our Hospital to undergo liver biopsy for suspected hepatic fibrosis. He had a past medical history of single ventricle anatomy (atrioventricular concordance, left ventricle pumping chamber, hypoplastic right ventricle, large ventricular septal defect, ventriculo-arterial discordance) corrected by means of an extracardiac Fontan procedure at the age of twelve. Surgery consisted in insertion of the IVC into a pulmonary artery fenestrated conduit and direct connection of the SVC to the pulmonary artery. Subsequently, at the age of 26, the patient underwent embolization to occlude several venous collateral vessels responsible for desaturation. Furthermore, the patient was also affected by a right parietal subcortical brain abscess, unrelated to the presence of infective endocarditis, which required evacuative surgery. As a consequence, the patient developed secondary epilepsy. He was taking Bisoprolol 1.25 mg/d, Ramipril 5 mg/d, Warfarin for INR 2-3, and Levetiracetam 1000 mg bid. His saturation ranged from 88% to 92%.
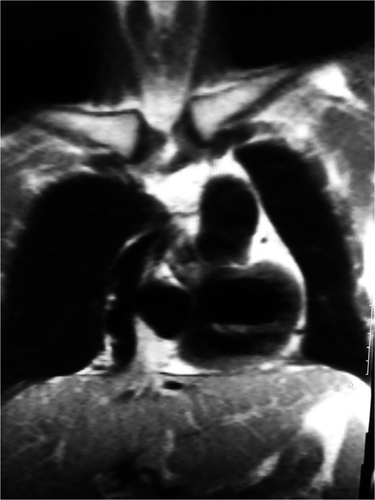
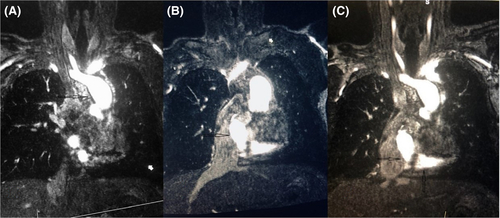
Laboratory tests showed a rise in transaminases, bilirubin, alkaline phosphatase, and gamma-glutamyl transferase as well as a decrease in albumin levels, thus suggesting possible worsening of liver function. The patient had no clinical signs of liver disease, but his fibroscan was 40.0 kPa with an interquartile of 5.5 and a cap of 282. These high fibroscan scores are usually related with the presence of advanced fibrosis, although in Fontan patients may simply be due to the presence of liver congestion. Accordingly, liver biopsy was scheduled to determine prognosis and assess the potential need for hepatocellular carcinoma surveillance. A transjugular liver biopsy (TJLB) approach was selected. A previously performed cardiac angio-MRI (Siemens 1.5 Tesla MRI Scanner; MAGNETOM Sola) facilitated in-depth clarification of the complex anatomy of this Fontan patient (tortuous, dilated, and right-to-left SVC-Fontan conduit-IVC-right hepatic veins. See sequential Figures 1,2 and 3).

Percutaneous transjugular access was achieved using ultrasound guidance with linear-array probe. Puncture of the right internal jugular vein was preferred as a right-side approach tends to provide a straighter route for catheter and guide. Local anesthesia was administered. A small skin incision was made and a wire used to navigate through the above-stated tortuous route from SVC into the right hepatic veins. Venography was subsequently performed to exclude hepatic vein stenosis and assess parenchymal flow. A liver specimen of approx. 2 cm3 was then sampled using a cutting biopsy needle. During the procedure, heparinized saline serum (4000 IU/500 mL) was used.
TJLB was performed without complications, and the patient discharged the following day. Microscope examination excluded the presence of advanced fibrosis.
3 DISCUSSION
As a result of the steady progress in cardiac surgery, thousands of individuals affected by CHD, who otherwise would not have survived, have reached adulthood.4 Nowadays, the number of adults living with CHD outweighs that of children affected by the same condition. This is particularly evident for those with complex CHD, including subjects who have undergone a Fontan procedure due to single ventricle anatomy. Although this palliative surgery has allowed patients to grow up, it has not been without significant challenging consequences, including liver function impairment.5
A strong correlation between congestive heart failure and liver disease was first demonstrated many years ago.6 Liver involvement is indeed one of the most important extracardiac manifestations of Fontan patients in late follow-up. Patients who have undergone Fontan palliation of single ventricle physiology are prone to develop a variety of liver lesions, both benign and malignant. The impact of liver disease on the aging cohort of Fontan patients may be of particular relevance due to the specificity of their hematic circulation. Increased central venous pressure in these subjects is a key factor implicated in the development of Fontan-related liver involvement, while other potentially involved mechanisms include pre-Fontan hypoxemia, perioperative liver injury, and altered hepatic blood flow.7-10 Fontan-related liver disease was described for the first time in a case report published in the early eighties.11 Latterly, the first small case series of autopsies on patients who had undergone Fontan surgery revealed how the majority displayed evidence of chronic passive hepatic congestion. Additionally, approximately 50% were also affected by hepatic centrilobular necrosis or cirrhosis.3 Severely compromised Fontan patients may even go on to develop hepatocellular carcinoma.12
Traditional blood markers of liver disease often proved to be insensitive and nonspecific, and frequently failed to correlate with degree of liver involvement. In addition, biomarkers have not been studied in the Fontan population, hepatic CT scan has not been established to correlate with histopathology, and diffusion-weighted MRI is capable of quantifying fibrosis, but has not been evaluated in a Fontan setting.5
Indeed, the gold standard for assessment of liver disease is liver biopsy, usually performed via ultrasound-guided percutaneous needle biopsy. However, this is an invasive procedure with a potential for significant bleeding and elevated venous pressures, which may not be feasible for use in patients with ascites, and potentially prone to sampling error. Other alternative approaches are bioptic sampling during traditional or laparoscopic surgery, and TJLB. The latter is an important, safer alternative to the traditional percutaneous method and facilitates biopsy without causing liver capsule injury.13, 14 TJLB is usually performed in patients when liver biopsy is essential for diagnosis and management, but percutaneous biopsy is contraindicated due to out of range bleeding parameters (including International Normalized Ratio-INR > 1.7 times the control and/or platelet count <35 000), ascites, or other reasons (eg, small shrunken liver, extreme obesity, peliosis hepatis). Due to the high risk of thromboembolism in Fontan patients caused by slow blood flow and conduit insertion, antiaggregant or anticoagulant therapies are routinely prescribed. While available evidence suggests that antiplatelet agents alone may prove as effective as oral anticoagulants in primary prevention, anticoagulant therapy is generally preferred over the first 6 months following Fontan surgery, as well as in the case of previous thromboembolic events (secondary prevention).15, 16 TJLB is usually performed as an inpatient procedure and the patient sedated. ECG, blood pressure, and pulse oximetry are monitored throughout the procedure. In the case report described, the wire was negotiated along the (tortuous, dilated, and right-to-left) SVC-Fontan conduit-IVC and into the right hepatic veins. In this respect, angio-cardiac MRI played a crucial role in clarifying the complex anatomy of Fontan patients, thus allowing the usual limitations of echocardiography (poor views in surgically treated patients) and CT scan (ionizing radiations) to be overcome. Cardiac MRI is now considered the "gold standard" in evaluating adult CHD patients and is applied increasingly frequently and extensively.17 Cardiac MRI, although time-consuming, allows evaluation not only of the Fontan anatomy, but also of the single ventricle pumping chamber function (MRI cine images vs still images in CT) in one single session. Moreover, cardiac MRI is also preferable in view of the reported possible occurrence of seizures following iodinated contrast agent injection for CT (our patient takes medications for epilepsy, as reported in the text).
Our approach, that is doing an angio-cardiac MRI prior to liver biopsy in this specific setting, is unique and novel. It allows to delineate the abnormal anatomy of the heart and major vessels thus avoiding possible complications such as miss passage of the catheter and life-threatening arrhythmias. On balance, this combination approach minimizes the risk of periprocedural complications.
Conversely, MRI is not particularly useful in making a diagnosis as to the etiology of the liver disease. In fact, increased liver stiffness did not identify specific disease patterns from MRI, supporting the need for multimodality imaging to characterize liver disease in Fontan patients.18
The described TJLB procedure in Fontan patients is technically more challenging compared to that routinely performed in subjects with a normal anatomy, due to the longer and more tortuous route, surgery-related scars, frequent early Fontan conduit calcification, increased risk of life-threatening ventricular arrhythmias, and bleeding.
Arrhythmias may develop during catheter transit; thus, particular care should be taken to ensure that the catheter and/or wire do not form loops or enter the right atrium through the fenestration in the conduit, thus minimizing manipulation. The risk of arrhythmias, usually transient and subsiding once the catheter/wire reaches IVC, is significantly higher and potentially lethal in Fontan patients.19 Ready access to facilities for the treatment of arrhythmias and cardiac arrest is therefore mandatory.
Common TJLB complications (approx. 7%) are access site-related (neck pain, hematoma in the neck, carotid artery puncture, pneumothorax) or due to heart (ventricular arrhythmias) or liver injuries (hemorrhage). The reported mortality ranges from 0.09% in adulthood to 0.1% in childhood.20
In conclusion, liver dysfunction is a common medium and long-term complication in patients previously subjected to Fontan procedure linked to a need for hepatic check by means of liver biopsy. Indeed, some institutions following a large number of Fontan patients tend to endorse routine liver biopsy at a predetermined interval after Fontan surgery.21
Overall, TJLB approach may also be successfully performed in this specific and potentially more challenging clinical setting characterized by the complex anatomy and potential risk of life-threatening arrhythmias. Cardiac angio-MRI has proved to be a useful tool in guiding TJLB. The involvement of a mixed team of cardiologists committed to CHD patients and interventional radiologists expert in this field (heart team) played a pivotal role in ensuring a safe and successful outcome to the procedure.
ACKNOWLEDGMENTS
Published with written consent of the patient.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
PPB: involved in design and conceptualization of the case report, clinical care, analysis and interpretation of data, and drafting of manuscript. KPW: involved in clinical care, interpretation of data, and revision of manuscript for intellectual content. JGM: acquisition, description and interpretation of cardiac MRI and transjugular liver biopsy data, and revision of manuscript for intellectual content.