A case of congenital tuberculosis with a favorable outcome in a full term neonate
All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding information
This study was funded by Helsinki University Hospital Research Funds (personal grant (TV)).
Abstract
This case of congenital tuberculosis (TB) emphasizes that TB should be suspected in newborns whose parents are from areas with high incidence of TB or who present with symptoms of an infection unresponsive to wide-spectrum antibiotics.
1 INTRODUCTION
We describe a case of congenital tuberculosis in a term newborn showing signs of infection during the first days of life. A suspicion of the diagnosis was based on abnormal abdominal ultrasound findings of the newborn and infiltration typical for tuberculosis in the mother's chest X-ray.
Tuberculosis (TB) is a rare disease in Western countries, and the incidence of TB in Finland has decreased steadily during the last 10 years.1 In 2018, only one percent of the new cases (two cases) of TB in Finland were diagnosed in children under 15 years of age.1 Congenital TB is a rarity, and the incidence of the disease has not been well characterized.2, 3 However, even with appropriate treatment, congenital TB is associated with a high mortality rate of up to 40%, and the disease is fatal without treatment.2 The diagnosis of congenital TB is not straightforward. The clinical manifestations of the disease are nonspecific ranging from poor feeding to meningitis, and the onset of the disease can occur weeks after birth delaying the suspicion of the disease and initiation of treatment.2 Congenital TB can be transmitted to the fetus via placenta (ie, vertical transmission), from infected amniotic fluid swallowed by the fetus, or it can be transmitted through an infected genital lesion of genital TB during vaginal delivery.4, 5 We report a case of congenital TB in a newborn developing fever within the first days of life. Her mother had fever without other symptoms prior to the delivery and continued having fever spikes after delivery. The infection of the newborn was unresponsive to empirical wide-spectrum antibiotics. The diagnosis of congenital TB was unveiled by the abnormal abdominal ultrasound findings of the newborn and the mother's chest X-ray being suspicious for TB.
2 CASE PRESENTATION
A term girl was born via spontaneous vaginal delivery. The membranes were ruptured 7 hours before delivery with meconium-stained amniotic fluid. The mother was an immigrant from a country with high incidence of TB and has moved to Finland 2 years earlier. The pregnancy was followed up in a maternity health clinic and it was unremarkable, although no chest X-ray was taken despite her immigrant background. The mother had fever without other symptoms 5 days prior to the delivery. The delivery was unproblematic, and the newborn had Apgar scores of 9 and 10. Umbilical artery pH was 7.21, and base excess was −6.0 mmol/L. She was appropriate for gestational age weighing 3716 g. The newborn and her mother were admitted to the maternity ward. After the delivery, the mother had fever and the newborn appeared lethargic, but was feeding well. At the age of 36 hours, the newborn presented with mild irritability and fever, and was admitted to the neonatal intensive care unit (NICU). She went through a regular sepsis workup without lumbar puncture. Her white blood cell count was 19.6 × 109/L (normal: 9-38 × 109/L), C-reactive protein (CRP) was 228 nmol/L (normal: <29 nmol/L), and plasma glucose was 4.9 mmol/L. Clinical examination was unremarkable, and intravenous penicillin and netilmicin were administered for suspected infection. The mother was allowed to visit her child at the NICU after her influenza A and B antigen tests came out negative.
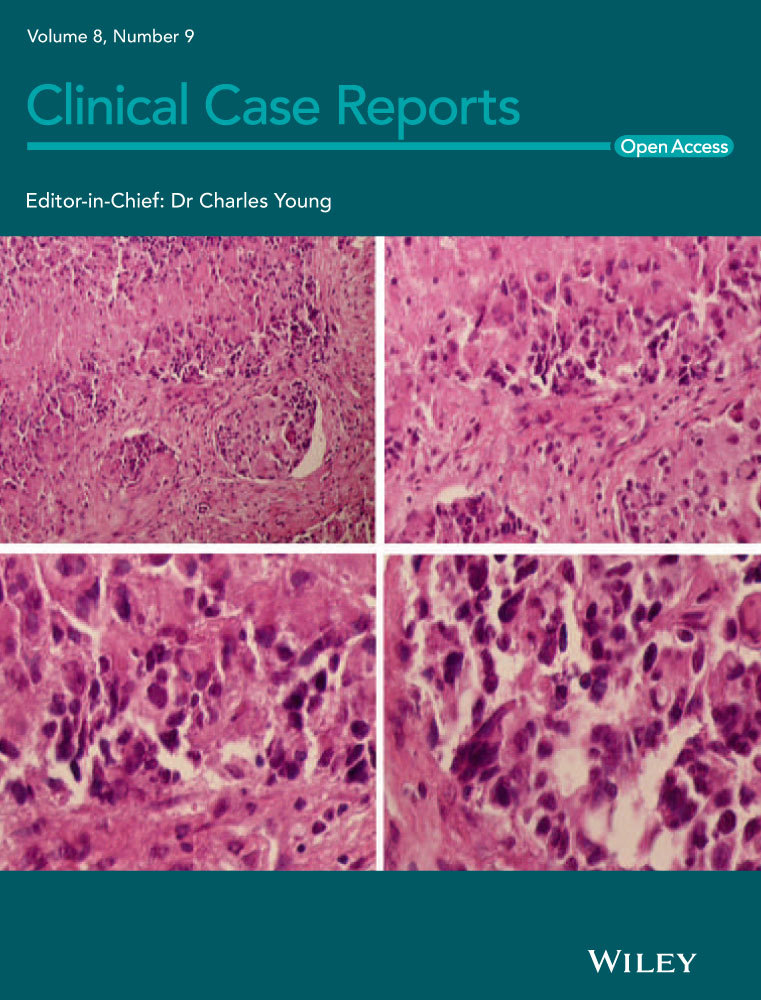
The newborn was closely monitored for 24 hours, and after showing no signs of sepsis, she was transferred to the maternity ward with antibiotics and paracetamol. Both the newborn and the mother continued to have fever. Subsequently, the newborn had unremarkable respiratory virus nucleic acid tests, viral stool culture, urine sample, and chest film. At the age of 5 days, the CRP level was 1110 nmol/L, white blood cell count was 18.0 × 109/L, and abdominal ultrasound showed an enlarged spleen with multiple small hypoechogenic lesions (Figure 1), which raised a suspicion of a hematogenously spread general infection. A pediatric infectious disease specialist was consulted and suggested that the mother should be screened for malaria and tuberculosis. The mother's chest X-ray showed an infiltration in the right apical lobe, which was further confirmed to be highly suspicious for TB with a computed tomography of the chest. Stomach fluid aspirate samples were obtained from the newborn infant, and treatment with rifampicin (RIF), pyrazinamide (PZA), isoniazid (INH), and ethambutol (EMB) was initiated. Lumbar puncture showed no signs of meningitis. The first interferon-gamma release assay could not be performed due to the limited number of white blood cells in the sample.

The smear of the stomach fluid aspirate showed no acid-fast bacilli, but Mycobacterium tuberculosis was diagnosed by nucleic acid test on the following day. The diagnosis of congenital TB was later confirmed by the culture, and the strain was fully sensitive to first-line TB drugs. There was a good clinical response to the treatment and CRP value normalized within 2 weeks from 1950 nmol/L, at highest. The newborn was closely monitored for 48 hours in the NICU and 6 days in a pediatric infectious disease unit and was then transferred to the pulmonary ward where the mother was treated for sputum smear-positive TB. The suggested treatment duration for the newborn was 6-9 months, and it was implemented as directly observed treatment. After discharge, the infant was followed at the outpatient clinic of the children's hospital.
At the age of 30 days, the girl was re-admitted to the children's hospital after presenting with fever since the previous evening without any other symptoms. Her laboratory results revealed anemia (hemoglobin 5.5 mmol/L, normal: 6.6-10.6 mmol/L), thrombocytopenia (149 × 109/L, normal: 200-450 × 109/L), and low white blood cell count (3.7 × 109/L). She went through sepsis workup including lumbar puncture, malaria samples, and echocardiography, which all were unremarkable. Brain magnetic resonance imaging (MRI) showed no sign of meningitis, whereas abdominal MRI showed enlarged mesenteric lymph nodes and hepatosplenomegaly (Figure 2). Her serum ALT, AST, and cystatin C were elevated to 1350 nmol/L, 2817 nmol/L, and 2.03 mg/L (normal: <667 nmol/L, <833 nmol/L, and <1.5 mg/L, respectively).6 Serum bilirubin level was 56 µmol/L (of which conjugated was 42 µmol/L). Lactate dehydrogenase was 15 µmol/L (2.3-6.3 µmol/L), and Coombs test was negative. Interferon-gamma release assay was positive.
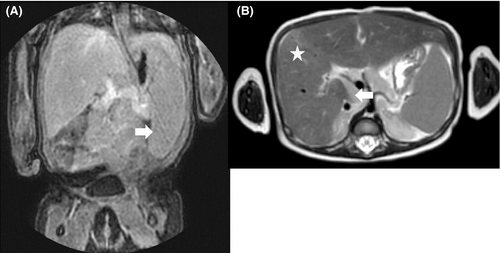
During hospital stay, she continued having fever spikes, but was otherwise in stable condition. CRP was 914 nmol/L at highest. Her interleukin-2 receptor level was 6810 kU/L (normal: 160-620 kU/L), and triglyceride level was 5.8 mmol/L (normal: 0.34-1.24 mmol/L). Her ferritin level was as high as 19 159 pmol/L (normal: 13-764 pmol/L). First, this prompted a suspicion of hemophagocytic lymphohistiocytosis (HLH), a disease known to associate with congenital TB.7 However, even though laboratory criteria were suggestive of HLH, the child's clinical presentation was not typical for HLH; thus, HLH disease needing specific therapy was considered unlikely. Fever, pancytopenia, and elevated liver enzyme levels were suspected to be a result of a RIF-related adverse effect. Thus, the treatment with RIF was discontinued and levofloxacin initiated instead. However, fever ended spontaneously before the first dose of levofloxacin and laboratory parameters started to improve. Thereafter, the initial combination was reconstituted 4 days later without any further complications. The girl was discharged at the age of 36 days. Thereafter, EMB and PZA treatments were discontinued after 6 and 8 weeks of treatment, respectively. RIF and INH treatments were continued for the total of 9 months. The girl was followed up in the outpatient clinic of the children's hospital and showed complete recovery from the infection. The child grew well and reached developmental milestones within normal range. The hepatosplenomegaly seen in abdominal MRI had normalized in a follow-up MRI scan performed at 8 months after initiation of the treatment.
3 DISCUSSION
Congenital TB is a rare but fatal disease, which needs to be diagnosed as early as possible to avoid fatal outcomes. In a newborn, the clinical presentation of the disease is nonspecific, which often delays the diagnosis.1 In this case, the symptoms were nonspecific; the newborn had fever, but was otherwise in good clinical condition, which was confusing for the clinicians treating her. Congenital TB in newborns presenting with fever or other symptoms of general illness, especially if the disease is unresponsive to wide-spectrum antibiotics. Additionally, the case emphasizes the need to screen all the immigrants from countries with a high risk of TB with a chest X-ray.
Our case presented with splenomegaly and multiple splenic lesions, which suggested that the infection was transmitted intrauterine via hematogenous spread. Notably, the single examination that suggested TB diagnosis was the mother's chest X-ray. She was an immigrant coming from a country with a very high incidence of TB, albeit she had lived in Finland for 2 years. This case reminds readers that a rare disease can emerge in a country with a very low TB incidence through immigration. The Finnish national guideline suggests that immigrants coming from countries with very high incidence of TB should be screened for pulmonary TB with a chest X-ray, an intervention with a minimal radiation dose.8 For reasons not known, the protocol was not followed in her case. Importantly, the chest X-ray taken after she gave birth was highly informative; thus, the infection of the newborn would have been prevented by following the guideline.
Pulmonary TB is transmitted via air, whereas it is highly unlikely that a newborn with TB without respiratory symptoms or aerosol-producing procedures transmits the disease to the environment through air.9 The transmission of TB from a newborn requires close contact with the newborn's secretions. Previously, this has been reported in an intensive care unit setting, where appropriate precautions were not followed due to an equivocal diagnosis.10 In our case, the newborn had no pulmonary findings and was in good condition, and she was followed without interventions for 2 days in the NICU. The mother had sputum smear-positive TB and was not treated during the first week after she gave birth. Both the mother and the newborn spent 5 days in the maternity ward without appropriate preventive measures. Consequently, we contacted 72 newborns who were possibly exposed to the infected mother. Of the 72 exposed newborns, 16 (22%) were evaluated in pediatric outpatient clinic. Ten (63%) newborns who were exposed to TB (ie, had been in the same facilities as the infected mother) received a prophylactic regimen of INH.
Congenital TB is a fatal disease without treatment, and the mortality rate is high even with an appropriate treatment. In our case, the diagnosis was made relatively swiftly, which resulted in a favorable primary response, and the newborn recovered well from the infection.
4 CONCLUSIONS
This case report describes congenital TB in a newborn presenting with symptoms within the first days of life. Congenital TB should be suspected in newborns whose parents are from areas with high incidence of TB and who present with symptoms of an infection or generalized illness. A suspicion of TB should be entertained when an adequate response to wide-spectrum antibiotics is not obtained in a few days. In our case, the diagnosis of congenital TB was suspected after the abdominal ultrasound of the newborn showed splenomegaly and multiple lesions in the spleen, and the mother's chest X-ray showed a pulmonary lesion suspicious for TB. Thus, the case emphasizes the need for chest X-ray screening for pregnant women coming from countries with high TB incidence. Chest X-ray is the primary instrument in diagnosing pulmonary TB, which is the contagious form of TB and should be diagnosed before the delivery to prevent the transmission not only to the mother's own baby, but to all the other newborns in the maternity ward.
CONFLICT OF INTEREST
The authors have no conflict of interest.
AUTHOR CONTRIBUTIONS
TV, TN, SK, TT, JA, and MM: treated the patient, wrote and commented on the manuscript, and approved the final version of the manuscript.