A case report of periprosthetic fracture left proximal humerus with radial nerve palsy following pectoralis major repair
The work was carried out at Princess of Wales Hospital, ABM University Health Board, Bridgend, Mid Glamorgan, United Kingdom.
Key Clinical Message
Primary repair of pectoralis major tendon with bony tunnels and anchor sutures in the proximal humerus creates a potential weakness and stress riser leading to increased risk of periprosthetic fracture and nerve damage at the site of weakness with subsequent injury, if not allowed to heal satisfactorily with adequate period of rest.
Introduction
Pectoralis major (PM) tendon avulsion is an uncommon injury of the shoulder. It usually occurs in younger people who are otherwise healthy and active. Violent eccentric contraction of PM in a load bearing arm, such as during weight lifting, can cause avulsion of the tendon. The tendon inserts into the lateral lip of the bicipital groove in the proximal humerus. Most commonly, the tendon avulses from this insertion but occasionally the injury can be from the musculotendinous junction, where primary repair is difficult 1.
Operative repair of the tendon can be accomplished by drilling bony tunnels and using suture anchor. This allows the tendon to be approximated to the insertion and allows healing to occur. The tendon typically takes 6 weeks to heal from the time of repair. In order to protect the fixation, the postsurgical rehabilitation protocol requires avoidance of contact sports or weight lifting for 3–6 months 2.
Periprosthetic fractures can occur where fixation techniques leave a stress riser. By fixing a PM tendon with internal fixation there is a potential stress riser in the relatively weak metaphyseal-diaphyseal junction in the proximal humerus. To date, there has been only one reported case of periprosthetic fracture following PM tendon repair. This case describes a 45-year-old patient who fell from standing height and sustained a closed, neurovascularly intact periprosthetic proximal humeral fracture. Eight weeks prior to the injury a PM tendon repair had been completed through the creation of suture tunnels through a bone trough to provide a hold for a modified Kessler suture. In this case the perioperative findings demonstrated that the new fracture was through the bone trough, with the PM tendon repair intact 3.
The aim of this case report is to report occurrence of proximal humeral fracture at the site of a PM tendon repair. This case is unique as the repair used bone anchors and bone tunnels for fixation of the PM tendon. There was also a dense radial nerve palsy associated with the peri-prosthetic fracture. In this case a nonoperative strategy is discussed, and the results demonstrated.
Case History
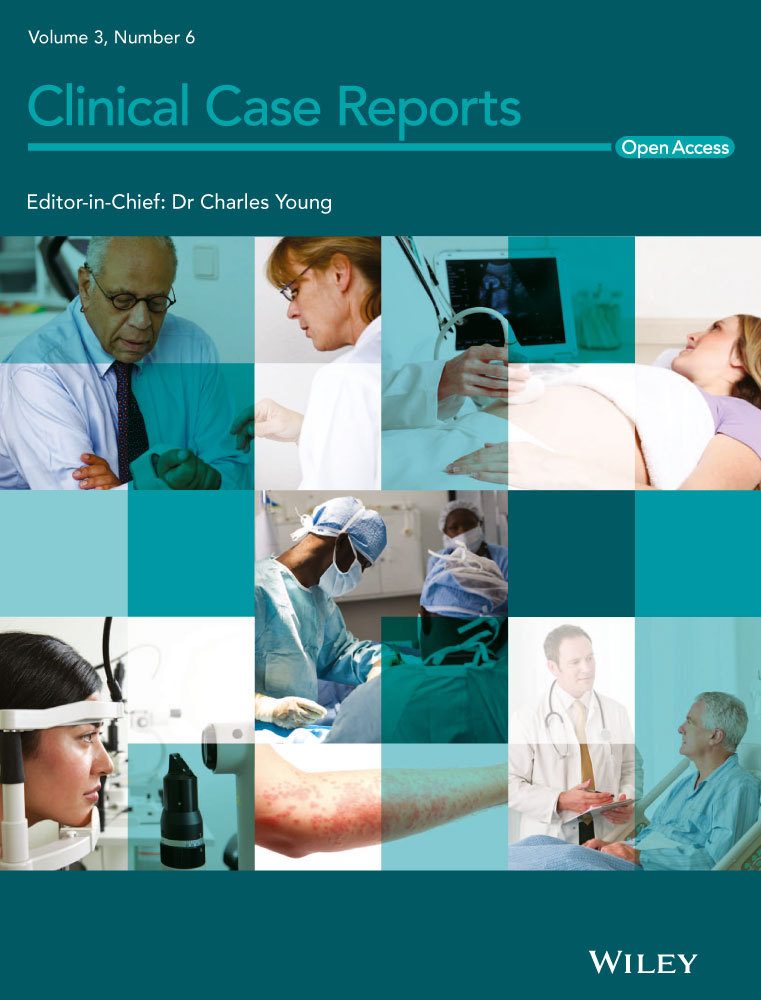
A 33-year-old male patient presented with a suspected left PM tendon avulsion from the humeral insertion in September 2011. The injury was sustained during a rugby tackle. He had no significant medical history and was keen to return to sport. MRI confirmed a PM tendon avulsion from the humeral insertion (Fig. 1).
The patient underwent primary repair of the tendon 2 weeks later. This was performed through a delto-pectoral approach. There was a small remnant of the tendon still attached to the lateral ridge of the bicipital groove, this was not sufficient for a direct end-to-end repair. The repair was completed in two parts. First, three bony tunnels were created with a 2 mm drill from lateral to medial on the lateral ridge of the bicipital groove. These were used to secure the deeper portion of the tendon. The superficial portion of the tendon was repaired using 3 Mitec Anchors (G11 QUICKANCHOR PLUS; DePuy Mitek Inc. Raynham, MA USA).
The postoperative plan is detailed in Table 1. The patient was instructed to remain in a sling to limit active and passive external rotation, forward flexion, and abduction for 4 weeks. The patient received physiotherapy to mobilize the shoulder with a strict instruction to abstain from contact sports and weight lifting for 3 months.
| Postoperative mobilization strategy | |
|---|---|
| Weeks | Activity |
| 0–4 | Nil, rest in sling |
| 4–12 | Active and passive movements with physiotherapy |
| 12+ | Full range of motion, return to sport |
Unfortunately, 3 months following the primary repair the patient attended the Emergency Department with an injury to the left proximal humerus. He had recommenced contact sports earlier than instructed and had sustained an injury while playing rugby. His arm was pulled and twisted forcefully in a rugby tackle. On examination he had a deformed arm with a neurological deficit in the territory of the radial nerve. Clinically, the PM tendon repair had healed and was functionally sound.
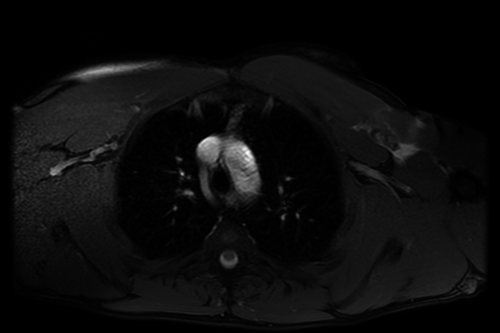
X-ray images demonstrated a spiral peri-prosthetic fracture at the site of the metal anchors in lateral proximal humerus (Fig. 2a,b). The neurological deficit was investigated at 2 months following the second injury with electromyogram and nerve conduction studies. These demonstrated a severe left radial neuropathy proximal to the origin of branch to brachioradialis. The radial nerve was in functional continuity.
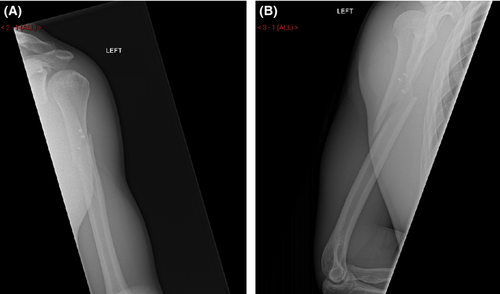
The periprosthetic fracture was treated nonoperatively in a humerus brace with radial nerve palsy (wrist drop) splint. He was referred to physiotherapy for passive mobilization of the wrist and fingers while waiting for the radial nerve to recover. Over the next 6 months, the periprosthetic fracture healed and the radial nerve recovered completely (Fig. 3a,b).
Outcome and Follow-Up
At 6-month clinic follow-up the patient had radiological union of his periprosthetic fracture and complete functional recovery of his radial nerve palsy. At this point he was discharged to his General Practitioner and has had no further issues with his left arm.
Four years following injury he is working as a store man. His job requires lifting heavy weight from time to time. He has full range of painless shoulder movements and his Oxford Shoulder Score is 48 and DASH score is 24 indicating an excellent recovery from both injuries. He does not play rugby anymore but regularly goes to gym for weight training and has no restrictions or pain in the shoulder or the arm.
Discussion
Periprosthetic fracture through the bony tunnels and metal anchors is a rare complication of fixation of PM tendon avulsions. The combination of a periprosthetic fracture with radial nerve palsy has not been reported in literature in our knowledge.
As described in the introduction, there is one previously published case of proximal shaft of humerus fracture following PM tendon repair 3. This has significant difference from the case described as the management of the initial injury did not include the use of suture anchors and the proximal humeral fracture was fixed with a locking plate. However, both cases have demonstrated excellent functional results and outcomes.
The use of suture anchors has been widely described for reattaching soft tissue to bone. Suture anchors have been used around most joints, including Achilles tendon repairs, extensor tendon repairs around the knee, shoulder reconstructions and biceps tendon repairs 4-7. Complications are uncommon, but typically involve anchor pull-out or osteolysis 8. Periprosthetic fracture is very rare, with fractures around a suture anchor described in only one case with a patella fracture following patellofemoral ligament reconstruction 9.
In this case it is difficult to identify the precise causation of the periprosthetic fracture. The use of suture anchors is unlikely to have contributed significantly to the risk of fracture. However, any intervention that breaches the cortex or reduces the cross-sectional area of the bone will introduce a stress riser which will predispose to fracture. In addition, the patient did not adhere to his original postoperative instructions to rest his tendon repair. While the intention of these instructions was to protect the repair itself it is probable that additional rest would have allowed the bone to remodel and reduce the risk of periprosthetic fracture.
In this case, the nerve injury associated with the periprosthetic fracture was found to be a neuropraxia type injury. This is classically described as a “lesion in continuity”, where the nerve is placed under traction causing temporary compromise. While very worrying for the patient and clinician, these lesions do resolve with conservative management and are the most common form of nerve injury associated with a closed fracture. As in this case, we would recommend additional investigation if the neurological findings do not resolve with electromyogram and nerve conduction studies, with a low threshold to proceed to open exploration if there is indication of nerve discontinuity 10, 11.
Overall, the patient made a good recovery following the pectoralis tendon repair. Future patients will be counseled with the evidence and experience of this case to abstain from contact sports and weight lifting until the tendon rupture has healed and the risk of fracture is significantly diminished.
Learning Points
- Primary repair of the bulky muscle/tendon unit like PM with bony tunnels and anchor sutures in a proximal humerus creates a weak area in the proximal shaft of the humerus. This creates the potential for a periprosthetic fracture.
- The patients sustaining PM Tendon avulsion from its insertion requiring repair are young and they should to be warned of this potentially serious complication. The length of time the young active patient should avoid the contact sports is debatable, but is generally recommended for at least 3 months
- Posttraumatic nerve injury, particularly the radial nerve injury with humerus shaft fracture is a Neuropraxia type of injury – lesion in continuity – and the treatment is mostly conservative/expectant if the fracture is treated nonoperatively. If the fracture is decided to be treated operatively, the affected nerve is explored to make sure that the nerve is physically intact.
Conflict of Interest
None declared.