Associations of Social Vulnerability and Race-Ethnicity With Gastrointestinal Cancers in the United States
Funding: The authors received no specific funding for this work.
ABSTRACT
Background
National social determinant of health (SDoH) studies on gastrointestinal cancers (GIC) have observed single GIC-types for surgery but not across all GIC-types, non-surgical treatments outcomes, or mortality. The Social Vulnerability Index (SVI), a validated large-data SDoH-tool, quantifiably characterizes the interrelatedness of SDoH-impact through dynamic, region-contextualized measures.
Methods
This retrospective cohort study assessed GIC patients (20+ years) between 2013 and 2017 from the Surveillance, Epidemiology, and End Results (SEER) database for total and subcomponent social vulnerability associations across 15 SDoH-variables encompassing themes of socioeconomic status, minority-language status, household composition, and housing-transportation measured by the Social Vulnerability Index (SVI). These are measured and contextualized from all US counties. Univariate logistic and linear regressions of these vulnerability associations with treatment receipt (chemotherapy, radiation, primary surgery) and survival were performed for the entire cohort and across race/ethnicity strata.
Results
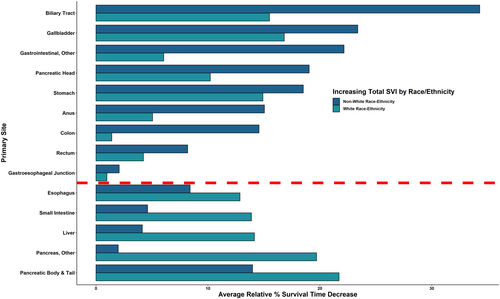
With increasing overall social vulnerability, 287,248 patients (162,387 [56.5%] male; 185,250 [64.6%] white) demonstrated decreased receipt of chemotherapy (lowest, pancreas-OR, 0.90; 95% CI, 0.88–0.93), radiotherapy (hepatic-OR, 0.87; 95% CI, 0.85–0.89) and surgery (esophagus-OR, 0.90; 95% CI, 0.87–0.92) for 13/14, 10/14, and 8/14 GIC-types, respectively. Survival period decreases upwards of 21.3% (biliary tract: 6.9–5.4 months) were observed across 7/14 GICs. Treatment receipt and survival decreases were exacerbated for non-White patients for 9/14 GICs. Socioeconomic status, minority-language, household composition, and housing-transportation vulnerabilities differentially contributed to these trends.
Discussion
Social vulnerability was associated with worse prognostic and treatment disparities, with certain SDoH-types differentially contributing to these detrimental trends per GIC-type while associations were exacerbated among non-White race/ethnic patients. These real-world contexts present actionable targets for further initiatives to combat GIC disparities.
1 Introduction
With rising worldwide morbidity and mortality of gastrointestinal cancers (GIC), characterization of the factors associated with this detrimental trend has become a topic of increased interest [1, 2]. In addition to patient and clinical factors that contribute to a growing GIC disease burden, social determinants of health (SDoH) such as socioeconomic status, race-ethnicity, transportation distance to a health provider, as well as other factors, have been identified as important drivers of inequalities in the diagnosis, delivery, and prognosis of patients. To this point, several studies have leveraged large-data approaches to define the impact of SDoH-related disparities relative to a range of disease processes [3-5].
While SDoH can impact a range of health care metrics, inequalities in social factors have disproportionate effects on patients receiving surgical treatment, especially among racial-ethnicity minority patients [6-10]. In particular, the interactions between socioeconomic status and race-ethnicity can have a modifying or synergistic effect on utilization and outcomes following surgical and non-surgical interventions [3, 11]. For example, Bakkila et al. reported a decrease in chemotherapy and radiation therapy utilization among Black versus White patients with a GIC diagnosis [7]. Similarly, Reif de Paula et al. noted that adjuvant chemotherapy utilization differed among patients with pT4N0M0 colon cancer who had Medicare/Medicaid insurance or were uninsured [12]. Prior studies have primarily focused on race/ethnicity or insurance-based disparities. However, SDoH-related disparities related to non-surgical treatment modalities for GICs have not been investigated at the national level.
In order to assess broader, real-world implications of SDoH [3, 13-15], nuanced population-based tools are needed to assess social factors associated with health care outcomes. The Centers for Disease Control and Prevention—Social Vulnerability Index (SVI) is a US census-validated tool that measures community-contextualized SDoH-factors [16]. SVI encompasses themes of socioeconomic status (SES), minoritized race-ethnicity and English-language proficiency (ML), household composition (HH), and housing-transportation status (HT). Prior studies have utilized the total SVI score to assess influence of overall social vulnerability with surgery receipt and post-resection outcomes [13, 17, 18].
Characterization of how SDoH-themes may differentially impact multi-modal treatment and prognostic outcomes among patients with GIC has not been elucidated. Therefore, the objective of the current study was to define the association of SVI with utilization of surgical and non-surgical treatment of GIC patients. We sought to examine how the different SVI subthemes (i.e., SES, ML, HH, and HT) may differentially affect treatment and prognosis of patients with GIC treated in the United States. Furthermore, we aimed to elucidate how the impact of the social vulnerability would differ among White and Non-White patients diagnosed with GIC.
2 Methods
This retrospective cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. The Northwestern University IRB deemed this research as exempt from needing ethics approvals or waiver of informed consent; the databases queried consist of publicly available, de-identified data.
2.1 Data Sources and Variables
Data on SVI were extracted relative to ranked scores along fifteen census-level social factors across four SDoH themes of socioeconomic status (poverty, unemployment, income level, high school diploma status), minority status-language (minority status, proficiency with English), household composition (household members 65+ years, household members ≤ 17 years, disability status, single-parent status), and housing-transportation (multi-unit structure, mobile homes, crowding, no vehicle, group quarters). Based on 2013–2018 CDC-SVI documentation [16], SVI-theme subscores were differentially weighed to formulate the total composite score and assigned different weights based on sociodemographic-census data related to the designated area (Figure S1). Total and SVI-theme scores were based on relative social vulnerabilities of a particular census tract among all 72,158 US-census tracts, ranging from 0 to 1; 0 represented the lowest social vulnerability and 1 represented the highest. Full details regarding formulation and the differential weighing incorporated in SVI-scores can be found in Data S1.
The National Cancer Institute-Surveillance, Epidemiology, and End Results Program (NCI-SEER) database contains datasets of patient variables, clinical characteristics, treatment modalities, and prognostic outcomes (see Data S1 for specific variables). SVI scores were matched to SEER-patient data based on county of residence upon diagnosis. County-assigned scores were generated by weighted score means per population density of each census tract within the county. A schematic workflow of this linkage is provided in Figure S2; descriptive details regarding this process of geocode linkage can be found in Data S1.
2.2 Population Definitions
The SEER database was queried for adult (> 20 years) patients diagnosed with GIC between 2013 and 2017 using International Classification of Diseases for Oncology, Third Edition (ICD-O-3) topographic codes [C15.0—C26.9]. Gastrointestinal stromal tumors (GIST) and neuroendocrine tumors (NET) identified based on SEER-generated histologic categories were excluded to homogenize the histological representation of primary site tumors.
Missing data entries due to lacking geographical information allowing SVI-variable linkage were excluded from all analyses. Unavailable data for a specified outcome necessitated for an analysis were excluded solely for that respective calculation. Survival/mortality was considered as “all-cause mortality” per SEER-data documentation.
2.3 Statistical Methods
SVI scores were categorized into quintiles based on SVI scores within each disease class. The relative-SVI quintiles were defined as “< 20”, “20–39.99”, “40–59.99”, “60–79.99”, “80–99.99”, which represented the relative percentiles per disease class (e.g., within a certain GIC diagnosis, patients with the lowest SVI scores are grouped into the “< 20” quintile group). Indicated chemotherapy, radiotherapy, and primary surgical resection within each GIC-type were analyzed using univariate logistic regression across the relative-SVI quintiles (representative of the differentially weighted aggregate of the 15 SDoH-variables), as well as each of the four SVI themes.
In assessing the impact of overall SVI and SVI-theme quintiles, differences in the mean months of survival for lowest and highest SVI-scored quintiles were calculated within each GIC type. Trend significance was assessed by linear regression across all data points relative to SVI quintiles for months survival. For each relative-SVI quintile, the median, interquartile range (IQR), and 1.5-times the IQR (i.e., boxplot) was calculated. Means, standard deviations, and ranges for months survival per quintile were also calculated across GIC types. In addition, Kaplan–Meier survival analyses of the entire GIC cohort with log-rank significance testing was also conducted between the lowest and highest total SVI quintile groups.
Odds of receiving a certain treatment were analyzed with univariate logistic regressions across relative-SVI quintiles for increasing levels of total SVI and each SVI-theme. References groups for odds ratios and 95% confidence intervals calculated for each SVI-association were represented by the lowest relative SVI-quintile (i.e., lowest social vulnerability group) with subsequent ordinal variable values sequentially matching each increasing level of relative quintile (i.e., “< 20” quintile was set as the reference, increasing levels of comparator values were ordinally organized by “20–39.99”, “40–59.99”, “60–79.99”, and “80–99.99” in sequence). Binary outcome delineations for outcome variables were utilized for whether a patient received surgical resection, radiation therapy, or chemotherapy. For race-ethnicity stratified analyses, similar techniques were performed independently regarding months of survival and treatment receipt within cohorts of patients that were (Non-Hispanic) White and Non-White (Hispanic, Black, Asian or Pacific Islander, Native American, or Other).
Statistical significance was set as p < 0.05. Two-sided p-values were reported for analyses. All statistical analyses were conducted in R version 4.2.1.
3 Results
Among 287,248 patients with GIC who were included in the analytic cohort, most patients were between 65 and 84 years of age (n = 137,674, 47.9%), male (n = 162,387, 56.5%), and self-identified as non-Hispanic White (n = 185,450, 64.6%) (Table 1). The primary GIC diagnosis varied considerably within the study population (esophagus, n = 16,276, 5.6%; gastroesophageal junction, n = 7961, 2.8%; stomach, n = 15,261, 5.3%; liver, n = 31,105, 10.8%; pancreas, n = 49,798, 17.3%; biliary tract, n = 10,510, 3.6%; gallbladder, n = 4550, 1.6%; small intestine, n = 3075, 1.1%; colon, n = 97,990, 34.1%; rectum, n = 40,351, 14.0%; anus, n = 7274, 2.5%; gastrointestinal-other, n = 3097, 1.1%). In assessing social vulnerability, total SVI scores ranged from 0.000 to 0.947 (subthemes: socioeconomic status-SVI: 0.000–0.976; minority status and language-SVI: 0.002–0.945; household composition-SVI: 0.091–0.971; housing and transport-SVI: 0.051–0.942) (Table 1). Treatment of patients with GIC also varied (chemotherapy, n = 123,822, 43.1%; radiation therapy, n = 50,103, 17.4%; surgical resection, n = 146,487, 52.9%) (Table 1). Clinicodemographic distribution across each SVI-subtheme was also varied (Tables S1–S4).
| Total SVI Score | p | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Overall, N = 287,248 (100%) | 0.000–0.199, N = 2238 (0.8%) | 0.200–0.399, N = 52,888 (18%) | 0.400–0.599, N = 137,250 (48%) | 0.600–0.799, N = 88,548 (31%) | 0.800–0.999, N = 6324 (2.2%) | |
| Age | < 0.001 | ||||||
| 20–44 years | 12,110 (4.2%) | 92 (4.1%) | 2138 (4.0%) | 5667 (4.1%) | 3956 (4.5%) | 257 (4.1%) | |
| 45–64 years | 105,661 (37%) | 802 (36%) | 18,178 (34%) | 50,629 (37%) | 33,628 (38%) | 2424 (38%) | |
| 65–84 years | 137,674 (48%) | 1108 (50%) | 25,947 (49%) | 65,374 (48%) | 42,115 (48%) | 3130 (49%) | |
| 85+ years | 31,803 (11%) | 236 (11%) | 6625 (13%) | 15,580 (11%) | 8849 (10.0%) | 513 (8.1%) | |
| Sex | < 0.001 | ||||||
| Male | 162,387 (57%) | 1289 (58%) | 29,484 (56%) | 77,622 (57%) | 50,295 (57%) | 3697 (58%) | |
| Female | 124,861 (43%) | 949 (42%) | 23,404 (44%) | 59,628 (43%) | 38,253 (43%) | 2627 (42%) | |
| Race | < 0.001 | ||||||
| White | 185,450 (65%) | 1928 (86%) | 43,799 (83%) | 87,604 (64%) | 48,714 (55%) | 3405 (54%) | |
| Hispanic | 37,956 (13%) | 180 (8.0%) | 2640 (5.0%) | 14,144 (10%) | 19,397 (22%) | 1595 (25%) | |
| Black | 34,239 (12%) | 40 (1.8%) | 3578 (6.8%) | 18,064 (13%) | 11,630 (13%) | 927 (15%) | |
| Asian or Pacific Islander | 26,267 (9.1%) | 43 (1.9%) | 2440 (4.6%) | 15,994 (12%) | 7671 (8.7%) | 119 (1.9%) | |
| Native American | 1866 (0.6%) | 32 (1.4%) | 194 (0.4%) | 756 (0.6%) | 624 (0.7%) | 260 (4.1%) | |
| Unknown | 1470 (0.5%) | 15 (0.7%) | 237 (0.4%) | 688 (0.5%) | 512 (0.6%) | 18 (0.3%) | |
| Region | < 0.001 | ||||||
| Midwest | 26,674 (9.3%) | 145 (6.5%) | 9788 (19%) | 16,170 (12%) | 571 (0.6%) | 0 (0%) | |
| Northeast | 45,747 (16%) | 1021 (46%) | 21,655 (41%) | 17,825 (13%) | 5246 (5.9%) | 0 (0%) | |
| South | 66,701 (23%) | 779 (35%) | 7730 (15%) | 32,662 (24%) | 22,925 (26%) | 2605 (41%) | |
| West | 148,126 (52%) | 293 (13%) | 13,715 (26%) | 70,593 (51%) | 59,806 (68%) | 3719 (59%) | |
| Primary site | < 0.001 | ||||||
| Anus | 7274 (2.5%) | 70 (3.1%) | 1386 (2.6%) | 3570 (2.6%) | 2127 (2.4%) | 121 (1.9%) | |
| Biliary tract | 10,510 (3.7%) | 104 (4.6%) | 2022 (3.8%) | 5041 (3.7%) | 3101 (3.5%) | 242 (3.8%) | |
| Colon | 97,990 (34%) | 766 (34%) | 18,130 (34%) | 46,369 (34%) | 30,470 (34%) | 2255 (36%) | |
| Esophagus | 16,276 (5.7%) | 148 (6.6%) | 3384 (6.4%) | 7926 (5.8%) | 4464 (5.0%) | 354 (5.6%) | |
| Gallbladder | 4550 (1.6%) | 24 (1.1%) | 787 (1.5%) | 2146 (1.6%) | 1490 (1.7%) | 103 (1.6%) | |
| Gastroesophageal junction | 7961 (2.8%) | 69 (3.1%) | 1652 (3.1%) | 3854 (2.8%) | 2255 (2.5%) | 131 (2.1%) | |
| Gastrointestinal, other | 3097 (1.1%) | 20 (0.9%) | 611 (1.2%) | 1392 (1.0%) | 1017 (1.1%) | 57 (0.9%) | |
| Liver | 31,105 (11%) | 177 (7.9%) | 4554 (8.6%) | 15,602 (11%) | 10,020 (11%) | 752 (12%) | |
| Pancreas, other | 13,369 (4.7%) | 115 (5.1%) | 2645 (5.0%) | 6296 (4.6%) | 4043 (4.6%) | 270 (4.3%) | |
| Pancreatic body and tail | 13,860 (4.8%) | 112 (5.0%) | 2879 (5.4%) | 6792 (4.9%) | 3828 (4.3%) | 249 (3.9%) | |
| Pancreatic head | 22,569 (7.9%) | 202 (9.0%) | 4436 (8.4%) | 10,944 (8.0%) | 6539 (7.4%) | 448 (7.1%) | |
| Rectum | 40,351 (14%) | 327 (15%) | 7561 (14%) | 18,829 (14%) | 12,699 (14%) | 935 (15%) | |
| Small intestine | 3075 (1.1%) | 27 (1.2%) | 626 (1.2%) | 1464 (1.1%) | 905 (1.0%) | 53 (0.8%) | |
| Stomach | 15,261 (5.3%) | 77 (3.4%) | 2215 (4.2%) | 7025 (5.1%) | 5590 (6.3%) | 354 (5.6%) | |
| TNM/AJCC Combined stage | 0.010 | ||||||
| Stage I-III | 175,818 (67%) | 1347 (66%) | 32,333 (67%) | 85,053 (67%) | 53,271 (67%) | 3814 (67%) | |
| Stage IV and Above | 86,936 (33%) | 706 (34%) | 16,257 (33%) | 41,451 (33%) | 26,659 (33%) | 1863 (33%) | |
| Primary surgery performed | < 0.001 | ||||||
| No surgery | 130,562 (47%) | 1014 (47%) | 23,766 (46%) | 62,279 (47%) | 40,600 (48%) | 2903 (48%) | |
| Surgery | 146,487 (53%) | 1145 (53%) | 27,503 (54%) | 70,301 (53%) | 44,406 (52%) | 3132 (52%) | |
| Radiation therapy performed | < 0.001 | ||||||
| No therapy | 237,145 (83%) | 1826 (82%) | 42,910 (81%) | 112,703 (82%) | 74,464 (84%) | 5242 (83%) | |
| Therapy | 50,103 (17%) | 412 (18%) | 9978 (19%) | 24,547 (18%) | 14,084 (16%) | 1082 (17%) | |
| Chemotherapy performed | < 0.001 | ||||||
| No therapy | 163,426 (57%) | 1129 (50%) | 28,868 (55%) | 77,034 (56%) | 52,624 (59%) | 3771 (60%) | |
| Therapy | 123,822 (43%) | 1109 (50%) | 24,020 (45%) | 60,216 (44%) | 35,924 (41%) | 2553 (40%) | |
| Vital status on last follow-up | < 0.001 | ||||||
| Alive | 153,472 (53%) | 1261 (56%) | 29,152 (55%) | 73,677 (54%) | 46,221 (52%) | 3161 (50%) | |
| Dead | 133,776 (47%) | 977 (44%) | 23,736 (45%) | 63,573 (46%) | 42,327 (48%) | 3163 (50%) | |
3.1 Impact of SVI on Treatment of GIC
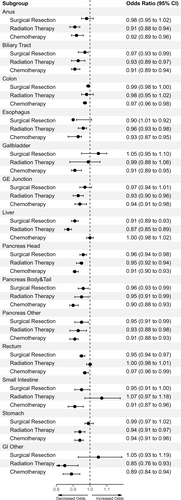
Social vulnerability was strongly associated with likelihood to receive chemotherapy, radiation therapy, as well as surgical resection. Specifically, across many GIC diagnoses, patients residing in counties with higher total SVI scores had decreased odds of receiving surgical resection on 8/14 GIC types (lowest, esophagus: OR, 0.90; 95% CI, 0.87–0.92) (see Data S1 for all significant sites) (Figure 1, Table 2). Of note, the subthemes that had the largest impact on decreased likelihood to undergo surgical resection included increasing vulnerability in household composition and socioeconomic status, followed by housing-transportation and then minority-language status (Table 2).
| Primary classificationa | Characteristic | Surgical resection | Radiation therapy | Chemotherapy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||
| Anus | Total | 0.98 | 0.95, 1.02 | 0.366 | 0.91 | 0.88, 0.94 | < 0.001 | 0.92 | 0.89, 0.96 | < 0.001 |
| Socioeconomic status | 1.00 | 0.96, 1.03 | 0.803 | 0.93 | 0.90, 0.97 | < 0.001 | 0.93 | 0.90, 0.97 | < 0.001 | |
| Minority-language status | 0.99 | 0.96, 1.02 | 0.479 | 0.90 | 0.87, 0.94 | < 0.001 | 0.93 | 0.90, 0.97 | < 0.001 | |
| Household composition | 1.00 | 0.96, 1.03 | 0.907 | 1.04 | 1.00, 1.07 | 0.071 | 1.01 | 0.97, 1.04 | 0.774 | |
| Housing-transportation | 0.98 | 0.95, 1.01 | 0.191 | 0.92 | 0.89, 0.96 | < 0.001 | 0.95 | 0.91, 0.98 | 0.003 | |
| Biliary tract | Total | 0.97 | 0.93, 0.99 | 0.042 | 0.93 | 0.89, 0.97 | 0.001 | 0.91 | 0.89, 0.94 | < 0.001 |
| Socioeconomic status | 0.95 | 0.92, 0.98 | 0.003 | 0.96 | 0.92, 1.00 | 0.045 | 0.94 | 0.91, 0.96 | < 0.001 | |
| Minority-language status | 1.05 | 1.01, 1.08 | 0.010 | 0.92 | 0.88, 0.96 | < 0.001 | 0.94 | 0.91, 0.96 | < 0.001 | |
| Household composition | 0.92 | 0.89, 0.95 | < 0.001 | 1.03 | 0.99, 1.08 | 0.096 | 0.98 | 0.96, 1.01 | 0.265 | |
| Housing-transportation | 0.96 | 0.93, 0.99 | 0.014 | 0.89 | 0.86, 0.93 | < 0.001 | 0.91 | 0.89, 0.94 | < 0.001 | |
| Colon | Total | 0.99 | 0.98, 1.00 | 0.118 | 0.98 | 0.95, 1.02 | 0.339 | 0.97 | 0.96, 0.98 | < 0.001 |
| Socioeconomic status | 1.0 | 0.98, 1.01 | 0.393 | 1.01 | 0.97, 1.04 | 0.630 | 0.98 | 0.97, 0.99 | < 0.001 | |
| Minority-language status | 0.97 | 0.96, 0.98 | < 0.001 | 0.90 | 0.87, 0.94 | < 0.001 | 0.96 | 0.95, 0.97 | < 0.001 | |
| Household composition | 1.02 | 1.01, 1.04 | < 0.001 | 1.07 | 1.04, 1.11 | < 0.001 | 1.00 | 1.0, 1.01 | 0.380 | |
| Housing-transportation | 0.99 | 0.98, 1.00 | 0.063 | 0.98 | 0.94, 1.01 | 0.193 | 0.97 | 0.96, 0.98 | < 0.001 | |
| Esophagus | Total | 0.90 | 0.87, 0.92 | < 0.001 | 0.96 | 0.93, 0.98 | < 0.001 | 0.93 | 0.90, 0.95 | < 0.001 |
| Socioeconomic status | 0.91 | 0.88, 0.93 | < 0.001 | 0.97 | 0.95, 0.99 | 0.010 | 0.94 | 0.92, 0.96 | < 0.001 | |
| Minority-language status | 0.93 | 0.91, 0.96 | < 0.001 | 0.94 | 0.92, 0.96 | < 0.001 | 0.94 | 0.92, 0.96 | < 0.001 | |
| Household composition | 0.96 | 0.93, 0.98 | 0.001 | 1.00 | 0.98, 1.03 | 0.776 | 0.98 | 0.96, 1.01 | 0.159 | |
| Housing-transportation | 0.94 | 0.91, 0.96 | < 0.001 | 0.97 | 0.95, 0.99 | 0.006 | 0.94 | 0.92, 0.96 | < 0.001 | |
| Gallbladder | Total | 1.05 | 1.01, 1.10 | 0.024 | 0.99 | 0.93, 1.06 | 0.843 | 0.91 | 0.87, 0.95 | < 0.001 |
| Socioeconomic status | 1.06 | 1.02, 1.11 | 0.006 | 1.00 | 0.94, 1.07 | 0.917 | 0.92 | 0.88, 0.96 | < 0.001 | |
| Minority-language status | 0.99 | 0.95, 1.03 | 0.576 | 0.95 | 0.89, 1.01 | 0.101 | 0.94 | 0.90, 0.98 | 0.003 | |
| Household composition | 1.02 | 0.98, 1.06 | 0.422 | 1.04 | 0.98, 1.11 | 0.227 | 0.98 | 0.94, 1.02 | 0.295 | |
| Housing-transportation | 1.02 | 0.98, 1.07 | 0.272 | 0.98 | 0.92, 1.05 | 0.598 | 0.92 | 0.88, 0.96 | < 0.001 | |
| Gastroesophageal junction | Total | 0.97 | 0.94, 1.01 | 0.106 | 0.93 | 0.90, 0.96 | < 0.001 | 0.94 | 0.91, 0.98 | < 0.001 |
| Socioeconomic status | 0.98 | 0.95, 1.01 | 0.223 | 0.98 | 0.95, 1.01 | 0.123 | 0.94 | 0.91, 0.97 | < 0.001 | |
| Minority-language status | 0.98 | 0.94, 1.01 | 0.139 | 0.88 | 0.85, 0.90 | < 0.001 | 0.96 | 0.93, 0.99 | 0.015 | |
| Household composition | 1.01 | 0.98, 1.04 | 0.539 | 1.07 | 1.04, 1.11 | < 0.001 | 0.97 | 0.94, 1.01 | 0.099 | |
| Housing-transportation | 0.98 | 0.95, 1.01 | 0.277 | 0.94 | 0.91, 0.97 | < 0.001 | 0.96 | 0.93, 0.99 | 0.007 | |
| Liver | Total | 0.91 | 0.89, 0.93 | < 0.001 | 0.87 | 0.85, 0.89 | < 0.001 | 1.00 | 0.98, 1.02 | 0.960 |
| Socioeconomic status | 0.89 | 0.87, 0.90 | < 0.001 | 0.92 | 0.89, 0.94 | < 0.001 | 1.00 | 0.98, 1.01 | 0.776 | |
| Minority-language status | 1.00 | 0.98, 1.02 | 0.868 | 0.83 | 0.81, 0.86 | < 0.001 | 1.02 | 1.00, 1.04 | 0.029 | |
| Household composition | 0.89 | 0.87, 0.91 | < 0.001 | 1.04 | 1.01, 1.07 | 0.003 | 1.00 | 0.99, 1.02 | 0.588 | |
| Housing-transportation | 0.95 | 0.94, 0.97 | < 0.001 | 0.85 | 0.83, 0.88 | < 0.001 | 0.98 | 0.97, 1.00 | 0.053 | |
| Pancreatic head | Total | 0.96 | 0.94, 0.98 | < 0.001 | 0.95 | 0.92, 0.97 | < 0.001 | 0.91 | 0.90, 0.93 | < 0.001 |
| Socioeconomic status | 0.94 | 0.92, 0.96 | < 0.001 | 1.00 | 0.97, 1.02 | 0.879 | 0.93 | 0.92, 0.95 | < 0.001 | |
| Minority-language status | 1.02 | 1.00, 1.04 | 0.099 | 0.88 | 0.86, 0.90 | < 0.001 | 0.94 | 0.92, 0.95 | < 0.001 | |
| Household composition | 0.95 | 0.93, 0.97 | < 0.001 | 1.08 | 1.05, 1.10 | < 0.001 | 0.98 | 0.97, 1.00 | 0.078 | |
| Housing-transportation | 0.99 | 0.97, 1.01 | 0.231 | 0.91 | 0.88, 0.93 | < 0.001 | 0.91 | 0.89, 0.93 | < 0.001 | |
| Pancreatic body and tail | Total | 0.96 | 0.93, 0.99 | 0.008 | 0.95 | 0.91, 0.99 | 0.013 | 0.90 | 0.88, 0.93 | < 0.001 |
| Socioeconomic status | 0.95 | 0.92, 0.97 | < 0.001 | 0.98 | 0.94, 1.03 | 0.452 | 0.93 | 0.91, 0.95 | < 0.001 | |
| Minority-language status | 1.05 | 1.02, 1.08 | 0.001 | 0.90 | 0.86, 0.94 | < 0.001 | 0.94 | 0.92, 0.96 | < 0.001 | |
| Household composition | 0.93 | 0.91, 0.96 | < 0.001 | 1.04 | 0.99, 1.08 | 0.108 | 0.96 | 0.94, 0.98 | 0.001 | |
| Housing-transportation | 0.98 | 0.95, 1.01 | 0.169 | 0.92 | 0.88, 0.96 | < 0.001 | 0.91 | 0.89, 0.94 | < 0.001 | |
| Pancreatic, other | Total | 0.95 | 0.91, 0.99 | 0.016 | 0.93 | 0.88, 0.98 | 0.004 | 0.91 | 0.88, 0.93 | < 0.001 |
| Socioeconomic status | 0.92 | 0.89, 0.97 | < 0.001 | 0.95 | 0.91, 1.00 | 0.066 | 0.92 | 0.89, 0.94 | < 0.001 | |
| Minority-language status | 1.03 | 0.99, 1.08 | 0.179 | 0.92 | 0.87, 0.96 | 0.001 | 0.97 | 0.95, 1.00 | 0.039 | |
| Household composition | 0.93 | 0.89, 0.97 | 0.001 | 1.00 | 0.95, 1.05 | 0.969 | 0.94 | 0.91, 0.96 | < 0.001 | |
| Housing-transportation | 0.97 | 0.93, 1.01 | 0.134 | 0.90 | 0.85, 0.94 | < 0.001 | 0.93 | 0.91, 0.95 | < 0.001 | |
| Rectum | Total | 0.95 | 0.94, 0.97 | < 0.001 | 1.00 | 0.98, 1.01 | 0.564 | 0.97 | 0.96, 0.99 | < 0.001 |
| Socioeconomic status | 0.96 | 0.95, 0.98 | < 0.001 | 1.01 | 1.00, 1.03 | 0.106 | 0.99 | 0.97, 1.00 | 0.043 | |
| Minority-language status | 0.94 | 0.93, 0.96 | < 0.001 | 0.95 | 0.93, 0.96 | < 0.001 | 0.95 | 0.93, 0.96 | < 0.001 | |
| Household composition | 1.00 | 0.99, 1.02 | 0.769 | 1.05 | 1.04, 1.07 | < 0.001 | 1.02 | 1.01, 1.04 | 0.001 | |
| Housing-transportation | 0.96 | 0.95, 0.98 | < 0.001 | 1.00 | 0.98, 1.01 | 0.539 | 0.98 | 0.96, 0.99 | 0.002 | |
| Small intestine | Total | 0.95 | 0.91, 1.00 | 0.066 | 1.07 | 0.97, 1.18 | 0.205 | 0.91 | 0.87, 0.96 | 0.001 |
| Socioeconomic status | 0.96 | 0.91, 1.01 | 0.099 | 1.00 | 0.90, 1.10 | 0.924 | 0.95 | 0.90, 1.0 | 0.030 | |
| Minority-language status | 0.95 | 0.90, 1.00 | 0.032 | 1.04 | 0.95, 1.15 | 0.380 | 0.96 | 0.91, 1.01 | 0.136 | |
| Household composition | 1.02 | 0.97, 1.07 | 0.486 | 1.02 | 0.93, 1.13 | 0.675 | 0.96 | 0.92, 1.02 | 0.166 | |
| Housing-transportation | 0.94 | 0.90, 0.99 | 0.022 | 1.07 | 0.97, 1.18 | 0.183 | 0.90 | 0.86, 0.95 | < 0.001 | |
| Stomach | Total | 0.99 | 0.97, 1.02 | 0.567 | 0.94 | 0.91, 0.97 | < 0.001 | 0.94 | 0.91, 0.96 | < 0.001 |
| Socioeconomic status | 0.97 | 0.95, 0.99 | 0.006 | 0.96 | 0.93, 0.99 | 0.007 | 0.93 | 0.91, 0.96 | < 0.001 | |
| Minority-language status | 1.04 | 1.01, 1.06 | 0.003 | 0.91 | 0.88, 0.94 | < 0.001 | 0.98 | 0.96, 1.00 | 0.049 | |
| Household composition | 0.95 | 0.93, 0.98 | < 0.001 | 1.02 | 0.99, 1.05 | 0.196 | 0.95 | 0.93, 0.97 | < 0.001 | |
| Housing-transportation | 1.01 | 0.99, 1.04 | 0.322 | 0.96 | 0.93, 0.99 | 0.007 | 0.97 | 0.94, 0.99 | 0.004 | |
| Gastrointestinal, other | Total | 1.05 | 0.93, 1.19 | 0.404 | 0.85 | 0.76, 0.93 | 0.001 | 0.89 | 0.84, 0.94 | < 0.001 |
| Socioeconomic status | 1.06 | 0.94, 1.20 | 0.341 | 0.87 | 0.79, 0.96 | 0.006 | 0.93 | 0.87, 0.98 | 0.006 | |
| Minority-language status | 1.07 | 0.95, 1.21 | 0.252 | 0.89 | 0.80, 0.98 | 0.017 | 0.91 | 0.86, 0.96 | 0.001 | |
| Household composition | 1.00 | 0.89, 1.13 | 0.965 | 0.97 | 0.88, 1.07 | 0.497 | 1.01 | 0.96, 1.07 | 0.603 | |
| Housing-transportation | 0.93 | 0.82, 1.05 | 0.250 | 0.91 | 0.82, 1.00 | 0.062 | 0.86 | 0.81, 0.91 | < 0.001 | |
- a By American Joint Committee on Cancer, 6th Edition (AJCC-6); Univariate logistic regressions with calculated Odds Ratios (OR) and 95% confidence intervals (95% CI) were performed with lowest relative SVI quintiles set as the reference within each histopathology type.
Patients residing in counties with higher total SVI scores also had decreased odds of receiving chemotherapy (lowest, pancreas-OR, 0.90; 95% CI, 0.88–0.93) (see Data S1 for all significant sites) (Figure 1, Table 2). Similarly, patients with higher total SVI also had decreased odds of receiving radiation therapy (lowest, hepatic-OR, 0.87; 95% CI, 0.85–0.89) (see Data S1 for all significant sites) (Figure 1, Table 2). Of note, the subthemes that had the biggest impact on decreased likelihood to receive chemotherapy included increasing vulnerability in housing-transportation, followed by minority-language status and socioeconomic status, as well as household composition proportionally. In contrast, the vulnerability subthemes with the biggest impact on radiation therapy receipt included vulnerability in minority-language status and socioeconomic status, with household composition and housing-transportation proportionally contributing the same impact (Table 2).
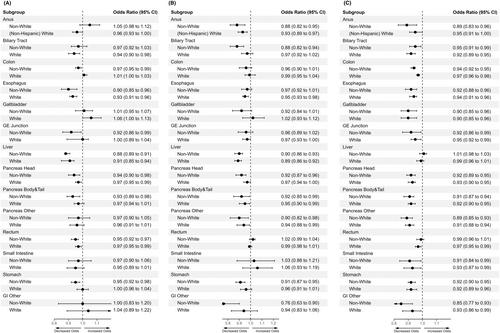
When differentiating the influence of increasing county-level social vulnerabilities between White and Non-White GIC patient cohorts, both cohorts displayed decreased odds of receiving indicated surgical resection and radiation therapy across several GICs. However, Non-White patients displayed higher-magnitude decreases compared to White patients across different GIC types for each modality (Figure 2, Table 3).
| Primary classificationa | Characteristic | Surgical resection | Radiation therapy | Chemotherapy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||
| Anus—Non-White | Total | 1.05 | 0.98, 1.12 | 0.200 | 0.88 | 0.82, 0.95 | 0.001 | 0.89 | 0.83, 0.96 | 0.002 |
| Socioeconomic status | 1.06 | 0.99, 1.14 | 0.077 | 0.91 | 0.85, 0.98 | 0.017 | 0.89 | 0.83, 0.96 | 0.002 | |
| Minority-language status | 0.98 | 0.91, 1.05 | 0.525 | 0.91 | 0.85, 0.98 | 0.017 | 0.93 | 0.87, 1.00 | 0.054 | |
| Household composition | 1.04 | 0.97, 1.12 | 0.224 | 1.00 | 0.93, 1.08 | 0.997 | 0.97 | 0.90, 1.04 | 0.412 | |
| Housing-transportation | 1.00 | 0.93, 1.07 | 0.912 | 0.93 | 0.86, 1.00 | 0.051 | 0.97 | 0.90, 1.04 | 0.389 | |
| Anus—White | Total | 0.96 | 0.93, 1.00 | 0.056 | 0.93 | 0.89, 0.97 | 0.001 | 0.95 | 0.91, 1.00 | 0.033 |
| Socioeconomic status | 0.97 | 0.94, 1.01 | 0.166 | 0.94 | 0.90, 0.99 | 0.010 | 0.96 | 0.92, 1.00 | 0.056 | |
| Minority-language status | 0.98 | 0.94, 1.01 | 0.214 | 0.91 | 0.87, 0.95 | < 0.001 | 0.95 | 0.91, 0.99 | 0.023 | |
| Household composition | 0.99 | 0.95, 1.03 | 0.621 | 1.03 | 0.99, 1.08 | 0.173 | 1.00 | 0.96, 1.05 | 0.844 | |
| Housing-transportation | 0.96 | 0.93, 1.00 | 0.064 | 0.92 | 0.88, 0.96 | < 0.001 | 0.95 | 0.91, 0.99 | 0.013 | |
| Biliary tract—Non-White | Total | 0.97 | 0.92, 1.03 | 0.292 | 0.88 | 0.82, 0.94 | < 0.001 | 0.95 | 0.91, 0.99 | 0.026 |
| Socioeconomic status | 0.95 | 0.90, 1.01 | 0.100 | 0.91 | 0.84, 0.97 | 0.008 | 0.98 | 0.93, 1.02 | 0.298 | |
| Minority-language status | 1.05 | 1.00, 1.11 | 0.069 | 0.92 | 0.85, 0.99 | 0.020 | 0.95 | 0.91, 1.00 | 0.037 | |
| Household composition | 0.91 | 0.86, 0.96 | < 0.001 | 0.99 | 0.92, 1.06 | 0.760 | 1.03 | 0.98, 1.07 | 0.264 | |
| Housing-transportation | 1.00 | 0.94, 1.05 | 0.915 | 0.86 | 0.80, 0.93 | < 0.001 | 0.92 | 0.88, 0.97 | 0.001 | |
| Biliary tract—White | Total | 0.94 | 0.90, 0.98 | 0.007 | 0.97 | 0.92, 1.02 | 0.196 | 0.92 | 0.89, 0.95 | < 0.001 |
| Socioeconomic status | 0.95 | 0.91, 0.99 | 0.011 | 1.01 | 0.96, 1.06 | 0.781 | 0.93 | 0.89, 0.96 | < 0.001 | |
| Minority-language status | 1.05 | 1.00, 1.09 | 0.030 | 0.96 | 0.91, 1.01 | 0.098 | 0.95 | 0.92, 0.98 | 0.004 | |
| Household composition | 0.92 | 0.88, 0.96 | < 0.001 | 1.04 | 0.99, 1.09 | 0.099 | 0.96 | 0.93, 0.99 | 0.018 | |
| Housing-transportation | 0.95 | 0.91, 0.99 | 0.011 | 0.93 | 0.89, 0.98 | 0.006 | 0.94 | 0.91, 0.97 | < 0.001 | |
| Colon—Non-White | Total | 0.97 | 0.95, 0.99 | 0.005 | 0.96 | 0.90, 1.01 | 0.133 | 0.94 | 0.92, 0.95 | < 0.001 |
| Socioeconomic status | 0.97 | 0.95, 0.99 | 0.003 | 0.97 | 0.92, 1.03 | 0.382 | 0.95 | 0.94, 0.97 | < 0.001 | |
| Minority-language status | 1.00 | 0.98, 1.02 | 0.869 | 0.92 | 0.86, 0.97 | 0.004 | 0.91 | 0.90, 0.93 | < 0.001 | |
| Household composition | 0.99 | 0.97, 1.01 | 0.171 | 1.03 | 0.97, 1.09 | 0.330 | 1.00 | 0.98, 1.02 | 0.971 | |
| Housing-transportation | 1.00 | 0.98, 1.02 | 0.806 | 0.96 | 0.91, 1.02 | 0.213 | 0.93 | 0.92, 0.95 | < 0.001 | |
| Colon—White | Total | 1.01 | 1.00, 1.03 | 0.158 | 0.99 | 0.95, 1.04 | 0.782 | 0.97 | 0.96, 0.98 | < 0.001 |
| Socioeconomic status | 1.02 | 1.00, 1.03 | 0.039 | 1.02 | 0.98, 1.07 | 0.295 | 0.98 | 0.97, 0.99 | 0.002 | |
| Minority-language status | 0.97 | 0.96, 0.99 | < 0.001 | 0.89 | 0.86, 0.93 | < 0.001 | 0.95 | 0.94, 0.96 | < 0.001 | |
| Household composition | 1.04 | 1.02, 1.05 | < 0.001 | 1.10 | 1.05, 1.14 | < 0.001 | 1.01 | 1.0, 1.02 | 0.267 | |
| Housing-transportation | 1.00 | 0.99, 1.02 | 0.656 | 0.98 | 0.94, 1.02 | 0.394 | 0.96 | 0.95, 0.98 | < 0.001 | |
| Esophagus—Non-White | Total | 0.90 | 0.85, 0.96 | 0.002 | 0.97 | 0.92, 1.01 | 0.151 | 0.92 | 0.88, 0.96 | < 0.001 |
| Socioeconomic status | 0.89 | 0.83, 0.95 | < 0.001 | 0.97 | 0.93, 1.02 | 0.209 | 0.93 | 0.89, 0.98 | 0.003 | |
| Minority-language status | 1.07 | 1.00, 1.14 | 0.043 | 0.89 | 0.85, 0.93 | < 0.001 | 0.93 | 0.89, 0.97 | 0.001 | |
| Household composition | 0.87 | 0.82, 0.93 | < 0.001 | 1.04 | 0.99, 1.08 | 0.131 | 0.99 | 0.95, 1.04 | 0.765 | |
| Housing-transportation | 1.00 | 0.94, 1.07 | 0.999 | 0.96 | 0.92, 1.00 | 0.080 | 0.93 | 0.89, 0.98 | 0.003 | |
| Esophagus—White | Total | 0.93 | 0.91, 0.96 | < 0.001 | 0.95 | 0.93, 0.98 | < 0.001 | 0.94 | 0.91, 0.96 | < 0.001 |
| Socioeconomic status | 0.93 | 0.90, 0.96 | < 0.001 | 0.96 | 0.94, 0.99 | 0.004 | 0.95 | 0.92, 0.97 | < 0.001 | |
| Minority-language status | 0.95 | 0.92, 0.98 | 0.001 | 0.95 | 0.92, 0.97 | < 0.001 | 0.95 | 0.93, 0.98 | < 0.001 | |
| Household composition | 0.97 | 0.94, 1.00 | 0.047 | 0.99 | 0.97, 1.02 | 0.598 | 0.98 | 0.95, 1.00 | 0.087 | |
| Housing-transportation | 0.96 | 0.93, 0.99 | 0.003 | 0.97 | 0.95, 1.00 | 0.046 | 0.95 | 0.93, 0.98 | < 0.001 | |
| Gallbladder—Non-White | Total | 1.01 | 0.95, 1.07 | 0.799 | 0.92 | 0.84, 1.01 | 0.089 | 0.90 | 0.85, 0.96 | 0.001 |
| Socioeconomic status | 1.00 | 0.94, 1.07 | 0.898 | 0.97 | 0.89, 1.06 | 0.490 | 0.91 | 0.86, 0.97 | 0.003 | |
| Minority-language status | 1.00 | 0.94, 1.06 | 0.958 | 0.88 | 0.80, 0.96 | 0.004 | 0.89 | 0.84, 0.95 | < 0.001 | |
| Household composition | 0.98 | 0.92, 1.04 | 0.546 | 1.09 | 0.99, 1.19 | 0.066 | 0.99 | 0.93, 1.05 | 0.769 | |
| Housing-transportation | 1.02 | 0.96, 1.09 | 0.456 | 0.93 | 0.85, 1.02 | 0.114 | 0.89 | 0.84, 0.95 | < 0.001 | |
| Gallbladder—White | Total | 1.06 | 1.00, 1.13 | 0.039 | 1.02 | 0.93, 1.12 | 0.653 | 0.90 | 0.85, 0.96 | 0.001 |
| Socioeconomic status | 1.11 | 1.04, 1.17 | 0.001 | 1.03 | 0.94, 1.12 | 0.581 | 0.92 | 0.87, 0.98 | 0.006 | |
| Minority-language status | 0.96 | 0.90, 1.02 | 0.157 | 0.98 | 0.89, 1.07 | 0.619 | 0.95 | 0.89, 1.00 | 0.067 | |
| Household composition | 1.05 | 0.99, 1.12 | 0.079 | 1.03 | 0.94, 1.12 | 0.576 | 0.97 | 0.91, 1.02 | 0.253 | |
| Housing-transportation | 1.03 | 0.97, 1.09 | 0.411 | 1.01 | 0.93, 1.11 | 0.756 | 0.91 | 0.86, 0.97 | 0.003 | |
| Gastroesophageal junction—Non-White | Total | 0.92 | 0.86, 0.99 | 0.025 | 0.96 | 0.89, 1.02 | 0.201 | 0.92 | 0.86, 0.99 | 0.016 |
| Socioeconomic status | 0.91 | 0.85, 0.97 | 0.007 | 0.96 | 0.89, 1.02 | 0.209 | 0.90 | 0.84, 0.96 | 0.002 | |
| Minority-language status | 1.03 | 0.96, 1.10 | 0.469 | 0.90 | 0.84, 0.96 | 0.002 | 0.97 | 0.91, 1.04 | 0.372 | |
| Household composition | 0.94 | 0.87, 1.01 | 0.071 | 1.02 | 0.96, 1.09 | 0.512 | 0.91 | 0.85, 0.97 | 0.004 | |
| Housing-transportation | 0.97 | 0.90, 1.04 | 0.357 | 0.92 | 0.86, 0.99 | 0.018 | 0.98 | 0.92, 1.05 | 0.553 | |
| Gastroesophageal junction—White | Total | 1.00 | 0.97, 1.04 | 0.859 | 0.97 | 0.93, 1.00 | 0.073 | 0.95 | 0.92, 0.99 | 0.013 |
| Socioeconomic status | 1.00 | 0.97, 1.04 | 0.806 | 1.00 | 0.97, 1.04 | 0.999 | 0.97 | 0.93, 1.00 | 0.067 | |
| Minority-language status | 0.98 | 0.94, 1.02 | 0.256 | 0.89 | 0.86, 0.93 | < 0.001 | 0.95 | 0.92, 0.99 | 0.007 | |
| Household composition | 1.02 | 0.98, 1.06 | 0.353 | 1.06 | 1.02, 1.10 | 0.001 | 0.99 | 0.95, 1.02 | 0.487 | |
| Housing-transportation | 1.01 | 0.97, 1.05 | 0.634 | 0.98 | 0.95, 1.02 | 0.273 | 0.97 | 0.94, 1.01 | 0.113 | |
| Liver—Non-White | Total | 0.88 | 0.86, 0.91 | < 0.001 | 0.90 | 0.86, 0.93 | < 0.001 | 1.01 | 0.98, 1.03 | 0.575 |
| Socioeconomic status | 0.87 | 0.85, 0.90 | < 0.001 | 0.94 | 0.90, 0.98 | 0.002 | 1.00 | 0.98, 1.03 | 0.735 | |
| Minority-language status | 1.02 | 1.00, 1.05 | 0.103 | 0.82 | 0.79, 0.86 | < 0.001 | 1.02 | 0.99, 1.04 | 0.182 | |
| Household composition | 0.86 | 0.83, 0.88 | < 0.001 | 1.04 | 1.00, 1.08 | 0.061 | 1.02 | 1.00, 1.04 | 0.107 | |
| Housing-transportation | 1.01 | 0.98, 1.04 | 0.474 | 0.86 | 0.82, 0.89 | < 0.001 | 0.99 | 0.96, 1.01 | 0.302 | |
| Liver—White | Total | 0.91 | 0.89, 0.94 | < 0.001 | 0.89 | 0.86, 0.92 | < 0.001 | 0.99 | 0.96, 1.01 | 0.244 |
| Socioeconomic status | 0.91 | 0.88, 0.93 | < 0.001 | 0.92 | 0.89, 0.96 | < 0.001 | 1.0 | 0.97, 1.02 | 0.645 | |
| Minority-language status | 1.01 | 0.98, 1.04 | 0.597 | 0.90 | 0.87, 0.93 | < 0.001 | 1.02 | 1.00, 1.04 | 0.086 | |
| Household composition | 0.91 | 0.89, 0.94 | < 0.001 | 1.01 | 0.97, 1.04 | 0.732 | 1.00 | 0.97, 1.02 | 0.805 | |
| Housing-transportation | 0.93 | 0.91, 0.96 | < 0.001 | 0.88 | 0.85, 0.91 | < 0.001 | 0.97 | 0.95, 1.00 | 0.021 | |
| Pancreatic head—Non-White | Total | 0.94 | 0.90, 0.98 | 0.002 | 0.92 | 0.87, 0.96 | < 0.001 | 0.92 | 0.89, 0.95 | < 0.001 |
| Socioeconomic status | 0.92 | 0.89, 0.96 | < 0.001 | 0.95 | 0.91, 1.00 | 0.055 | 0.93 | 0.90, 0.96 | < 0.001 | |
| Minority-language status | 1.03 | 0.99, 1.07 | 0.114 | 0.87 | 0.83, 0.91 | < 0.001 | 0.92 | 0.89, 0.95 | < 0.001 | |
| Household composition | 0.92 | 0.88, 0.96 | < 0.001 | 1.05 | 1.00, 1.10 | 0.059 | 0.99 | 0.96, 1.02 | 0.563 | |
| Housing-transportation | 1.02 | 0.98, 1.06 | 0.308 | 0.88 | 0.84, 0.93 | < 0.001 | 0.92 | 0.89, 0.96 | < 0.001 | |
| Pancreatic head—White | Total | 0.97 | 0.95, 0.99 | 0.044 | 0.97 | 0.94, 1.00 | 0.072 | 0.93 | 0.90, 0.95 | < 0.001 |
| Socioeconomic status | 0.95 | 0.93, 0.98 | < 0.001 | 1.02 | 0.99, 1.05 | 0.196 | 0.94 | 0.92, 0.96 | < 0.001 | |
| Minority-language status | 1.02 | 1.00, 1.05 | 0.114 | 0.90 | 0.88, 0.93 | < 0.001 | 0.96 | 0.94, 0.98 | < 0.001 | |
| Household composition | 0.96 | 0.94, 0.99 | 0.005 | 1.07 | 1.04, 1.10 | < 0.001 | 0.96 | 0.94, 0.98 | 0.001 | |
| Housing-transportation | 0.99 | 0.97, 1.02 | 0.534 | 0.93 | 0.90, 0.95 | < 0.001 | 0.92 | 0.90, 0.94 | < 0.001 | |
| Pancreatic body and tail—Non-White | Total | 0.93 | 0.89, 0.98 | 0.007 | 0.92 | 0.85, 0.99 | 0.041 | 0.91 | 0.87, 0.94 | < 0.001 |
| Socioeconomic status | 0.89 | 0.85, 0.94 | < 0.001 | 0.96 | 0.89, 1.04 | 0.329 | 0.92 | 0.88, 0.96 | < 0.001 | |
| Minority-language status | 1.05 | 1.00, 1.11 | 0.057 | 0.88 | 0.81, 0.95 | 0.001 | 0.94 | 0.90, 0.98 | 0.007 | |
| Household composition | 0.89 | 0.85, 0.94 | < 0.001 | 1.00 | 0.93, 1.08 | 0.938 | 0.95 | 0.91, 0.99 | 0.021 | |
| Housing-transportation | 1.00 | 0.95, 1.06 | 0.919 | 0.90 | 0.83, 0.97 | 0.006 | 0.92 | 0.88, 0.96 | < 0.001 | |
| Pancreatic body and tail—White | Total | 0.97 | 0.94, 1.01 | 0.097 | 0.95 | 0.90, 0.99 | 0.037 | 0.92 | 0.90, 0.95 | < 0.001 |
| Socioeconomic status | 0.96 | 0.93, 1.00 | 0.040 | 0.99 | 0.94, 1.04 | 0.736 | 0.94 | 0.91, 0.96 | < 0.001 | |
| Minority-language status | 1.04 | 1.00, 1.07 | 0.050 | 0.90 | 0.85, 0.95 | < 0.001 | 0.96 | 0.93, 0.99 | 0.006 | |
| Household composition | 0.96 | 0.92, 0.99 | 0.011 | 1.05 | 1.00, 1.10 | 0.068 | 0.95 | 0.93, 0.98 | 0.001 | |
| Housing-transportation | 0.97 | 0.94, 1.01 | 0.093 | 0.92 | 0.88, 0.97 | 0.002 | 0.93 | 0.90, 0.96 | < 0.001 | |
| Pancreatic, other—Non-White | Total | 0.97 | 0.90, 1.05 | 0.419 | 0.90 | 0.82, 0.98 | 0.016 | 0.89 | 0.85, 0.93 | < 0.001 |
| Socioeconomic status | 0.93 | 0.86, 1.00 | 0.054 | 0.95 | 0.87, 1.04 | 0.231 | 0.92 | 0.87, 0.96 | < 0.001 | |
| Minority-language status | 1.06 | 0.99, 1.15 | 0.115 | 0.86 | 0.79, 0.94 | 0.001 | 0.94 | 0.90, 0.99 | 0.016 | |
| Household composition | 0.89 | 0.83, 0.96 | 0.003 | 1.03 | 0.94, 1.13 | 0.494 | 0.95 | 0.90, 0.99 | 0.018 | |
| Housing-transportation | 1.02 | 0.95, 1.10 | 0.576 | 0.85 | 0.78, 0.93 | 0.001 | 0.92 | 0.87, 0.96 | < 0.001 | |
| Pancreatic, other—White | Total | 0.96 | 0.91, 1.01 | 0.097 | 0.94 | 0.88, 0.99 | 0.034 | 0.91 | 0.88, 0.94 | < 0.001 |
| Socioeconomic status | 0.95 | 0.90, 1.00 | 0.074 | 0.95 | 0.90, 1.01 | 0.123 | 0.92 | 0.89, 0.95 | < 0.001 | |
| Minority-language status | 1.00 | 0.95, 1.05 | 0.975 | 0.93 | 0.87, 0.99 | 0.018 | 0.97 | 0.93, 1.00 | 0.030 | |
| Household composition | 0.95 | 0.90, 1.00 | 0.044 | 0.98 | 0.92, 1.04 | 0.520 | 0.93 | 0.90, 0.96 | < 0.001 | |
| Housing-transportation | 0.97 | 0.92, 1.02 | 0.218 | 0.92 | 0.87, 0.98 | 0.009 | 0.95 | 0.92, 0.98 | 0.001 | |
| Rectum—Non-White | Total | 0.95 | 0.92, 0.97 | < 0.001 | 1.02 | 0.99, 1.04 | 0.222 | 0.99 | 0.96, 1.01 | 0.268 |
| Socioeconomic status | 0.93 | 0.91, 0.96 | < 0.001 | 1.03 | 1.00, 1.05 | 0.029 | 1.00 | 0.98, 1.03 | 0.709 | |
| Minority-language status | 1.00 | 0.97, 1.03 | 0.925 | 0.97 | 0.94, 0.99 | 0.007 | 0.94 | 0.92, 0.97 | < 0.001 | |
| Household composition | 0.95 | 0.93, 0.98 | 0.001 | 1.05 | 1.02, 1.07 | < 0.001 | 1.02 | 1.00, 1.05 | 0.057 | |
| Housing-transportation | 0.99 | 0.96, 1.01 | 0.314 | 0.99 | 0.97, 1.01 | 0.421 | 0.97 | 0.95, 1.0 | 0.017 | |
| Rectum—White | Total | 0.97 | 0.95, 0.99 | 0.002 | 0.99 | 0.98, 1.01 | 0.519 | 0.97 | 0.95, 0.99 | < 0.001 |
| Socioeconomic status | 0.99 | 0.97, 1.01 | 0.526 | 1.00 | 0.99, 1.02 | 0.809 | 0.97 | 0.96, 0.99 | 0.004 | |
| Minority-language status | 0.93 | 0.91, 0.95 | < 0.001 | 0.94 | 0.92, 0.95 | < 0.001 | 0.94 | 0.93, 0.96 | < 0.001 | |
| Household composition | 1.02 | 1.00, 1.04 | 0.054 | 1.04 | 1.03, 1.06 | < 0.001 | 1.02 | 1.00, 1.04 | 0.041 | |
| Housing-transportation | 0.97 | 0.95, 0.98 | < 0.001 | 1.00 | 0.98, 1.01 | 0.692 | 0.98 | 0.96, 1.0 | 0.010 | |
| Small intestine—Non-White | Total | 0.97 | 0.90, 1.06 | 0.537 | 1.03 | 0.88, 1.21 | 0.710 | 0.91 | 0.84, 0.99 | 0.030 |
| Socioeconomic status | 0.96 | 0.89, 1.05 | 0.380 | 1.04 | 0.88, 1.22 | 0.654 | 0.95 | 0.87, 1.03 | 0.194 | |
| Minority-language status | 0.95 | 0.87, 1.03 | 0.224 | 0.96 | 0.81, 1.13 | 0.600 | 0.89 | 0.82, 0.97 | 0.009 | |
| Household composition | 1.00 | 0.92, 1.09 | 0.974 | 1.03 | 0.87, 1.21 | 0.745 | 1.02 | 0.94, 1.11 | 0.592 | |
| Housing-transportation | 0.96 | 0.88, 1.04 | 0.296 | 0.97 | 0.83, 1.15 | 0.758 | 0.85 | 0.78, 0.92 | < 0.001 | |
| Small intestine—White | Total | 0.95 | 0.89, 1.01 | 0.116 | 1.06 | 0.93, 1.19 | 0.388 | 0.93 | 0.87, 0.99 | 0.031 |
| Socioeconomic status | 0.97 | 0.91, 1.03 | 0.343 | 0.97 | 0.86, 1.10 | 0.663 | 0.93 | 0.87, 0.99 | 0.033 | |
| Minority-language status | 0.96 | 0.90, 1.02 | 0.167 | 1.10 | 0.97, 1.24 | 0.129 | 0.97 | 0.91, 1.04 | 0.413 | |
| Household composition | 1.02 | 0.95, 1.08 | 0.599 | 1.00 | 0.89, 1.13 | 0.961 | 0.93 | 0.87, 0.99 | 0.028 | |
| Housing-transportation | 0.95 | 0.89, 1.01 | 0.088 | 1.12 | 0.99, 1.26 | 0.078 | 0.93 | 0.87, 0.99 | 0.018 | |
| Stomach—Non-White | Total | 0.95 | 0.92, 0.98 | 0.001 | 0.91 | 0.87, 0.95 | < 0.001 | 0.92 | 0.90, 0.95 | < 0.001 |
| Socioeconomic status | 0.94 | 0.91, 0.97 | < 0.001 | 0.93 | 0.89, 0.96 | < 0.001 | 0.94 | 0.91, 0.96 | < 0.001 | |
| Minority-language status | 1.02 | 0.99, 1.05 | 0.125 | 0.89 | 0.85, 0.92 | < 0.001 | 0.94 | 0.92, 0.97 | < 0.001 | |
| Household composition | 0.94 | 0.91, 0.97 | < 0.001 | 1.00 | 0.97, 1.05 | 0.814 | 0.97 | 0.94, 1.00 | 0.037 | |
| Housing-transportation | 1.00 | 0.97, 1.03 | 0.920 | 0.94 | 0.91, 0.98 | 0.005 | 0.95 | 0.92, 0.98 | < 0.001 | |
| Stomach—White | Total | 1.00 | 0.96, 1.04 | 0.903 | 0.96 | 0.91, 1.01 | 0.118 | 0.92 | 0.89, 0.96 | < 0.001 |
| Socioeconomic status | 1.00 | 0.97, 1.04 | 0.818 | 1.00 | 0.95, 1.06 | 0.877 | 0.92 | 0.89, 0.96 | < 0.001 | |
| Minority-language status | 1.00 | 0.97, 1.04 | 0.881 | 0.88 | 0.83, 0.93 | < 0.001 | 0.98 | 0.94, 1.02 | 0.256 | |
| Household composition | 0.98 | 0.94, 1.02 | 0.241 | 1.07 | 1.01, 1.13 | 0.017 | 0.95 | 0.92, 0.99 | 0.009 | |
| Housing-transportation | 1.02 | 0.98, 1.06 | 0.253 | 0.93 | 0.89, 0.99 | 0.013 | 0.95 | 0.91, 0.98 | 0.005 | |
| Gastrointestinal, other—Non-White | Total | 1.00 | 0.83, 1.20 | 0.966 | 0.76 | 0.63, 0.90 | 0.002 | 0.85 | 0.77, 0.93 | 0.001 |
| Socioeconomic status | 1.05 | 0.87, 1.27 | 0.583 | 0.77 | 0.65, 0.92 | 0.003 | 0.88 | 0.80, 0.97 | 0.009 | |
| Minority-language status | 0.99 | 0.82, 1.19 | 0.895 | 0.83 | 0.69, 0.98 | 0.030 | 0.90 | 0.82, 0.99 | 0.025 | |
| Household composition | 1.10 | 0.91, 1.33 | 0.314 | 0.86 | 0.73, 1.03 | 0.094 | 0.93 | 0.85, 1.02 | 0.144 | |
| Housing-transportation | 0.85 | 0.70, 1.02 | 0.082 | 0.85 | 0.71, 1.01 | 0.059 | 0.83 | 0.75, 0.91 | < 0.001 | |
| Gastrointestinal, other—White | Total | 1.04 | 0.89, 1.22 | 0.616 | 0.94 | 0.83, 1.06 | 0.285 | 0.93 | 0.86, 0.99 | 0.030 |
| Socioeconomic status | 1.07 | 0.92, 1.26 | 0.380 | 0.93 | 0.83, 1.05 | 0.255 | 0.95 | 0.88, 1.01 | 0.122 | |
| Minority-language status | 1.08 | 0.92, 1.28 | 0.322 | 0.93 | 0.82, 1.05 | 0.218 | 0.91 | 0.85, 0.97 | 0.007 | |
| Household composition | 0.98 | 0.83, 1.15 | 0.812 | 1.02 | 0.90, 1.15 | 0.768 | 1.05 | 0.98, 1.13 | 0.166 | |
| Housing-transportation | 1.01 | 0.86, 1.19 | 0.868 | 0.93 | 0.82, 1.05 | 0.222 | 0.89 | 0.83, 0.96 | 0.002 | |
- a By American Joint Committee on Cancer, 6th Edition (AJCC-6); Univariate logistic regressions with calculated Odds Ratios (OR) and 95% confidence intervals (95% CI) were performed with lowest relative SVI quintiles set as the reference within each histopathology type.
For surgical resection, Non-White patients were less likely to receive surgery than White patients with increasing overall social vulnerability for 8 out of 14 GIC sites (largest odds-ratio difference, gastroesophageal junction [Non-White, OR 0.92, 95% CI 0.86–0.99; White, OR 1.00, 95% CI 0.97–1.04]) (see Data S1 for all significant sites) (Figure 2A). Specific vulnerabilities in socioeconomic status and household composition contributed the most to these observed associations across both race-ethnicity cohorts (Table 3).
For radiation therapy, similar trends were observed for 7 out of 14 types (largest odds-ratio difference, gastrointestinal-other [Non-White, OR 0.76, 95% CI 0.63–0.90; White, 0.94, 95% CI 0.83–1.06]) (see Data S1 for all significant sites) (Figure 2B). Specific vulnerabilities in minority-language status, followed by socioeconomic status and housing-transportation in magnitude, contributed differentially to these observed trends across both cohorts (Table 3).
In contrast to surgery and radiation therapy, both Non-White and White cohorts displayed similar magnitudes of decreased chemotherapy receipt with increasing social vulnerability for a majority of GIC sites (see Data S1 for all significant sites) (Figure 2C). Specific vulnerabilities across all themes of socioeconomic status, minority-language status, household composition, and housing-transportation contributed differentially to these observed trends (Table 3).
3.2 Primary Site-Specific Trends in Survival Relative to SVI Percentile
Social vulnerability was strongly associated with survival differences among most patients with GIC (Figure S2). Survival among patients residing in the lowest versus highest SVI county had differences in survival that ranged from as high as a 21.3% decrease (6.85–5.40 months) among patients with biliary tract cancer to as low as a 1.3% decrease (8.48–8.37 months) among individuals with a gastroesophageal junction cancer (Figure 3). The impact of social vulnerability on survival varied across GIC diagnoses, having the most pronounced effect on patients with cancers of esophagus, stomach, liver, pancreas, and biliary tract (all p < 0.001) (Figure S5). Of note, social vulnerability subthemes that contributed the most to differences in survival were socioeconomic status and household composition, followed by housing-transportation, and then minority-language status (Figure 3).
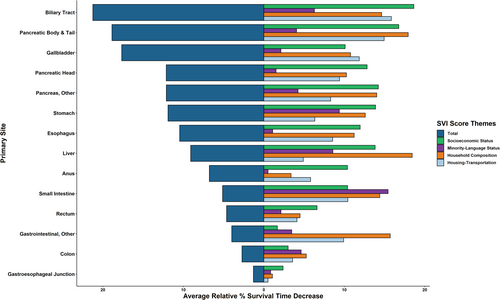
When differentiating the influence of increasing social vulnerability with survival among White and Non-White patients diagnosed with GIC, both cohorts displayed associated decreases in survival (Figures S3 and S4). However, Non-White patients experienced higher decreases in survival period compared with White patients for 9/14 GIC types analyzed, with the maximum difference of 18.78% in biliary tract (Non-White, 34.29% decrease [7.91–5.20 months]; White, 15.50% decrease [6.66–5.63 months]) and minimum difference of 1.1% in gastroesophageal junction (Non-White, 2.07% decrease [8.51–8.33 months]; White, 0.98% decrease [8.47–8.39 months]). White patients experienced higher decreases in survival period versus non-White patients for 5/14 GIC types analyzed. The maximum difference was 17.7% for pancreas—other (White, 19.71% decrease [4.48–3.59 months]; Non-White, 1.99% decrease [4.31–4.22 months]), and the minimum difference was 4.45% for esophagus (White, 12.86% decrease [8.13–7.09 months]; Non-White, 8.41% decrease [7.31–6.69 months]) (Figure 4). For White patients with GIC, specific vulnerabilities in housing-transportation and household composition, followed by socioeconomic status, contributed the most to these observed overall vulnerability trends (Figure S6). For Non-White patients with GIC, minority-language status, housing transportation, and household composition contributed similarly to observed overall vulnerability trends (Figure S7).
4 Discussion
This nationally representative cohort of GIC patients serves to highlight how decreases in systemic and surgical therapy receipt and survival period were differentially associate with increasing overall social vulnerability and specific types of social vulnerability. Moreover, these differences were exacerbated relative to treatment receipt and survival period among Non-White patients with GIC versus White patients. The current study was important as the data provide information that identified which social vulnerability factors specifically impact non-surgical treatment disparities across a majority of GIC types, as well as demonstrated surgical treatment disparities among patients with understudied GIC types (e.g., non-hepatopancreatobiliary cancers). Furthermore, we demonstrated a wider variety of SDoH-factors to contextualize GIC disparities relative to long-term surveillance and survival/mortality that prior literature had not fully elucidated.
To our knowledge, this study principally demonstrated varied social vulnerability-related associations with GIC disparities relative to chemotherapy and radiotherapy receipt in a large, national scale dataset many GIC types. While racial disparities have been observed in adjuvant therapy receipt for certain GICs, data from this current study examined a broader cohort of GIC with consideration of other SDoH factors beyond race-ethnicity having a dramatic impact on outcomes [7, 12, 19]. Specifically, we confirmed how SDoH-vulnerabilities beyond race/ethnicity had greater impact. For instance, housing-transportation type & access, a notable SDoH-theme has been strongly linked to worse access to quality surgical care at high-volume surgical centers [20]. In the current study, housing-transportation had a larger magnitude-associations with decreased receipt of chemotherapy receipt than race-ethnicity and English-language proficiency. Furthermore, socioeconomic vulnerabilities had comparable association with worse outcomes as minoritized race-ethnicity across overall trends of poor chemotherapy receipt, which were consistent with previous work that noted an intersection of socioeconomic status and race/ethnicity [3, 11]. A similar trend was noted for receipt of radiation therapy for 7 out of 14 types with specific vulnerabilities related to minority-language status, followed by socioeconomic status and housing-transportation in magnitude. Collectively, SDoH-factors had a marked impact on the lack of utilization of non-operative management of several GIC at the national level [21-23]. In turn, the data emphasize how social factors beyond race-ethnicity impact receipt and utilization of non-operative cancer therapies for patients with GIC.
Notably, increased social vulnerability was associated with decreased utilization of surgical resection across 8/14 GIC types. Disparities in surgical utilization for GICs including esophageal, hepatic, pancreas, and biliary tract cancers were noted, and were directly impacted by differences related to socioeconomic status, race-ethnicity, and geography-transportation. Of note, many of the GIC types analyzed were characterized by the lowest-magnitude/highest-impact associations relative to HT- or SES-vulnerability, both of which were lower magnitude/higher impact than ML-vulnerabilities. Data on these themes and how each was differentially associated with variations in surgical treatment utilization across GICs further contextualized the relationship between socioeconomic-status and race-ethnicity [3, 11]. Prior investigations of the surgical resection trends among other oncologic pathologies have showcased similar trends of SES- and HT-vulnerabilities playing substantial roles in conferring this detrimental association, such as those of the head–neck, endocrine, skin, and central nervous systems [17, 18, 24-32]. Given calls to address systemic social biases that exacerbate racial differences in GIC treatment, data from the current study specifically highlights how SES and HT-based differences may represent important policy targets of policy to mitigate disparities in care across diverse sociodemographic/racial-ethnic groups [33].
The current study specifically highlights which subthemes of social vulnerability contributed the most to overall and individual racial/ethnic differences in the treatment of GIC. As overall social vulnerability increased, decreased utilization of surgical resection and radiation therapy receipt were more pronounced among Non-White GIC patients versus White GIC patients. Here, Non-White patients experienced worse disparities in surgery and radiation therapy than White patients that not only corroborated prior findings [6, 10, 34], but also went beyond them by specifically quantifying how race/ethnic disparity differences are delineated across specific community-level social vulnerabilities. Specifically, ML-vulnerability of the community more strongly influenced disparities in radiation therapy receipt versus other SDoH factors, suggesting that the racial-ethnic makeup and language capacity inherent in a Non-White GIC-patient community needs to be addressed to improve care of these individuals.
Alongside this influence, SES-vulnerability also showed substantial impact in effecting poor multi-modal treatment receipt for non-white patients compared to white patients. Although race-ethnicity has been examined relative to SES among patients undergoing surgery [35, 36], the impact and interaction of race/ethnicity and SDoH on non-operative GIC therapy such as chemotherapy and radiation therapy has not been studied until this present study. Furthermore, lesser-studied SDoH such as housing-transportation type and household composition were also identified as important drivers of multi-modality care of patients with GIC, indicating that multifaceted social vulnerability impacted not only surgery but also receipt of radiation therapy receipt among both White and Non-White GIC patients.
Given these vast differences in treatment receipt, this study also analyzed the downstream effect of social vulnerability on worse overall survival among many patients GIC. In fact, the impact on survival ranged from as high as a 21% decrease in survival length across observed vulnerability trends, with an increased detrimental effect on survival observed among Non-White GIC-patients with a majority of GIC versus White individuals. Compared to prior literature, these trends of downstream multi-modal treatment effects were not only present within solid tumor-based SVI studies, such as ours and the ones prior referenced, but also in hematologic cancer types ranging upwards of over 50% survival differences [37, 38].
Since the pandemic, social vulnerability has been a focus of public health initiatives, (e.g., hundreds of COVID-19 test based in areas of high social vulnerability) [39]. Within GIC, adoption of similar outreach efforts are needed to implement policies aimed at addressing some of the SDoH subthemes identified in the current study (i.e., transportation, language barriers, economic mobility, etc.). For instance, publicly led initiatives, such as the CDC-sponsored tobacco cessation programs in Mississippi or accessible testing programs in New York City [40], have utilized information derived from large-data analyses to allocate resources. As national support for cancer equity grows [41], public health efforts and investigations, such as increased low-cost screening availability in socially vulnerable areas or the provision of supportive care services of transportation and fee waivers for vulnerable GIC patients, should continue to derive thoughtful action based on innovative, large-data investigations to understand and address the multifaceted impact of SDoH in GIC and the broader oncologic field.
Despite the strengths of this study, there were several limitations. The SEER database did not encompass variables to characterize details on operation and systemic treatment (e.g., sequence), including the lack of data on immunotherapies. In addition, most of the study population was White, which may have skewed the results. Although constituted by 15 SDoH-factors, the CDC-SVI did not measure all SDoH that would be of clinical interest, as more detailed measures cannot be ascertained due to the design of CDC-SVI.
Author Contributions
David J. Fei-Zhang: conceptualization (lead), data curation (lead), formal analysis (lead), funding acquisition (lead), investigation (lead), methodology (lead), project administration (lead), resources (lead), software (lead), validation (lead), visualization (lead), writing – original draft (lead), writing – review and editing (lead). David J. Bentrem: conceptualization (equal), investigation (equal), methodology (equal), project administration (equal), resources (equal), supervision (supporting), validation (equal), visualization (equal), writing – review and editing (equal). Jeffrey D. Wayne: conceptualization (equal), data curation (equal), investigation (equal), methodology (equal), project administration (equal), resources (equal), supervision (supporting), validation (equal), visualization (equal), writing – review and editing (equal). Lifang Hou: conceptualization (supporting), investigation (equal), methodology (equal), project administration (supporting), resources (supporting), supervision (supporting), visualization (equal), writing – review and editing (supporting). Peiwen Fei: conceptualization (equal), data curation (supporting), funding acquisition (supporting), investigation (equal), methodology (equal), project administration (equal), resources (equal), software (supporting), supervision (equal), validation (supporting), visualization (supporting), writing – original draft (equal), writing – review and editing (equal). Timothy M. Pawlik: conceptualization (equal), data curation (equal), formal analysis (equal), funding acquisition (equal), investigation (equal), methodology (equal), project administration (equal), supervision (equal), validation (equal), visualization (equal), writing – original draft (equal), writing – review and editing (equal).
Conflicts of Interest
The authors declare no conflicts of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control and Prevention or the National Cancer Institute.
Open Research
Data Availability Statement
All authors had full access to all the data in the study and take full responsibility for the integrity of the data and the accuracy of the data analysis. These data and their defined variables are publicly available through the SEER administrators (https://seer.cancer.gov/index.html) and the CDC-SVI website (https://www.atsdr.cdc.gov/placeandhealth/).