DNA damage response signaling: A common link between cancer and cardiovascular diseases
Abstract
DNA damage response (DDR) signaling ensures genomic and proteomic homeostasis to maintain a healthy genome. Dysregulation either in the form of down- or upregulation in the DDR pathways correlates with various pathophysiological states, including cancer and cardiovascular diseases (CVDs). Impaired DDR is studied as a signature mechanism for cancer; however, it also plays a role in ischemia-reperfusion injury (IRI), inflammation, cardiovascular function, and aging, demonstrating a complex and intriguing relationship between cancer and pathophysiology of CVDs. Accordingly, there are increasing number of reports indicating higher incidences of CVDs in cancer patients. In the present review, we thoroughly discuss (1) different DDR pathways, (2) the functional cross talk among different DDR mechanisms, (3) the role of DDR in cancer, (4) the commonalities and differences of DDR between cancer and CVDs, (5) the role of DDR in pathophysiology of CVDs, (6) interventional strategies for targeting genomic instability in CVDs, and (7) future perspective.
1 INTRODUCTION
Genome integrity is constantly endangered by thousands of factors that are capable of inducing DNA damage each day.1 DNA lesions can arise from either endogenous normal metabolic processes or exogenous physical and chemical factors. Endogenous cellular processes include the production of reactive oxygen species (ROS) that can trigger oxidative base lesions and DNA mismatch errors caused by DNA polymerase enzymes during replication.2 Exogenous factors include ionizing and ultraviolet (UV) radiation that can trigger the formation of roughly 105 DNA lesions such as3, 4 photoproducts and pyrimidine dimers per cell everyday.5 Ionizing radiation in sunlight or therapeutic radiation can instigate single-strand breaks (SSBs) and double-strand breaks (DSBs) in the DNA backbone. Chemical factors including smoke, vehicle exhaust and factory fumes, and chemotherapy agents, such as bleomycin and cisplatin, can also give rise to DNA damage by hindering the DNA topoisomerase enzyme activity or adding alkyl groups to bases. Other factors, such as infection by microorganisms can also lead to DNA damage.3 The accurate and rapid restoration of DNA following damage is pivotal for cell survival and for preserving genomic integrity. Genomic instability caused by inaccurate or defective DNA repair can negatively impact the genetic code and lead to the accumulation of mutations, which eventually increases the incidence of carcinogenesis.6 Accordingly, cells have evolved intricate mechanisms to confront and repair DNA lesions, collectively known as the DNA damage response (DDR) signaling. DDR involves a coordinated network of proteins, including sensors, transducers, and effectors, which altogether create a complex signaling cascade to respond to genotoxic stress. As summarized in Figure 1, the DDR system is mainly conducted by the phosphoinositide 3 kinase proteins (PI3Ks): ataxia-telangiectasia-mutated (ATM), ATM- and RAD3-related (ATR), and DNA-dependent protein kinase (DNA-PK) and by the poly (ADP-ribose) polymerase (PARP) proteins. DNA-PK and ATM mainly mediate the detection and repair of DSBs,6 whereas PARP1 and ATR are activated by SSB lesions created at DSB sites or collapsed replication forks.6, 7
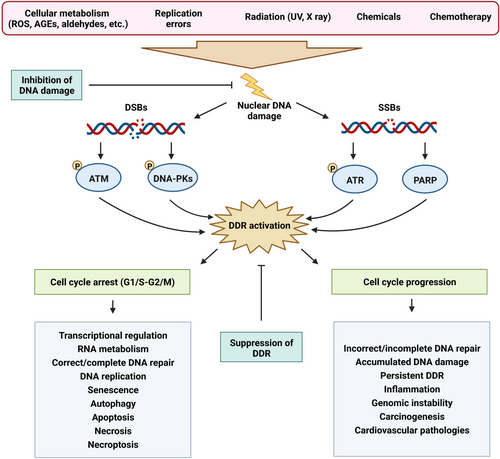
Normally, once the DDR cascade is initiated, cells undergo transient cell cycle arrest to repair the damaged DNA, a process ending in proper DNA repair and DDR inactivation.8 However, excessive or persistent DNA damage or DDR activation can result in accumulated DNA damage and trigger cell death, senescence, or tumorigenesis.5 DDR activation may exert differential effects depending on the cell type. The cardiovascular system consists of multiple cell types, including fibroblasts, vascular smooth muscle cells (VSMCs), cardiomyocytes, immune, progenitor, epithelial, and endothelial cells. A growing number of in vitro and in vivo studies have demonstrated the presence of DNA damage in nearly all cell types of the cardiovascular system, and genomic instability has been suggested as a potential factor in the development and/or progression of CVDs although remaining greatly underexplored. The purpose of this review is to thoroughly discuss different DDR mechanisms, their functional cross talk, the role of DDR in malignancies as well as CVDs, the common features and differences of DDR in cancer and CVDs, as well as therapeutic strategies targeting DNA damage and DDR in CVDs.
2 DNA DAMAGE RESPONSE SIGNALING PATHWAYS
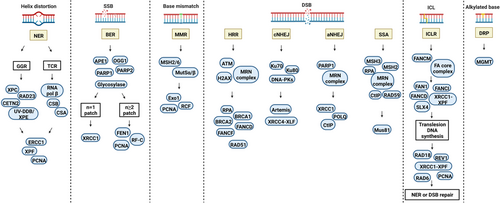
The DDR network generally includes the following six different pathways as briefly summarized in Figure 2.
2.1 Single-strand break repair
2.1.1 Nucleotide excision repair (NER)
Large DNA lesions that disturb the structure of the DNA helix are recognized and removed by NER.9 NER involves the removal of DNA adducts produced by UV radiation (cyclobutane pyrimidine dimers), 6-4 photoproducts, or DNA lesions generated by ROS, environmental carcinogens (benzo[a]pyrene), or genotoxic drugs (cisplatin and melphalan).10, 11 NER can be categorized into two sub-pathways (Figure 2) such as global genome repair (GGR) and transcription-coupled repair (TCR). The only difference between these sub-pathways is in the recognition of DNA damage. In GGR, helix distortion caused by DNA adduct initiates the employment of the damage detection factor XPC/RAD23/CETN2 and UV-DDB, whereas, in TCR, detection of damage is induced by a stalled RNA polymerase β upon a DNA damage site which is then removed by Cockayne syndrome A (CSA) and B (CSB) proteins to facilitate the accessibility of the lesion for NER proteins. After the detection of damage, both GGR and TCR progress via common pathways. Defective NER can result in several human genetic disorders associated with photosensitivity.12
2.1.2 Base excision repair (BER)
BER mediates the recognition and removal of damaged DNA bases, which are not typically helix-distorting.13 DNA lesions recognized by BER are created by spontaneous hydroxylation or deamination of bases, through oxidation of nucleotides by ROS produced as the result of either normal metabolism or environmental stresses (ionizing radiation, oxidizing chemicals, or smoking)14 or by alkylation of bases produced via endogenous or exogenous elements (antineoplastic drugs and carcinogens), all of which are able to trigger mutations if left unrepaired.15 There are two sub-pathways of BER, termed as short-patch or single-nucleotide and long-patch (Figure 2). The activation of each sub-pathway is dependent on the source and nature of DNA damage, the nature of the abasic (apurinic/apyrimidinic) site, and the ongoing cell cycle phase. The short-patch route handles single-base lesions in the G1 phase. On the other hand, the long-patch route is involved in the resynthesis of larger lesions (2–8 nucleotides neighboring the apurinic/apyrimidinic site) during S or G2. DNA glycosylases are among the most important BER enzymes that perform the hydrolyzation of the N-glycosylic bond between the sugar-phosphate backbone and the damaged base, generating an apurinic/apyrimidinic intermediate site.15
2.1.3 Mismatch repair (MMR)
MMR is the major mechanism for the preservation of replication fidelity. MMR handles the removal of base insertion/deletion and substitution mismatches caused by replication errors evading the proofreading activity of DNA polymerases.16 DNA lesions are recognized by Mutator Sα (MutSα), a heterodimer complex consisting of the DNA mismatch repair proteins Mutator S homolog 2 (MSH2), and MSH6. MutSβ is another heterodimer complex that contains MSH2 and MSH3 and binds only to insertion/deletion mismatches. Upon damage recognition, Mutator Lα (MutLα) [MLH1/postmeiotic segregation increased 2 (PMS2)] or MutLβ (MLH1/MLH3) endonucleases cut DNA near the damage site. The enzyme 5′ exonuclease 1 (Exo1) enters the damage site through the nick, then degrades DNA past the mismatch. The resultant ssDNA gap is filled in and sealed by polymerase δ and DNA ligase I, respectively.17, 18 Defects in MMR can cause microsatellite instability and is related to certain prognosis, clinical features, therapy response, and immune checkpoint blockade.19, 20
2.2 Double-strand break repair
DSBs can be the product of both exogenous factors, such as genotoxic drugs and ionizing radiation,7 and endogenous events, such as replication fork collapse, oxidative stress, and telomere erosion.21 DSBs can also occur as a part of programmed cellular events during meiosis, V(D)J recombination, and class-switch recombination.22 However, unrepaired DSBs are severely dangerous for cells as they can lead to mutations, chromosomal abnormalities, and cell death.23 Cells have developed the following mechanisms to repair DSBs (Figure 2).
2.2.1 Homologous recombination repair (HRR)
HRR is a major contributor to error-free DDR that acts during the S and G2 stages of the cell cycle to locate a large homologous DNA sequence on a sister chromatid that can be utilized as a template for resynthesizing damaged or missing bases.24 DSBs are recognized by histone H2AX, the mediator of DNA damage checkpoint protein 1 (MDC1), and RING finger protein 8 (RNF8). Upon activation of mediator proteins including Rap80, Abraxas, and BRCA1, 5ʹ-3ʹ DNA end resection is performed by the MRN complex, which includes MRE11–RAD50–NBS1 (Nijmegen breakage syndrome protein 1), to generate a 3ʹ ssDNA tail. The MRN complex also binds to the BRCA1–CtBP-interacting protein (CtIP) complex which is necessary to activate the DNA damage signaling kinases ATM, ATR, and CHK2.25-27 The ssDNA is then coated with the replication protein A (RPA) to prevent it from binding to other ssDNA molecules in the form of spurious secondary structures. RPA also serves as a platform for the loading of RAD51 recombinase and must be removed by recombination mediators to enable RAD51 filament formation.28 The formation of BRCA1–partner and localizer of BRCA2 (PALB2)–BRCA2 complex is required for RAD51-dependent HRR. There are three sub-pathways of HRR, activation of which is dependent on how two DNA ends interact at the recombination synapse and operate on the D-loop created after the formation of synapsis. The major repair pathway in somatic cells is the noncrossover synthesis-dependent strand annealing. The creation of a double Holliday junction intermediate can result in crossing over in meiotic cells. If cells fail to involve the second end of the break or fail to replace the nascent strand, abnormal replicative HRR responses including long tract gene conversion and break-induced replication will occur. BRCA2 acts as the major mediator of recombination in vertebrates and in several fungal species.29-31 BRCA2, which is constitutively bound to the proteasomal component DSS1, interacts with both ssDNA and RAD51 monomers and with BRCA1–BARD1 via the PALB2 protein.32
2.2.2 Canonical nonhomologous end joining (cNHEJ)
cNHEJ is an error-prone DNA repair mechanism that operates during the entire cell cycle and entails the interaction of the Ku70–Ku80 (also known as XRCC6–XRCC5) heterodimer to DNA ends at DSBs. cNHEJ involves a two-step mechanism of DNA end synapsis.33 First, a long-range synapsis is established by Ku70–Ku80 and DNA-PKs; then, the two ends become closely associated via XLF, XRCC4–ligase IV, and DNA-PKs kinase activity.34 Ku facilitates recruitment of other cNHEJ proteins such as the DNA-dependent protein kinase catalytic subunit (DNA-PKs), DNA ligase IV, and the associated scaffolding factors such as XRCC4, XRCC4-like factor (XLF), and paralog of XRCC4, and XLF (PAXX).35-39 DNA-PKs activate the XRCC4–ligase IV complex to religate the broken DNA ends. However, prior to binding, the MRN complex, the Flap Endonuclease 1 (FEN1), and Artemis operate together to process DSB ends.40, 41 Deficiencies in cNHEJ are associated with genomic rearrangements and chromosomal translocations,42 defective V(D)J recombination, and immune defects.43
2.2.3 Alternative nonhomologous end joining (aNHEJ)
aNHEJ, also referred to as microhomology-mediated end-joining, is another pathway of DSB repair.44 The most outstanding feature of aNHEJ is the utilization of 5–25 bp microhomologous sequences during the alignment of DSB ends prior to religation, thus giving rise to deletions that flank the original break.45 aNHEJ is often related to pathogenic chromosomal errors such as inversions, deletions, and translocations.46, 47
Complex regulatory mechanisms regulate the choice between the HRR and cNHEJ pathways. These mechanisms mainly involve competition between BRCA1, which favors HRR, and the p53-binding protein 1 (53BP1), which promotes cNHEJ. Histone H4 methylation by Multiple Myeloma SET (MMSET) leads to the employment of 53BP1 at the DSBs, preventing DNA end resection by the MRN complex, C-terminal binding protein 1 interacting protein (CtIP), and BRCA1. On the other side, acetylation of histone H4 by Tip60 (Tat-interactive protein) prevents 53BP1 employment while promoting BRCA1 occupancy and HRR. Cell cycle regulatory proteins including the cyclin-dependent kinases are also important in determining the pathway of choice to repair DSBs.22
2.2.4 Single-strand annealing (SSA)
SSA is a very efficient yet highly mutagenic mechanism to resolve DSBs.22, 49 Following a DSB between homologous repeats, DNA end resection creates 3′ ssDNA tails, giving rise to flanking homologous sequences which are annealed together to create a synapsedintermediate. Ligation is later performed by endonucleolytic cleaving of nonhomologous 3′ ssDNA tails and subsequent gap filling by a polymerase. SSA is genetically different from other HRR mechanisms since it operates independently of RAD51 and is dependent on the RAD52 paralog, RAD59, instead. SSA is essential to repair chromosomal DSBs that have undergone extensive end resection but cannot be restored by HRR or aNHEJ.50 However, SSA can be relatively mutagenic leading to rearrangement between repeat elements. The importance of the SSA repair mechanism is dependent on several factors, such as the cell cycle phase, the presence or absence of the sister chromatid, and the length of uninterrupted homology.50
2.2.5 Interstrand cross-link repair (ICLR)
DNA interstrand cross links can be formed by exogenous chemicals, such as cyclophosphamide, cisplatin, melphalan, psoralen, and mitomycin C,50 or endogenously produced aldehydes.51 Such lesions are considered critical because if left unrepaired, they can give rise to replication or cell cycle arrest and eventually cell death.52 Mammalian cells have developed three pathways for the detection of cross-links. ICLR adducts can be detected through disturbed DNA duplex by damage-recognizing factors, via interacting with the transcription machinery, and stalled replication fork, all of which trigger a repair response. In nonproliferating cells, ICLR is performed by NER and by the FANCM DNA translocase that enables nuclease entrance to the damage site. Interestingly, ICLR is integrated into the DNA replication system in S-phase cells and is dependent on HRR.53 In human cells, there are four distinct steps to accomplish ICLR: (i) the interstrand cross-link is unhooked on one strand, and a DSB is induced in a DNA replication-dependent manner, (ii) translesion DNA synthesis is performed by utilizing the unhooked interstrand cross-link as a template, (iii) DSB is processed and the collapsed DNA replication fork is restored, and (iv) the residual unhooked interstrand cross-link is removed.54 Defects in proteins of the ICLR pathway play central roles in the pathophysiology of Fanconi anemia,55 Cockayne syndrome,56 trichothiodystrophy,57 xeroderma pigmentosum,58 and cerebro-oculo-facio-skeletal syndrome.59
2.2.6 Direct repair pathway (DRP)
The most distinguishing property of the DRP is that it is a single-step route with only one protein, O6-methylguanine-DNA methyltransferase (MGMT), handling the process.61 The DRP is involved in the removal of aberrant alkyl groups caused by alkylating agents including procarbazine, dacarbazine, and temozolomide. MGMT removes alkyl groups from guanine or thymine and transfers them to a cysteine residue of MGMT.62 The alkylated MGMT is functionally deactivated and eliminated by the ubiquitin proteolysis pathway. If left unrepaired, alkyl adducts can lead to thymine mismatch during replication, causing G:C to A:T transitions or strand breaks.63
3 THE FUNCTIONAL CROSS TALK AMONG DISTINCT DNA DAMAGE RESPONSE PATHWAYS
The DDR pathways evaluate the scale and severity of DNA damage and trigger cell cycle arrest, repair, senescence, or apoptosis in the case of irreversible damage. If repair is initiated, one of the DDR routes mentioned above will be activated. Based on the type and extent of the damage, there is significant cross talk between the various DDR mechanisms (Figure 3). The detectors of DDR signaling activate mediators and effectors by employing them at the DNA damage site. The ATM pathway operates throughout the entire cell cycle. Following DSB formation, the break site is recognized by the MRN sensor complex which employs the transducer kinase ATM at the break site.28, 64 ATM activation then results in the phosphorylation of H2AX as well as its ubiquitination by RNF8 and RNF168, resulting in the employment of downstream effectors BRCA1, BRCA2, and 53BP1.65, 66 In addition, the phosphorylated H2AX, known as γH2AX, facilitates the interaction of MDC1 at the damage site, where it is later phosphorylated by ATM.67 This precedes the phosphorylation and activation of cell cycle checkpoint proteins such as CHK2 and p53 that trigger cell cycle arrest to inhibit replication of damaged and/or unrepaired DNA.6 The tumor suppressor protein p53 is a critical sensor of DNA damage that functions downstream to ATM/ATR/DNA-PK and plays a central role in the maintenance of genome integrity by deciding between the dilemma of cell cycle arrest or apoptosis.
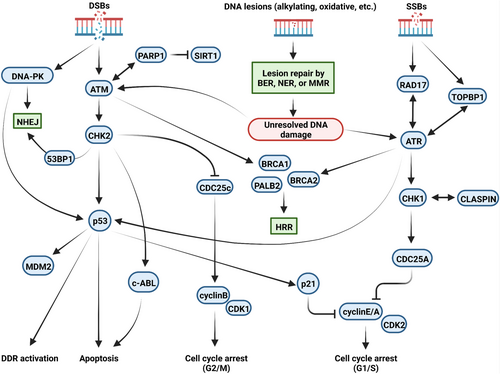
On the other hand, ATR is activated at ssDNA regions formed at DSB overhangs or collapsed replication forks6 and acts in an ATM-dependent manner in the S and G2 phases of the cell cycle.68, 69 Indeed, it is now well known that the ATR pathway is also capable of activating downstream elements of the ATM arm.70 Upon replication fork collapse or UV treatment, ssDNA regions are quickly coated by RPA. This leads to the recruitment of ATR to the site of DNA damage via interacting with ATR-interacting protein (ATRIP).71 Several protein complexes such as the RAD17-replication factor C 2 (RFC2) clamp loader complex and the RAD9-RAD1-Hus1 (9-1-1 complex) are serially employed in the RPA-coated ssDNA, which eventually leads to the localization of topoisomerase II binding protein 1 (TOPBP1). The interactions of TOPBP1 with ATRIP and RAD of the 9-1-1 complex result in ATR activation,72 which precedes the phosphorylation of p53 and CHK1 effector proteins, cell cycle arrest, and DNA repair.72 Unlike the ATM and ATR kinases, DNA-PK is involved in the DSB repair via the NHEJ pathway. DNA-alkylating agents are capable of activating both ATM and ATR pathways. Although these agents inflict stress on advancing replication forks, they can also trigger strand breaks in some cases.73
4 DNA DAMAGE RESPONSE SIGNALING IN CANCER
In the section above, the essential role of the various DRS mechanisms in guarding the genome integrity is thoroughly explained. It is not surprising that deficiencies in any of these pathways would be deleterious for cell physiology. Aberrant operation or overburdening of DDR mechanisms and/or checkpoints can lead to the accumulation of mutations, which may initiate a series of events that finally lead to genomic instability and malignant transformation (Figure 1). In order to provide a comprehensive signature of aberrations associated with carcinogenesis, more than 9000 samples, including 33 different cancer types, were investigated by the Cancer Genome Project and Cancer Genome Atlas. These mutations can be generally classified as “driver,” which directly triggers tumor formation and development, and “passenger,” promoting cancer development as a consequence of their accumulation.74 In about a third of the cases, somatic mutations associated with DDR genes were observed. One example is the MLH1 and MSH2 mutations that result in dysfunctional MMR and thereby defective recognition and restoration of replicative lesions on DNA which eventually prime malignant outcomes75 or predisposition to cancer.76 Due to the central role played by DDR in malignant transformation and the associated consequences, anticancer therapies mostly target DDR either directly or indirectly.77, 78 There is a high probability that different DNA damage thresholds exist at distinct stages of tumor progression.79 The DDR pathway is quickly primed and precisely controlled in tumor cells as in normal cells, which suggests the possibility of targeting certain steps and proteins of the DDR machinery to hinder tumor growth. However, DDR is a double-edged sword in the context of cancer development and therapy. The DDR contributes to tumor cell protection and survival as it repairs their restorable DNA damages, also when they are primed by DNA-targeted therapies. This event is a major pathway in generating resistance to a genotoxic intervention. Any missing or defective canonical pathways of DDR can result in the dysregulation of DNA restoration routes leading to genomic instability which is a significant hallmark of cancer. Aberrant mechanisms may be finally compensated to substitute DDR routes creating an environment that highly promotes tumorigenesis and resistance to genotoxic treatments.80 DDR in cancer is reviewed in detail elsewhere.81
5 DNA DAMAGE RESPONSE SIGNALING: COMMONALITIES AND DIFFERENCES BETWEEN CANCER AND CARDIOVASCULAR DISEASES
5.1 DNA damage response in cardiovascular diseases
While originally considered two distinct diseases, recent investigations have revealed remarkable commonalities between CVDs and cancer, including common risk factors and intracellular pathways for disease development and progression. Of particular interest, many of the “hallmarks of cancer,” such as inflammation, genomic instability, cellular proliferation, cell death, therapy resistance, and angiogenesis represent the pathophysiologic routes common to both cancer and CVDs.82 A growing amount of clinical and preclinical evidence has revealed the presence of DNA damage and activation of DDR signaling in CVDs.83-85 While DDR activation was initially assumed to be a cell cycle arrest response limited to dividing cells, it became evident that DDR is also activated in postmitotic cells such as cardiomyocytes.86 Enhanced senescence and apoptosis secondary to DDR were observed in atherosclerotic lesions.99, 106, 107 Accumulated DNA damage was shown to be positively correlated with the severity of atherosclerosis in human coronary artery disease.87 Among different genomic insults orchestrating cardiovascular pathology, ROS represents the key endogenous culprit that leads to the formation of oxidative DNA lesions such as base oxidations, SSBs, DSBs, and telomere shortening.5, 88 An increase of BER markers following oxidative DNA damage84 suggests the critical role of ROS in the accumulation of DNA damage in atherosclerotic 22ques. Although mitochondrial DNA damage is also involved in the pathogenesis of CVDs,89 here we will only discuss the nuclear DNA damage signaling in CVDs.
DNA DSBs have been detected during genomic stress in roughly all cardiovascular cell types.84, 89-91 Theoretically, HRR is not likely to take place in postmitotic cardiomyocytes due to cell cycle restriction. Nevertheless, upregulation of BRCA1 was identified in the postischemic human myocardium.84 Although, in mice, depletion of BRCA1 in cardiomyocytes resulted in increased γH2AX and decreased RAD51-foci indicating loss of DSB repair leading to DSB accumulation and impaired cardiac function in myocardial ischemia, however, there was no direct evidence of HRR repair in cardiomyocytes.84 Increased DNA damage and upregulation of MRN complex were observed in VSMCs of human atherosclerotic lesions, suggesting the presence of HRR.91 In contrast to homologous recombination, a role for NHEJ was identified in endothelial cells from atherosclerotic plaques.92 Here, decreased expression of lncRNA SNHG12 was attributed to decreased interaction of Ku70-Ku80 and DNA-PKs, leading to impaired DDR activation and vascular senescence.92 In an independent study, human atherosclerotic plaques were shown to contain accumulated DSBs and activated ATM in comparison to healthy tissue.104
DNA SSBs, on the other hand, are the most frequent outcome of oxidative stress. In proliferating cells, the most common outcome of SSBs is replication fork repression, which subsequently results in DSB formation.94 On the other side, cell death induced by SSBs in nondividing cells such as cardiomyocytes involves RNA polymerase and activation of PARP1 (the SSB sensor).94 XRCC1 depletion in cardiomyocytes increased SSBs, DDR activation, and inflammation.95 Moreover, the critical role of NER in cardiovascular pathology was confirmed using NER-defective murine models, Ercc1d/− and XpdTTD, which demonstrated an enhanced vascular stiffness, senescence, and compromised vasodilator function with aging.96 Together, these findings highlight the significance of genomic instability and DDR activation as the central modulators of CVD progression.
5.2 Cancer and cardiovascular dysfunction in genomic instability syndromes (GIS)
In humans, a mutation in certain genes of DDR leads to autosomal recessive syndromes called progeroid syndromes (PS) or GIS. It should be noted that some GISs are associated with senescence, others manifest with susceptibility to cancer, and some exhibit both phenotypes.97 Some syndromes are important in the study of CVDs since affected patients show early onset atherosclerosis, diabetes, and dyslipidemia.97 Mutation of ATM in humans can lead to a distinctive GIS, called Ataxia-telangiectasia syndrome (ATS), in homozygous patients in addition to predisposing them to cancer.98 ATM mutation carriers were reported to have higher mortality rates compared with noncarriers due to the occurrence of ischemic heart disease and cancer.98, 99 Heterozygous patients for the ATM allele display an enhanced risk of death from ischemic heart disease in comparison with noncarriers.124 As mentioned before, ATM plays a critical role in DDR by contributing to DSB repair and regulation of cell cycle checkpoint, senescence, and apoptosis. Among myriad downstream targets of ATM, p53 plays a key role by modulating the transcription of numerous target genes.97 However, studies investigating ATM function in p53 knockout mice reported that there are also p53-dependent, ATM-independent routes leading to apoptosis and senescence.92, 97, 100 ATS patients demonstrate accumulated DSBs and chromosomal breakages, defective cell-cycle checkpoints, and sensitivity to ionizing radiation. Therefore, ATM plays a critical role in maintaining genomic stability and reducing the risk of cancer and other diseases.
Werner syndrome (WS) is another GIS, which is defined by the early onset of signs of aging as well as atherosclerosis, diabetes, and a high incidence of malignancies.108, 109 The main causes of death in WS include myocardial infarction, stroke, and cancer. The WRN protein (encoded by the WRN gene) comprises a RecQ-type helicase and an exonuclease domain and exhibits SSA activity110, 111 and telomere maintenance.110, 112 WRN-knockdown cells are more sensitive to DSB-inducing agents and exhibit accumulated DSBs and increased DDR rate.113 WRN protein contributes to HRR by interacting with BRCA1, RAD51, and RAD52. WRN also acts in concert with key molecules of NHEJ including Ku and DNA-PKs.97 Extensive deletion is detected at ends joined by NHEJ in cells from WS patients.114 Several studies have shown that WRN-knockdown cells exhibit defective BER and thus contain accumulated oxidative DNA damage.115, 116 Finally, WRN plays a key role in the maintenance of telomeres and telomere abrasion is the main mechanism in WS pathogenesis. Telomeres are remarkably truncated in WS cells, and telomerase introduction helps improve lifespan and decrease chromosomal aberration in these cells.117-119 Mice that were double-knockout for WRN and the telomerase RNA component (TERC) manifest clinical features of WS patients,97, 101, 102 whereas WRN deficiency alone did not result in premature aging.122
In addition to ATM and WRN, accumulating evidence from recent investigations highlights the role of BRCA1, BRCA2, and p53 proteins in the pathophysiology of CVDs. Germline mutations in either one of BRCA1 and BRAC2 primarily predispose carriers to hereditary breast and ovarian cancer (HBOC) syndrome, which is inheritable in an autosomal-dominant manner, as well as other cancer syndromes.103 HRR mediated by BRCA1 and BRCA2 was suggested to be a central phenomenon in the pathophysiology of CVDs as previously mentioned in this review. Studies suggest that BRCA1 and BRCA2 mutation carriers show excessive noncancerous mortality, especially at older ages,104, 105 which may be due to complications of CVDs. While p53-induced apoptotic cell death is considered a protective route against tumor development, pro-apoptotic p53 function is particularly damaging in the context of CVDs.106, 107 Activation of p53 by oxidative stimuli or other DNA damage sources can lead to numerous cardiovascular complications including atherosclerosis, thereby presenting a link between cancer and CVDs. Systemic deletion of BRCA1 and BRCA2 causes embryonic lethality in mice and the developing embryos exhibit defective cellular proliferation related to induction of the p53 pathway.108 The same study reported that heterozygous deletion of p53 can in part rescue the embryonic lethality caused by systemic BRCA1 and BRCA2 loss and that p21 mutation delays the onset of the lethality in BRCA1 mutants. These findings demonstrate that p53 and p21 are two significant modulators of cell cycle progression and play critical roles in the progression of BRCA1- and BRCA2-mutant phenotypes.108 Intriguingly, p53 loss was reported to protect the heart from rupture and subsequent death while upregulation of p53 promoted apoptosis in cardiomyocytes.85, 109-112 Taken together, investigations on the role of genomic instability and DDR in the prediction of cardiovascular risk can open a new window into broadening our knowledge of the common pathophysiological processes in cancer and CVDs.
5.3 p53: Different regulatory functions in cancer and cardiovascular diseases
The tumor suppressor p53 is the primary responder to cellular stress stimuli such as oncogene expression, DDR, ribosomal dysfunction, oxidative stress, and hypoxia. p53 activation triggers myriad cellular mechanisms which collectively induce cell cycle arrest to maintain genomic integrity, senescence, ferroptosis, or apoptosis to remove irrecoverable cells. Thereby, p53 is known as the “guardian of the genome” which prevents the accumulation of pro-tumorigenic mutations.112, 113 TP53 is the most commonly mutated gene in human cancers.114 Germline mutations in TP53 result in the Li Fraumeni syndrome cancers115 and also are linked to adverse prognoses in numerous sporadic cancers.114 From a functional perspective, p53 mutants not only result in the loss of wild-type p53 functions but can also obtain oncogenic gain-of-function activity, leading to a dominant negative effect through creating hetero-tetramers with the wild-type p53 expressed from the other nonmutated allele.116 Loss-of-function mutations in p53 render a substantial advantage during tumorigenesis by allowing cells to evade intrinsic tumor suppressive mechanisms including cell death and senescence. Gain-of-function mutations, on the other hand, enable p53 to acquire new transcriptional targets,117 such as p63, p73, NF-Y, Sp1, ETS1/2, NF-κB, ATM, and SMADs, modifying the metabolism, cell cycle, and apoptosis of tumor cells and promoting genomic instability, cell proliferation, metastasis, and therapy resistance.118
p53 also exerts essential regulatory effects on the cardiovascular system during physiological processes such as embryonic heart development and adult heart homeostasis119, 120 as well as during the development of CVDs including atherosclerosis, myocardial IRI, heart failure, diabetic-induced or pressure-overload maladaptive remodeling, and chemotherapy-induced cardiotoxicity.121-124 In the vasculature, p53 regulates the progression of CVDs through pro-apoptosis, pro-necrosis, antiangiogenesis, and pro-autophagy activities as well as regulation of inflammation, metabolism, and cell cycle arrest.125, 126 It is important to note that p53 functions can lead to different outcomes in the cardiovascular system compared with cancer cells in terms of the pathophysiology of the disease. Contrary to the canonical role p53 plays as a tumor suppressor, its upregulation and activation can exacerbate the progression of CVDs by promoting cell death and/or phenotypical changes in the cells of the cardiovascular system. Under physiological circumstances, p53 is retained at low levels by the ubiquitin-proteasome system.127 Basal levels of p53 maintain normal cardiac function and architecture by regulating the expression of cardiac architecture-related proteins. p53 has different functions in cardiomyocytes and nonmyocytes. While p53 primarily regulates metabolism and programmed cell death in cardiomyocytes, it controls angiogenesis and cell cycle arrest in nonmyocytes. A growing body of research has shown an increased p53 expression and activation in numerous CVDs such as late-stage heart failure.128 Upon stimulation by stress, p53 is subjected to several translational or posttranslational modifications such as phosphorylation, ubiquitination, acetylation, glycosylation, and SUMOylation in CVDs. p53 regulates angiogenesis by suppressing the expression of angiogenic mediators.129 Endothelial cell-specific p53 knockout was shown to promote angiogenesis in a murine hindlimb ischemia model.130 Endothelial p53 expression was also increased in mice fed with a high-fat diet.131 Additionally, high-fat diet-induced eNOS (endothelial nitric oxide synthase type III enzyme) dysfunction was restored via p53 knockdown in endothelial cells.132 Low-grade expression of p53 is not pro-apoptotic, but it results in reversible cell cycle arrest133 and inhibits migration of endothelial cells via downregulation of β-3 integrin.134 The principal role of p53 in atherosclerosis was demonstrated using apoE −/− p53 −/− double-knockout mice fed with a high-fat diet.135 These animals demonstrated increased hypercellular lesions in their aorta.135 Later, it was shown that p53 deficiency in subendothelial macrophages promoted atherosclerotic lesions.136 Furthermore, p53 plays a critical role in vascular senescence. Disturbed blood flow triggers endothelial cell apoptosis via p53 SUMOylation, a phenomenon that was ameliorated in p53−/−mice.137 In endothelial cells, prolonged IFN-γ treatment triggered senescence through the accumulation of γH2AX foci and upregulation of p53 and p21. Additionally, ATM knockdown alleviated IFN-γ-induced cellular senescence.138 Treatment of endothelial cells with hydrogen peroxide also induced senescence through p53 and NAD-dependent deacetylase sirtuin-1 (SIRT1).138 Reduced endothelial SIRT-1 expression during aging139 augments genomic instability, leading to p53 activation and exacerbation of senescence.140, 141 Taken together, these findings highlight the role of p53 activation secondary to stress stimuli such as oxidative stress and DNA damage in the modulation of endothelium function and progression of CVDs.
6 DNA DAMAGE RESPONSE SIGNALING IN THE PATHOPHYSIOLOGY OF CARDIOVASCULAR DISEASES
The overall role of DDR in the pathophysiology of CVDs is briefly summarized in Figure 4.
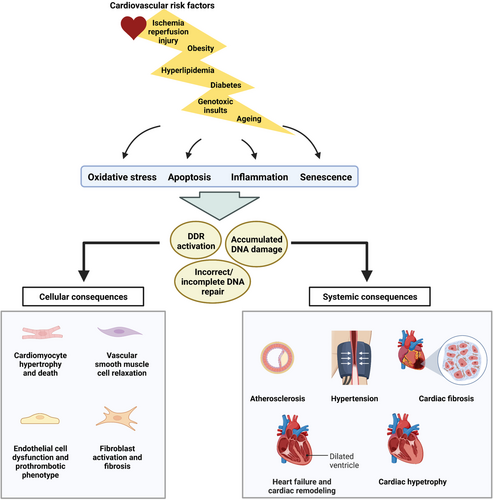
6.1 Oxidative stress, atherosclerosis, and aging
It is widely accepted that factors related to the development of CVDs can trigger the generation of ROS and lead to oxidative DNA damage and subsequent senescence by targeting both nuclear and mitochondrial DNA (thoroughly reviewed in75, 76). ROS can be a by-product of endogenous biochemical processes such as mitochondrial respiration, membrane NADH/NADPH oxidase, peroxisomes, endoplasmic reticulum, and uncoupling of NOS or exposure to exogenous stimuli such as chemotherapeutic agents (cisplatin and doxorubicin) and ionizing radiation that affect the function of the aforementioned enzymes and organelles.142, 143 ROS regulate a variety of signaling pathways that can lead to endothelial cell dysfunction, premature aging, and atherosclerosis progression.144, 145 ROS induce DNA damage by generating oxidized nucleoside bases such as 7,8-dihydro-8-oxoguanine (8-oxoG),146 which results in G-A or G-T transversions if left unrepaired. Atherogenic risk factors such as smoking and diabetes induce oxidative DNA damage, impair DDR, and accelerate the formation of mutagenic advanced glycation end products (AGEs).147 Increased oxidative stress and reduced antioxidant levels together with impaired DDR can gradually lead to the progression of atherosclerotic coronary disease.148, 149 Oxidized bases are typically resolved by the BER system; however, simultaneous formation of oxidized bases on opposing strands can result in the generation of DSBs by BER.150 Levels of 8-oxoG and DNA strand breaks were higher in patients with atherosclerosis compared to a normal cohort with multiple reports stating a correlation in levels with disease severity.86, 151 Martinet et al. reported enhanced immunoreactivity to DNA damage markers and upregulation of DDR proteins in atherosclerotic plaques of carotid artery.152 In vitro, BRCA1- and BRCA2-deficient endothelial cells are associated with increased inflammatory and oxidative stress-induced ROS production, accumulation of DNA damage leading to apoptosis, and/or endothelial dysfunction,153, 154 which play integral roles in the development of various CVDs. In another study, human atherosclerosis was related to VSMC senescence which demonstrated elevated levels of 8-oxoG and remarkable telomere shortening.155 Mice that were knockout for OGG1 (a BER protein that removes 8-oxoG from DNA) in VSMCs showed elevated oxidative stress, DNA-strand breaks, activation of pro-inflammatory mechanisms, and extensive atherosclerosis.91 DNA damage can result in apoptosis in cells with accumulated DNA damage and impaired DDR as well as in cells that are triggered to proliferate. In atherosclerotic plaques, apoptosis is detected in endothelial cells, macrophages, and VSMCs. While VSMC apoptosis can trigger attenuation of the fibrous cap and plaque rupture, endothelial cell death is evident in both atherogenesis and plaque erosion.156 Apoptosis can be triggered by ROS in vascular endothelium where it is exacerbated by p53, leading to plaque rupture.157 Although accumulating evidence demonstrates DDR activation in atherosclerosis, cells exhibiting DNA damage are much more frequent compared with ones that exhibit apoptotic markers, indicating that DDR is activated to prevent cell death.152 Systemic low-density lipoprotein receptor (LDLR) knockout mice that were fed a high-lipid diet expressed higher p53 levels along with disturbed flow-induced senescence mediated by the p53–p21 pathway.158 p21 knockout mice exhibited accelerated atherosclerosis following high-lipid diet consumption compared with their wild-type littermates.159 DDR markers in human plaques are related to activation of BER or nonspecific repair pathways.152 Mercer et al. showed that ATM knockout in ApoE-null mice leads to accelerated atherosclerosis.160 In plaques of thoracic aorta derived from cholesterol-fed rabbits, DNA damage was associated with the upregulation of DDR enzymes such as PARP1 and XRCC1.161 Although DNA breaks were normalized following four weeks of dietary lipid reduction, a remarkable reduction of 8-oxoG was only evident after a long period of diet modification, indicating the prolonged existence of DNA damage in atherosclerosis. Moreover, DDR proteins were significantly downregulated when switched to a normal diet.161 Taken together, these studies show that DNA damage and the subsequent DDR activation play central roles in atherosclerosis and may be repairable, at least in the early stages of atherosclerosis.
A great amount of ROS is produced throughout vascular aging.162 This ROS can be either a product of eNOS, when it is in the uncoupled state,163 or of other resources such as NADPH oxidase or mitochondria, which form free radicals upon interacting with NO. Overproduction of ROS can ultimately culminate in decreased NO bioavailability, formation of SSBs, 8-oxoG, and other oxidative lesions in vascular endothelial cells.164 Aberrant eNOS activity is closely related to genomic instability and dysfunctional vascular endothelial cells as observed in diseased and aged blood vessels. Downregulation of eNOS mRNA was correlated with overt DNA damage in human endothelial cells treated with oxidized LDL in vitro154 and with advanced atherosclerotic plaques in vivo.152 eNOS knockout mice demonstrated a variety of cardiovascular complications such as altered vascular remodeling, systemic hypertension, abnormal angiogenesis, and a prothrombotic phenotype.165-169 Apart from the critical role, eNOS plays in the initiation of DNA damage, genomic instability itself can result in the disturbance of NO signaling. Mice with genetic instability due to deficient ERCC1 (Ercc1d/− mice; involved in the NER pathway) demonstrated early onset vascular cell senescence, vasodilatory dysfunction, elevated blood pressure, and enhanced vascular stiffness. The impaired vasodilatory function was correlated with increased eNOS-activating phosphorylation at serine 1177 residue which subsequently resulted in reduced activation and production of eNOS and decreased NO-mediated vasodilation.95 Uncoupling of eNOS due to decreased tetrahydrobiopterin (BH4) bioavailability can lead to a switch from NO to ROS production. Similar to Ercc1d/− mice, age-dependent endothelial cell-mediated vasodilation was impaired in mice with XPD deficiency (XpdTTD mice; another gene involved in the NER mechanism).95 Moreover, mice that were transgenic for APE1/ref-1 (apurinic/apyrimidinic endonuclease 1/redox factor 1; plays major roles in DDR) manifested decreased vascular NO levels, dysfunctional endothelial cell-dependent vascular tone, and systemic hypertension.99 Taken together, aberrant eNOS activation and genomic instability can ultimately lead to progressive endothelial cell dysfunction which promotes vascular aging.
6.2 Metabolic stress
6.2.1 Diabetes
Patients with type 1 or type 2 diabetes show enhanced serum levels of glucose and AGEs which are considered diagnostic markers. As a result of obesity-related insulin resistance, type 2 diabetic patients exhibit increased levels of serum insulin and free fatty acids during the early stages of the disease. These pathophysiological factors were reported to induce DNA damage in vitro which may explain why diabetic patients show enhanced DNA damage in vivo.170 Hyperglycemia was shown to promote DNA DSBs in endothelial cells as well as increase 8-oxoG levels in endothelial and tubular cells.171, 172 The genotoxicity of AGEs was proven using numerous cell lines such as pig kidney cells,173 human liver and colon cells,174 and mouse podocytes.175 AGEs were also able to cause oxidation of DNA bases and trigger the generation of 8-oxoG in VSMCs.176 In diabetes-associated mutation, DNA damage caused by ROS can take place either through a direct or indirect pathway. Increased plasma levels of glucose, AGEs, insulin, and free fatty acids—all initiate ROS generation leading to direct DNA damage in type 2 diabetes.177 Additionally, diabetic patients demonstrate reduced antioxidative capacity such as decreased glutathione synthesis, which can result in susceptibility to oxidative damage.178 Indirect diabetes-associated DNA damage can take place via various signaling pathways such as the PI3K-Akt-tuberin pathway.179 Blasiak et al. reported decreased DDR efficacy in type 2 diabetic patients.180 Since impaired DDR may increase the proneness of cancer development,180 diabetic patients may also develop a greater risk for carcinogenesis.181 The effect of hyperglycemia on cellular oxidative stress and 8-oxoG levels has been investigated in human microvascular182 and human umbilical vein endothelial cells.183
6.2.2 Hyperlipidemia
Studies have demonstrated that obese patients who show enhanced risk for cancer also showed higher serum levels of free fatty acids and 8-oxoG, strengthening the notion that there is a possible correlation among free fatty acids, DNA damage, and carcinogenesis.184 Atheroma obtained from ApoE-null mice fed a high-fat diet contained increased DNA DSBs along with enhanced levels of poly ADP ribose, arising from PARP activity.161, 185 In addition, enhanced DNA damage, poly ADP ribose, and cell death were clearly detected within the atheromatous plaques in this model.185 Godschalk et al.186 assessed DNA etheno adducts in aortic cells derived from ApoE-null mice fed either a low- or a high-lipid diet and reported that the number of exocyclic adducts was inversely associated with the levels of total serum cholesterol. However, the expression of APE1/Ref1 was enhanced in these mice, suggesting that increased DDR caused by genotoxic lipid oxidation products is probably responsible for the observed decrease in DNA damage.186 Etheno adducts were also found in human atherosclerotic plaques as reported by the same researchers. Although few studies have confirmed the casual correlation between hyperlipidemia and DNA damage,160, 187-190 it appears that consuming a high-lipid diet can induce DNA damage in the cardiovascular system.
6.2.3 Obesity
Obesity is involved in the early onset of diabetes and atherosclerosis-associated diseases and it enhances the risk of death from CVDs.191 Mutations of DDR genes in mice and humans lead to a phenotype that is similar to obesity-related metabolic and cardiovascular dysfunctions.192 A higher frequency of DNA lesions including SSB, DSB, and oxidized bases was observed in lymphocytes derived from obese patients.193-195 It is now well accepted that chronic energy overload in obesity leads to elevated ROS generation and creates a chronic inflammatory condition.196 Production of pro-inflammatory adipokines as a result of excessive fat accumulation in adipocytes induces infiltration of T cells and macrophages.197 Accumulation of immune cells in adipose tissue triggers the production of ROS by NOX2, the NADPH oxidase produced in inflammatory cells. Smooth muscle cells and adipocytes exposed to excessive free fatty acids or hyperglycemia displayed enhanced mitochondrial ROS generation.198-200 Obesity-associated chronic inflammation was strongly correlated with the instigation of DNA damage.196 Activated macrophages release cytokines such as IL-6 and TNF-α which are capable of inducing DNA damage in nontargeting tissues remote from the inflammation site.201, 202 Translocation of cytokines to distinct tissues of the body triggers resident macrophages to release pro-inflammatory mediators including NO, NOS, COX2, superoxide, and ROS,203, 204 which all culminate in oxidative DNA damage. In young females, body mass index was inversely associated with NER capacity.205 Obesity was also reported to dysregulate DSB repair triggered by genotoxic factors.206 Studies have reported inhibition of DDR enzymes associated with oxidative stress in obesity.207, 208 Barouch et al. demonstrated that cardiomyocyte apoptosis was linked to enhanced DNA damage and reduced survival rate in obese mice.209
6.3 Myocardial ischemia-reperfusion injury (IRI)
Myocardial IRI is the most common consequence of ischemic heart disease which results in apoptosis and necrosis along with the transient decrease of contractility in surviving myocardial tissue.211 Shortly after total or partial coronary artery obstruction, ischemic myocardium utilizes anaerobic glycolysis as the main mechanism for generating ATP, leading to excessive production of intracellular H+.211, 212 When reperfusion and reoxygenation take place, the heart tissue will operate at a relatively inefficient rate due to the imbalance of electrolytes213 and the resultant myocardial dysfunction, microvascular injury, and arrhythmias.214-216 The most notable result of reperfusion is an ROS burst which is a main contributory factor to IRI. The ROS burst together with a variety of IRI-induced pathophysiological events that arise from intense mitochondrial redox conditions that exacerbate ROS generation. Overproduction of ROS activates oxidative DNA damage signaling and PARP1, leading to decreased intracellular ATP and NAD+.217, 218 NAD+ is a cosubstrate for sirtuin family proteins (SIRT1-7), all of which play a critical role in regulating redox homeostasis and are associated with CVDs.219, 220 Intracellular depletion of NAD+ attenuates the activity of SIRT1221 and SIRT3,222 further disturbing mitochondrial biogenesis and antioxidant defense, which leads to mitochondrial dysfunction, one of the hallmarks of IRI.223 Numerous investigations have confirmed the correlation between myocardial IRI and ROS-induced oxidative DNA damage.224 The production of 8-oxoG was directly related to the IRI severity in a study on rat hearts.225 In another study on rat myocardium, the level of 8-oxoG was gradually enhanced as a function of reperfusion time and was totally inhibited by means of an ROS scavenger.226 These findings validate the remarkable role of oxidative DNA damage in the development of myocardial IRI. Dysfunctional DDR proteins were also reported to negatively impact cell proliferation, apoptosis, and mitochondrial function, enhancing the risk of atherosclerosis, metabolic syndromes, and ischemic heart disease.161, 227 Collectively, although interventional strategies are essential for protecting the heart from ischemic injury, they can be inevitably entangled by IRI. Therefore, the lack of sufficient clinical data and inadequate pharmacodynamic and pharmacokinetic studies prompt a critical demand for efficient treatments for IRI in ischemic heart disease.
6.4 Heart failure and cardiac remodeling
Recent studies demonstrated the role of DNA damage in the setting of heart failure in rodent models95 and humans.230 In mice, cardiomyocyte-specific loss of BRCA1 or BRCA2 is shown to exacerbate myocardial infarction- and doxorubicin-induced accumulation of DNA damage, respectively, eventually leading to heart failure.85, 231 Studies have reported activation of DNA glycosylase toward 3-methyladenine and uracil in the infarcted and noninfarcted areas of the left ventricle in a rodent model of heart failure.232 Given the central role of DNA glycosylases in BER, these findings demonstrate an increase in deaminated and alkylated base lesions in heart failure. PARP1 deficiency in a murine model of aortic banding decreased translocation of apoptosis-inducing factors and myocardial hypertrophy.233 Studies have exhibited a role for BRCA1 and BRCA1-associated protein 2 (BRAP2) in an experimental model of right ventricular hypertrophy.234 Another study demonstrated that mechanical loading induced cardiac hypertrophy associated with overexpression of BRCA1.235 In another study, single nucleotide polymorphisms in BRAP2 were significantly associated with susceptibility to myocardial infarction.236 Higo et al. reported that DDR activation secondary to DNA SSBs increases the expression of pro-inflammatory cytokines via the NF-κB pathway in cardiomyocytes of the pressure overload-induced failing heart. Additionally, they showed that XRCC1 knockout mice had more severe heart failure, a phenomenon that was later restored by ATM deletion.95 In another study, Cao et al. identified a causal role for Ascc2 (activating signal cointegrator 1 complex subunit 2; an enzyme involved in DNA alkylation damage repair) in heart failure with preserved ejection fraction.237
7 TOWARD INTERVENTIONAL STRATEGIES IN CARDIOVASCULAR DYSFUNCTION CAUSED BY GENOMIC INSTABILITY
Given the significant contribution of DNA damage in the pathophysiology of CVDs, therapeutic strategies targeted toward genomic instability and DDR are proposed to lower CVDs-related morbidity and mortality. In general, such strategies can either inhibit the initiation of DNA damage or inactivate the DDR mechanisms in various disease stages (Figure 1).
7.1 Preventing DNA damage in cardiovascular diseases
7.1.1 Natural antioxidants
Preclinical and clinical studies have demonstrated that polyphenols such as resveratrol alleviate DNA damage in CVDs238 via activating antioxidant enzymes and scavenging ROS.239 Although therapeutically effective in preclinical investigations,240 randomized controlled trials of supplementary antioxidants such as vitamins C and E have not shown remarkable cardiovascular benefits in humans.241, 242 The inconsistency among these studies could be due to inadequate methodological design of trials, diverse baseline status of antioxidants, and lack of reliable oxidative stress biomarkers for clinical trials.
7.1.2 Statins
Statins exert their pharmacological effects via alleviation of DNA damage in CVDs such as atherosclerosis,243, 244 dyslipidemia,245, 246 myocardial infarction,247 and chemotherapy-induced cardiopathy.248 Statins decrease oxidative DNA damage and suppress DDR signaling. Statins can trigger phosphorylation of the ubiquitin ligase MDM2, leading to p53 degradation. Atorvastatin therapy inhibited ATM and ATR and decreased VSMC senescence and apoptosis in atherosclerosis.243 Statins can facilitate DDR through phosphorylation of human double minute protein Hdm2, resulting in Hdm2 dissociation from NBS-1 and inhibition of NBS-1 degradation. Additionally, statin therapy abrogates ionizing radiation-induced DDR including p53 and CHK1 activation in human endothelial cells.249
7.1.3 Angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin II receptor blockers (ARBs)
Elevated levels of angiotensin II cause oxidative stress in endothelial dysfunction and atherosclerosis.249 Ang II triggers oxidative DNA damage and accelerates vascular senescence via AT1 receptor in humans.250 ACEIs/ARBs exert cardiovascular protection by attenuating oxidative DNA damage.251, 252 The ARB losartan can decrease oxidative DNA damage and cellular senescence via inhibiting telomere-dependent replicative senescence, or telomere-independent stress-induced premature senescence.250 Oxidative DNA damage and myocardial infarction severity were decreased by valsartan and ramipril treatment in an experimental myocardial infarction model.253 Moreover, the administration of ARBs prevented oxidative DNA damage in hypertensive mice.254
7.1.4 β-blockers
Although little is known regarding the mechanism of β-adrenergic receptor blockade on DNA damage, experimental studies have shown that β-blockers exert cardiovascular protective effects by inhibiting DNA damage.256-258 Early administration of carvedilol-alleviated doxorubicin-induced DNA damage and cardiotoxicity.257 Carvedilol therapy also reduced levels of 8-oxoG and ameliorated heart failure in patients with dilated cardiomyopathy256 and reduced oxidative DNA damage in patients with hypertension.258
7.2 DNA damage response blockade: novel targets for the treatment of cardiovascular diseases
7.2.1 PARP inhibition
Accumulating evidence confirmed that PARP enzymes are aberrantly activated in CVDs,188, 259 and PARP inhibition is rendered therapeutically effective in preclinical and clinical investigations of CVDs.260, 261 INO-1001 reduced infarct size and improved cardiac function in myocardial IRI233, 262 and became the first PARP inhibitor to enter clinical trials.263 In this trial, PARP inhibition reduced postmyocardial infarction-associated inflammation via lowering plasma C-reactive protein and IL-6 levels. Pharmaceutical inhibition of PARP1 activity in mice with type 2 diabetes could remarkably improve vascular tone and function through NF-κB pathway regulation.264 In another independent study, INO-1001 inhibited pressure overload-induced reduction in cardiac contractility and prevented cardiac fibrosis, hypertrophy, and apoptosis in a murine model of heart failure.233
7.2.2 ATM inhibition
Genetic ablation of ATM and pharmacological inactivation by KU60019 improved cardiac function secondary to pressure overload.265 The lncRNA Caren preserved cardiac function during pressure overload by inhibition of ATM and activation of mitochondrial bioenergetics.91 In Caren loss-of-function mice, KU60019 could relatively rescue cardiac function. Although ATM inhibition has shown promising cardioprotective effects in heart failure, several studies have reported aberrant ATM activation in myocardial infarction.266-269 ATM deficiency attenuated postmyocardial infarction cardiac dysfunction, dilation, fibrosis, and increased apoptosis.266 Furthermore, ATM was shown to trigger cardiac inflammation during myocardial infarction.267 In ATM heterozygous knockout mice, cardiac remodeling was attenuated after myocardial infarction. KU60019 was recently shown to reduce infarct size and attenuate systolic dysfunction in myocardial infarction.269 While these studies hold promise of ATM inhibition in myocardial infarction, several investigations demonstrated that ATM deficiency aggravated postmyocardial infarction cardiac dysfunction and remodeling via disturbed autophagy and angiogenesis.270, 271 Based on these studies, ATM inhibition diminished cardiac inflammation, remodeling, and dysfunction 1–7 days postmyocardial infarction, whereas aggravating cardiomyocyte apoptosis, fibrosis, and cardiac hypertrophy was 14–28 days postmyocardial infarction.
7.2.3 ATR inhibition
Excessive ATR-p53 activation secondary to replication stress-induced DNA damage was reported in a model of Mybpc3−/− cardiomyopathy.272 Here, AZD6738 (a highly selective ATR inhibitor) was able to decrease cardiac remodeling and p53 depletion in cardiomyocytes imitated the cardioprotective function of AZD6738.
7.2.4 DNA-PK inhibition
DNA-PKs are aberrantly activated in various CVDs such as myocardial IRI,273 cardiac hypertrophy,265 atherosclerosis,93, 155, 274 and diabetic cardiomyopathy.275 Genetic and pharmacological inhibition of DNA-PKs showed favorable effects in atherosclerosis. The selective DNA-PK inhibitors DMNB and NU7024 could prevent NOR-1-dependent proliferation of aortic VSMCs in humans.274 Moreover, DNA-PK inhibition was shown to decrease neointimal lesion size following wire injury. DNA-PK was excessively activated in response to IRI-induced stress, and DNA-PK inhibition was reported to have protective effects.273 Interestingly, cardiomyocyte-specific DNA-PK depletion prevented inflammation and apoptosis and preserved cardiac function during IRI injury.
7.2.5 CHK1/2 inhibition
Several investigations have recently reported a role for CHK1/2 kinases in pulmonary artery hypertension273 and heart failure.274 Cardiomyocyte apoptosis is associated with CHK2 activation and telomere shortening.274 CHK1 was shown to be upregulated in distal pulmonary arteries and VSMCs of patients with pulmonary arterial hypertension.273, 275 CHK1 promoted VSMC resistance to apoptosis and proliferation. The CHK1 inhibitor MK8776, previously tested for clinical efficacy, improved hemodynamic parameters, and attenuated vascular remodeling in an experimental model of pulmonary artery hypertension,273 suggesting a therapeutic potential for CHK1 inhibitors in the management of pulmonary artery hypertension.
7.2.6 p53 inhibition
Several upstream kinases such as ATM, ATR, DNA-PK, CHK1, and CHK2279 regulate the phosphorylation and activation of p53. p53 activation was reported in a variety of CVDs such as cardiac remodeling, heart failure, diabetic cardiomyopathy, myocardial IRI, and chemotherapy-induced cardiotoxicity. Moreover, p53 plays a cardinal role in the pathogenesis of CVDs by mediating autophagy, apoptosis, angiogenesis, necrosis, senescence, and metabolic alterations. Genetic and pharmacological loss-of-function of p53 demonstrates beneficial effects on cardiovascular health.279 The therapeutic potential of p53 in CVDs is demonstrated in the mouse model, where deletion of one p53 allele is sufficient to protect the heart in cardiomyocyte-specific BRCA1 knockout mice.85 The p53 inhibitor pifithrin is currently utilized in preclinical models of CVDs to further assess its therapeutic efficacy.
8 FUTURE PERSPECTIVE
Inherited cancer syndrome is characterized by an increased risk of certain types of cancer that accounts for approximately 10% of all cancer cases.279 Inherited cancer syndromes are caused by heritable mutations in specific genes that lead to specific patterns of cancer such as early onset tumor development or developing more than one type of cancer in the same person.280, 281 Mutations of BRCA1 and/or BRCA2 result in HBOC that enhances the chance of developing breast, ovarian, prostate, pancreatic, and colon cancers.282 BRCA genes are inheritable in an autosomal-dominant manner and tend to be very penetrant. BRCA-associated tumors exhibit distinctive manifestations, clinical features, and pathologic profiles including younger patient age, advanced tumors, and aggressive nature. Current standard methods for experimental assessment of BRCA genes include comprehensive sequencing and examination of broad genomic rearrangements. Thorough knowledge of the molecular pathways involved in the initiation and progression of these malignancies will open a window on the behavior of these tumors and differential diagnosis of affected patients, supporting healthcare providers to make appropriate decisions regarding therapies. Recent investigations have revealed surprising similarities of molecular pathways involved in cancer and CVDs. Cumulative data suggest that DDR is activated in a variety of CVDs, indicating a close relation between CVDs and DNA damage or deficient DDR. Studies suggest that BRCA1 and BRCA2 mutation carriers show increased nonneoplastic mortality, especially at older ages.103, 104 While the causal factors of nonneoplastic death in these patients are still unidentified, the data presented in this review raise the likelihood that excess mortality can be mediated by enhanced rates of cardiovascular complications. From a pharmacological point of view, comprehensive knowledge of the DDR network will provide opportunities for the development of novel personalized therapeutics based on specific disease profiles. Furthermore, the knowledge that DDR is involved in both cancer and CVDs offers new opportunities to regulate oxidative DNA damage and target DDR pathways for the rational development of novel treatments.
AUTHOR CONTRIBUTIONS
KS and SN conceived and SN wrote the first draft of this review. SN made the figures. KS and SN revised and finalized the review.
FUNDING INFORMATION
This work was supported by a grant from the Canadian Institutes of Health Research to KS (grant/award no. FRN # 153216).
CONFLICT OF INTEREST
None.
ETHICS STATEMENT
Not applied.
CONSENT STATEMENT
Not applied.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




