Geographical disparities in human papillomavirus herd protection
Abstract
Background
Human papillomavirus (HPV) vaccination has occurred unequally across the United States, potentially contributing to uneven vaccine-type HPV prevalence between regions. We examined whether emerging vaccine-related herd protection exhibits regional differences among unvaccinated girls and women.
Methods
We evaluated the prevalence of vaginal HPV among women 14-59 years of age from 2003 to 2014 using repeated cross-sectional data from the National Health and Nutrition Examination Survey (NHANES). Women who provided an adequate vaginal swab sample were included. Vaginal prevalence of vaccine-type HPV (types 6, 11, 16, 18) were examined in four regions of the United States between 2003 and 2014. We examined vaccine-type HPV prevalence in 2007-2014 in each US census region among younger participants (14-34 years old) stratified by vaccination status to determine whether one or both groups contributed to uneven HPV prevalence.
Results
A total of 12 175 participants 14-59 years of age met inclusion criteria. Vaccine-type HPV prevalence decreased in all regions. Vaccine-type HPV varied by region only among unvaccinated 14-34 year olds, with a higher prevalence in the Midwest (13.8%, 95% confidence interval (CI): 10.7-17.0) and South (12.5%, 95% CI: 10.2-14.8) compared to the Northeast (8.9%, 95% CI: 6.5-11.2). No regional variation in vaccine-type HPV prevalence was observed among vaccinated participants.
Conclusions
Higher prevalence of vaccine-type HPV among unvaccinated women in the South and Midwest may contribute to regional disparities in HPV-related cancer incidence, as emerging herd immunity may not be as strong in those regions.
1 INTRODUCTION
Human papillomavirus (HPV) is a prevalent infection that causes genital warts and several cancers, including cervical and oropharyngeal cancer. The HPV vaccine series is expected to greatly reduce the morbidity and mortality caused by the virus. In fact, some nations with high HPV vaccine uptake are already reporting reductions in genital warts and abnormal cervical cancer screens.1, 2 Despite these benefits, the rate of adoption of the vaccine in the United States has been inadequate.3 The Advisory Committee for Immunization Practices recommends routine vaccination of adolescents at 11-12 years of age,4 but as of 2018, only 68% of 13-17 year olds had initiated the HPV vaccine series, and only 51% had completed it.5
National surveillance studies indicate that HPV vaccine initiation and completion rates among females are lower in the South and Midwest compared to other regions of the United States.3, 6, 7 This regional inequality among girls and women is a major concern because cervical cancer rates are higher in the South and in some Midwestern states.8 Continued low vaccination rates in these regions could further contribute to geographic disparities in HPV infection rates and HPV-related cancers.
Recently, regional variation in HPV prevalence following the launch of the HPV vaccine in the United States in 2006 was described, with a higher prevalence of vaccine-type HPV occurring in the South and Midwest than in the West and Northeast in post-licensure years according to data from the National Health and Nutrition Examination Survey (NHANES).9 Additionally, herd immunity is emerging in the US population. These studies demonstrated reduced HPV, genital wart, and precancerous cervical lesion prevalence among unvaccinated groups eligible to receive the vaccine in the United States.10-14 Age groups not eligible, or that may have already been exposed before catch-up vaccination could occur, did not exhibit similar decreases in HPV-related disease which indicates that HPV vaccination is likely responsible for the emerging herd immunity.10 Given these findings and prior reports of regional disparities in HPV vaccination, it is likely that emergent herd protection is also geographically heterogeneous. Therefore, we sought to examine variation in HPV prevalence among vaccinated and unvaccinated women in four regions of the United States during post-licensure years (2007-2014) and explore the distribution of herd protection among unvaccinated girls and women in each region using NHANES data.
2 MATERIALS AND METHODS
For this study, we utilized the NHANES dataset to conduct a secondary data analysis. NHANES consists of a series of nationally representative, cross-sectional surveys of the noninstitutionalized US population, conducted in two-year cycles by the US Centers for Disease Control and Prevention.15 Detailed methods have been previously described.16 Briefly, NHANES participants complete a household survey and undergo physical exams in a mobile examination center. Females 14-59 years of age were also asked to self-collect a vaginal swab for HPV testing. All NHANES swab samples were extracted and tested for types of HPV DNAusing Linear Array HPV genotypying assay (Roche Diagnostics). This data analysis, conducted using NHANES data, was exempted from review by the University of Texas Medical Branch Institutional Review Board. Restricted geographic variables were accessed through the Research Data Center at the National Center for Health Statistics.
The prevalence of HPV by region for six biennial cycles was determined between 2003 and 2014. Inclusion in this study required the following: (a) female, (b) 14-59 years of age, (c) adequate vaginal swab sample, (d) state of residence, and (e) self-reported HPV vaccination status for those participating 2007-2014. HPV results were grouped by type: any of 37 HPV types, vaccine-types (6, 11, 16, 18), and non-vaccine types (any HPV types except vaccine-types). Each HPV type group was transformed into a binary variable, with 0 = no type in the group detected and 1 = at least one type in the group detected.
Participants before the 2007-2008 cycle were considered unvaccinated, as the vaccine was approved for sale in mid-2006. Among those who responded to a question asking if they had received at least 1 dose of the HPV vaccine, the proportion of participants who responded “yes” was calculated. Demographics included race/ethnicity, marital status, and health insurance coverage. Behavioral characteristics included cigarette use, sexual behaviors, and alcohol and marijuana use in the past 12 months among 20-59 year olds. History of gonorrhea and chlamydia were based on self-report while history of herpes simplex type 2 (HSV2) was based on lab-confirmed testing and self-report.
The region of residence for participants in the NHANES dataset was defined by four US census regions, including the Northeast, Midwest, South, and West. Bivariate comparisons were conducted using Rao-Scott chi-square tests. For 2007-2008 through 2013-2014 cycles, analyses were restricted to participants who responded to whether they had received at least 1 HPV vaccine dose. After examining comparisons among 14-59 year olds, we grouped the sample into younger (14-34-year-old) and older (35-59-year-old) participants. We included older participants who would not have been eligible for HPV vaccination during the periods examined to determine whether observations were similar or different in both groups. We anticipated that women in the 35 - 59 year old group would not exhibit signs of herd immunity, as most would not have received HPV vaccine doses, and would therefore have different results than the younger age group. Percent change vaccine-type HPV prevalence between 2003-2004 and 2013-2014 cycles was calculated by subtracting 2003-2004 prevalence from 2013-2014 prevalence, and then dividing by prevalence of 2003-2004. Unadjusted logistic regression models were used to compare HPV population adjusted odds ratios (PaORs), which were weighted to produce national estimates as well as adjusted for the complex survey design. Each model was stratified by region. A multivariable logistic regression model was used to calculate adjusted PaORs (aPaORs) for vaccine-type HPV during post-licensure cycles, after adjusting for demographics and HPV risk factors. MEC weights were used to account for nonresponse and complex survey methods.17 Analyses on the NHANES dataset were conducted using SAS statistical software version 9.4 (SAS Institute, Inc).
3 RESULTS
A total of 14 033 females 14-59 years of age participated across the 6 cycles of NHANES sampling from 2003 to 2014. Of these, 12 182 (86.8%) had valid HPV genotyping results.7 After excluding 7 participants without known region of residence, 12 175 participants were eligible for final analyses. For post-vaccine licensure cycles (2007-2014), 8025 girls and women 14- 59 years old reported their HPV vaccination status.
There were regional differences in several demographic characteristics, including age group, race/ethnicity, and health insurance coverage (Table 1). Regional differences were also observed in behavioral characteristics including cigarette use, sexual activity, number of lifetime partners, vaginal sexual activity, and oral sexual activity. The prevalence of HSV2 also varied by region.
| Frequency (n, w%) | P-value* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall (N = 12,175) | Northeasta (n = 1947) | Midwesta (n = 2394) | Southa (n = 4688) | Westa (n = 3146) | ||||||||
| NHANES cycle | ||||||||||||
| 2003-2006 | 3929 (32.0) | 584 (30.4) | 808 (32.2) | 1538 (32.3) | 999 (32.7) | .96 | ||||||
| 2007-2010 | 4114 (33.1) | 647 (33.7) | 912 (36.8) | 1544 (32.3) | 1011 (30.1) | |||||||
| 2011-2014 | 4132 (34.9) | 716 (35.9) | 674 (31.0) | 1606 (35.4) | 1136 (37.2) | |||||||
| Age (y), mean | ||||||||||||
| 14-34 | 6201 (42.3) | 908 (39.3) | 1210 (40.5) | 2410 (42.8) | 1673 (45.7) | .02 | ||||||
| 35-59 | 5974 (57.7) | 1039 (60.7) | 1184 (59.5) | 2278 (57.2) | 1473 (54.3) | |||||||
| Race | ||||||||||||
| Hispanic | 3413 (15.0) | 431 (11.6) | 290 (4.9) | 1215 (16.3) | 1477 (25.4) | <.0001 | ||||||
| Non-hispanic white | 4804 (65.1) | 877 (71.9) | 1433 (80.8) | 1501 (56.1) | 993 (58.5) | |||||||
| Non-hispanic black | 2903 (13.2) | 431 (10.5) | 527 (9.7) | 1687 (22.1) | 258 (4.9) | |||||||
| Other | 1055 (6.7) | 208 (6.0) | 144 (4.6) | 285 (5.5) | 418 (11.2) | |||||||
| Health insurance coverage | ||||||||||||
| Private/Public | 9103 (80.0) | 1628 (87.3) | 1940 (85.5) | 3284 (74.9) | 2251 (77.1) | <.0001 | ||||||
| Uninsured | 3038 (20.0) | 313 (12.7) | 450 (14.5) | 1390 (25.1) | 885 (22.9) | |||||||
| Missing = 34 | ||||||||||||
| Marital status | ||||||||||||
| Never married | 5872 (61.3) | 939 (61.7) | 1193 (63.8) | 2167 (59.7) | 1573 (60.9) | .32 | ||||||
| Married/Living together | 1769 (16.1) | 283 (15.5) | 345 (14.2) | 700 (16.8) | 441 (17.3) | |||||||
| Widowed/divorced/separated | 3256 (22.6) | 534 (22.8) | 624 (22.0) | 1327 (23.5) | 771 (21.8) | |||||||
| Missing = 1278 | ||||||||||||
| Cigarette use | ||||||||||||
| Never | 7436 (59.7) | 1117 (56.0) | 1285 (10.2) | 2971 (20.4) | 2063 (64.1) | <.0001 | ||||||
| Former | 2138 (21.9) | 372 (21.7) | 466 (19.8) | 749 (15.9) | 551 (18.2) | |||||||
| Current | 2422 (18.4) | 428 (22.3) | 618 (25.9) | 893 (21.9) | 483 (17.7) | |||||||
| Missing = 179 | ||||||||||||
| Alcohol use in 12 mo, average number of drinks per week (≥20 yo) | ||||||||||||
| 0 | 3618 (33.8) | 517 (28.0) | 600 (27.5) | 1558 (40.0) | 943 (35.2) | <.0001 | ||||||
| ≥1 | 5245 (66.2) | 920 (72.0) | 1193 (72.5) | 1835 (60.0) | 1297 (64.8) | |||||||
| Missing = 899 | ||||||||||||
| Marijuana usec | ||||||||||||
| Never | 4854 (47.1) | 724 (41.5) | 827 (43.7) | 1972 (52.8) | 1331 (46.0) | <.0001 | ||||||
| Former | 3122 (42.7) | 518 (48.6) | 700 (46.3) | 1103 (38.4) | 801 (41.4) | |||||||
| Current | 951 (10.2) | 173 (9.9) | 203 (10.0) | 320 (8.8) | 255 (12.6) | |||||||
| Missing = 1228 | ||||||||||||
| Ever had sex (any sex) | ||||||||||||
| No | 1235 (7.4) | 179 (6.8) | 205 (6.8) | 451 (7.1) | 400 (8.8) | .05 | ||||||
| Yes | 9793 (92.6) | 1553 (93.2) | 2003 (93.2) | 3793 (92.9) | 2444 (91.2) | |||||||
| Missing = 1147 | ||||||||||||
| Number of lifetime sex partners (any sex) (include only have ever sex) | ||||||||||||
| 0 | 51 (0.4) | 10 (0.6) | 5 (0.3) | 21 (0.5) | 15 (0.4) | .02 | ||||||
| 1-2 | 2959 (27.3) | 394 (23.6) | 551 (26.5) | 1084 (27.2) | 930 (30.9) | |||||||
| ≥3 | 6581 (72.3) | 1105 (75.8) | 1404 (73.2) | 2612 (72.3) | 1460 (68.7) | |||||||
| Missing = 207 | ||||||||||||
| Number of vaginal sex partners in past 12 mod | ||||||||||||
| 0 | 685 (14.6) | 112 (14.8) | 120 (13.9) | 264 (13.8) | 189 (16.2) | .37 | ||||||
| 1 | 3214 (70.1) | 543 (72.4) | 645 (68.9) | 1185 (69.5) | 841 (70.7) | |||||||
| ≥2 | 791 (15.3) | 119 (12.8) | 164 (17.2) | 333 (16.7) | 175 (13.1) | |||||||
| Missing = 230 | ||||||||||||
| HPV vaccine (≥1 dose)b | ||||||||||||
| Yes | 1015 (11.2) | 208 (13.1) | 185 (10.0) | 351 (10.7) | 271 (11.7) | .28 | ||||||
| No | 7010 (88.8) | 1114 (86.9) | 1379 (90.0) | 2719 (89.3) | 1798 (88.3) | |||||||
| Missing = 224 | ||||||||||||
| HPV vaccine dose number, n = 1015 (only for vaccinated women) | ||||||||||||
| 1 dose | 187 (15.8) | 28 (10.4) | 29 (12.8) | 77 (18.1) | 53 (19.8) | .22 | ||||||
| 2 dose | 197 (19.9) | 43 (19.6) | 32 (21.1) | 60 (16.3) | 62 (24.0) | |||||||
| 3 dose | 587 (64.3) | 127 (70.0) | 117 (66.0) | 195 (65.6) | 148 (56.2) | |||||||
| Missing = 44 (excluded from 03-04 data, and need to consider only for vaccinated women) | ||||||||||||
| Gonorrhea or chlamydia (self-reported) | ||||||||||||
| Positive | 448 (2.7) | 55 (1.9) | 88 (2.8) | 214 (3.0) | 91 (2.7) | .19 | ||||||
| Negative | 10 205 (97.3) | 1603 (98.1) | 2073 (97.2) | 3931 (97.0) | 2598 (97.3) | |||||||
| Missing = 1522 | ||||||||||||
| Herpes simplex virus type 2 (lab tested, then self-reported) | ||||||||||||
| Positive | 1390 (12.4) | 217 (11.0) | 240 (9.7) | 640 (14.9) | 293 (12.3) | .0008 | ||||||
| Negative | 9755 (87.6) | 1551 (89.0) | 1997 (90.3) | 3628 (85.1) | 2579 (87.7) | |||||||
| Missing = 1030 | ||||||||||||
- Bolded values indicate significance at P < .05.
- Abbreviation: w%, weighted percent.
- a Northeast states = Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont; Midwest states = Indiana, Illinois, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin; South states = Arkansas, Alabama, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, +Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia; West states = Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming.
- b Data on HPV vaccination were included in survey years 2007-2014 for females.
- c Marijuana data available from 20-59 yo in 2003-2006 cycle and 14-59 yo in 2007-2014 cycle. Current marijuana use was defined as ≥1 use within the past 30 d.
- d Lifetime and recent number of vaginal sex partners included same- and opposite-sex partners.
- * Rao-Scott Chi-Square test comparing Northeast, Midwest, South, and West.
Prevalence of any HPV type remained stable across time and had similar rates among 14-59-year-old participants in the Northeast, Midwest, and South after the 2005-2006 cycle (Figure 1A). Between the 2003-2004 and the 2013-2014 cycles, vaccine-type HPV prevalence decreased by 65% in the Northeast, 48.7% in the Midwest, 27.2% in the South, and 37% in the West (Figure 1B).
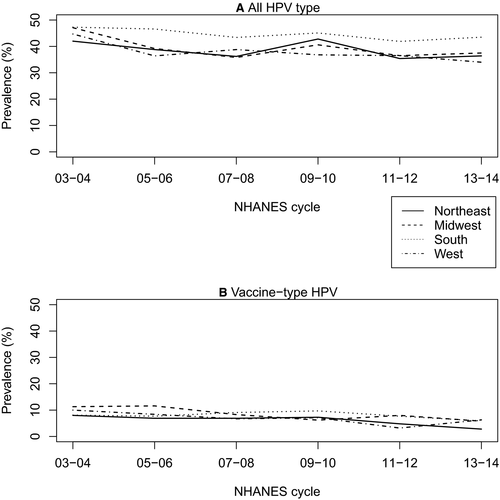
Among 14-59-year-old participants in the post-vaccine licensure cycles, we found significant regional differences in the prevalence of non-vaccine-type HPV (Table 2). However, after stratifying by vaccination status, there were significant regional differences in HPV prevalence among unvaccinated participants only. Regional differences among the unvaccinated were observed for the prevalence of any type, vaccine type, and non-vaccine type HPV. No regional differences were observed among vaccinated participants in the post-licensure cycles.
| Prevalence (w%, 95% CI) | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 8025) | Northeasta (n = 1322) | Midwesta (n = 1564) | Southa (n = 3070) | Westa (n = 2069) | P * | |
| Entire sample | ||||||
| Any HPV typesb | 39.6 (33.6, 45.6) | 37.8 (34.1, 41.4) | 38.1 (36.9, 39.2) | 43.3 (27.6, 59.0) | 36.7 (30.6, 42.8) | .06 |
| Vaccine-type (6, 11, 16, 18) | 6.8 (5.8,7.9) | 5.4 (2.8, 7.9) | 7.1 (4.2, 10.1) | 8.1 (5.4, 10.7) | 5.8 (0.2, 11.4) | .18 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 37.9 (31.3, 44.4) | 36.8 (33.0, 40.7) | 36.0 (35.0. 37.1) | 41.4 (26.8, 56.0) | 35.1 (32.9, 37.3) | .01 |
| Vaccinated | ||||||
| Any HPV typesb | 48.7 (44.2, 53.2) | 54.5 (45.4, 63.6) | 51.1 (43.6, 58.7) | 48.5 (39.8, 57.3) | 42.1 (34.4, 49.8) | .21 |
| Vaccine-type (6, 11, 16, 18) | 4.9 (3.2, 6.5) | 4.5 (0.8, 8.3) | 5.9 (1.6, 10.2) | 5.8 (2.6, 9.0) | 2.9 (0.8, 5.0) | .54 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 47.9 (43.4, 52.5) | 54.5 (45.4, 63.6) | 48.2 (39.5, 57.0) | 48.1 (39.4, 56.8) | 41.9 (33.9, 49.8) | .27 |
| Unvaccinated | ||||||
| Any HPV typesb | 38.4 (36.7, 40.2) | 35.3 (31.7, 38.8) | 36.6 (33.6, 39.7) | 42.7 (39.9, 45.5) | 36.0 (32.3, 39.7) | .001 |
| Vaccine-type (6, 11, 16, 18) | 7.1 (6.3, 7.9) | 5.5 (4.3, 6.7) | 7.3 (5.9, 8.7) | 8.3 (7.0, 9.7) | 6.2 (4.5, 7.8) | .02 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 36.6 (35.0, 38.3) | 34.2 (30.6, 37.8) | 34.7 (31.6, 37.8) | 40.6 (37.9, 43.4) | 34.2 (30.8, 37.6) | .002 |
| PaOR (95% CI) unvaccinated vs vaccinated | ||||||
| Any HPV typesb | 0.46 (0.36, 0.58) | 0.55 (0.44, 0.70) | 0.79 (0.56,1.12) | 0.77 (0.55,1.09) | ||
| Vaccine-type (6, 11, 16, 18) | 1.23 (0.52, 2.89) | 1.25 (0.76, 2.05) | 1.48 (0.78, 2.81) | 2.20 (1.28, 3.76) | ||
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 0.43 (0.34, 0.55) | 0.57 (0.45, 0.72) | 0.74 (0.52, 1.06) | 0.72 (0.51, 1.03) | ||
- Bolded values indicate significance at P < .05.
- Abbreviations: 95% CI, 95% confidence interval; PaOR, population adjusted odds ratio unadjusted for potential confounders; w%, weighted percent.
- a Northeast states = Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont; Midwest states = Indiana, Illinois, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin; South states = Arkansas, Alabama, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia; West states = Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming.
- b HPV types: 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, and IS39.
- * Rao-Scott chi-Square test comparing Northwest, Midwest, South, and West.
To determine whether emerging herd immunity is apparent, we examined the prevalence of HPV between vaccinated and unvaccinated women by region. Among 14-34 year olds in post-licensure cycles, we observed regional differences in the prevalence of vaccine-type HPV, but not the other groupings of HPV types (Table 3). HPV vaccination among the 14-34 year olds increased from 10.9% in 2007-2008 to 34.9% in 2013-2014, with the greatest increase occurring in the Northeast. However, the vaccination rate within each cycle and in all cycles combined did not vary by US region (Table S2). Conversely, among women 35-59 years of age, of whom only 1.55% have received the HPV vaccine during 2007-2014, we observed regional differences for any type, for high-risk type, for high-risk non-vaccine type, and non-vaccine type HPV in the post-licensure cycles (Table S1).
| Prevalence (w%, 95% CI) | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 3709) | Northeasta (n = 566) | Midwesta (n = 718) | Southa (n = 1435) | Westa (n = 990) | P * | |
| Combined years | ||||||
| Any HPV typesb | 44.7 (42.4, 47.0) | 45.1 (39.6, 50.6) | 45.5 (40.3, 50.8) | 47.3 (43.9, 50.7) | 40.1 (35.6, 44.6) | .10 |
| Vaccine-type (6, 11, 16, 18) | 9.4 (8.4, 10.5) | 7.4 (5.1, 9.7) | 11.5 (9.1, 13.9) | 10.7 (8.7, 12.8) | 7.0 (5.0, 9.1) | .01 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 43.2 (40.8, 45.6) | 44.5 (38.7, 50.3) | 43.5 (38.3, 48.7) | 45.4 (41.8, 49.0) | 38.9 (34.4, 43.4) | .16 |
| Vaccinated group | ||||||
| Any HPV typesb | 49.0 (44.1, 54.0) | 55.7 (45.7, 65.6) | 49.2 (41.0, 57.5) | 48.5 (39.3, 57.7) | 43.6 (34.3, 52.9) | .36 |
| Vaccine-type (6, 11, 16, 18) | 4.2 (2.8, 5.6) | 4.2 (0.9, 7.4) | 4.2 (1.3, 7.0) | 4.9 (2.0, 7.9) | 3.1 (0.7, 5.4) | .81 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 48.6 (43.7, 53.6) | 55.7 (45.7, 65.6) | 48.3 (40.0, 56.6) | 48.2 (39.1, 57.4) | 43.3 (33.8, 52.9) | .35 |
| Unvaccinated group | ||||||
| Any HPV typesb | 43.3 (40.8, 45.8) | 40.2 (33.7, 46.7) | 44.4 (38.7, 50.0) | 46.9 (43.1, 50.7) | 39.1 (34.0, 44.2) | .08 |
| Vaccine-type (6, 11, 16, 18) | 11.1 (9.8, 12.4) | 8.9 (6.5, 11.2) | 13.8 (10.7, 17.0) | 12.5 (10.2, 14.8) | 8.2 (5.6, 10.8) | .01 |
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 41.4 (38.9, 44.0) | 39.3 (32.5, 46.2) | 42.0 (36.3, 47.7) | 44.6 (40.4, 48.7) | 37.6 (32.5, 42.8) | .20 |
| PaOR (95% CI) unvaccinated vs vaccinated | ||||||
| Any HPV typesb | 0.54 (0.38, 0.75) | 0.82 (0.66, 1.03) | 0.94 (0.63, 1.39) | 0.83 (0.55, 1.26) | ||
| Vaccine-type (6, 11, 16, 18) | 2.24 (1.21, 4.14) | 3.70 (1.21, 4.14) | 2.74 (1.35, 5.56) | 2.82 (1.49, 5.34) | ||
| Nonvaccine-type (any type other than 6, 11, 16, 18) | 0.52 (0.37, 0.73) | 0.78 (0.61, 0.98) | 0.86 (0.57, 1.30) | 0.79 (0.51, 1.21) | ||
- Bolded values indicate significance at P < .05.
- Abbreviations: 95% CI, 95% confidence interval; PaOR, population adjusted odds ratio unadjusted for potential confounders; w%, weighted percent.
- a Northeast states = Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont; Midwest states = Indiana, Illinois, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin; South states = Arkansas, Alabama, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia; Weststates = Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Washington, Wyoming.
- b HPV types: 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, and IS39.
- * Rao-Scott chi-Square test comparing Northeast, Midwest, South, and West.
We next sought to determine if emerging herd protection, indicated by declines in vaccine-type HPV prevalence among the unvaccinated, varies across the United States. We found no regional differences in HPV prevalence for any grouping of HPV types among vaccinated 14-34-year-old participants (Table 3). Among unvaccinated 14-34 year olds, however, we observed regional variations in vaccine-type HPV, which was significantly higher among unvaccinated young women compared to vaccinated young women in every region. Among Northeastern participants, those who were unvaccinated had lower prevalence rates of any type HPV compared to those who were vaccinated.
To determine whether these findings were the result of confounding factors, we used multivariable models to calculate aPaORs for demographics and behavioral characteristics among unvaccinated 14- to 34-year-old women. Vaccine-type HPV prevalence in unvaccinated participants was lower in the late vaccination periods (2011-2012 and 2013-2014) compared to the early period (2007-2008; Table 4). In a model that included only region and number of lifetime same sex partners, we found that the time effects were magnified compared to the model adjusted with other confounders. (Table S2).
| Variable | aPaOR (95% CI) |
|---|---|
| NHANES cycle | |
| 2007-2008 | Reference |
| 2009-2010 | 0.93 (0.66, 1.32) |
| 2011-2012 | 0.59 (0.37, 0.94) |
| 2013-2014 | 0.53 (0.34, 0.83) |
| Race | |
| Hispanic | Reference |
| Non-hispanic white | 1.01 (0.64, 1.60) |
| Non-hispanic black | 1.02 (0.58, 1.79) |
| Others | 1.64 (0.88, 3.04) |
| Insurance status | |
| None | Reference |
| Has insurance | 0.64 (0.44, 0.94) |
| Marital status | |
| Never married | Reference |
| Married/living with partner | 0.36 (0.24, 0.53) |
| Widowed/divorced/separated | 0.85 (0.51, 1.41) |
| Cigarette use | |
| Never | Reference |
| Former | 1.08 (0.56, 2.08) |
| Current | 1.74 (1.15, 2.62) |
| Alcohol use in 12 mo, average number of drinks per week (≥20 yo) | |
| 0 | Reference |
| ≥1 | 1.21 (0.80, 1.83) |
| Marijuana use status | |
| Never | Reference |
| Former | 1.56 (1.05, 2.33) |
| Current | 1.28 (0.74, 2.24) |
| Gonorrhea or chlamydia (self-reported) | |
| Negative | Reference |
| Positive | 3.11 (1.77, 5.49) |
| Herpes simplex virus type 2 (tested and self-reported) | |
| Negative | Reference |
| Positive | 0.84 (0.52, 1.38) |
Note
- Bolded values indicate significance at P < .05.
- Abbreviations: 95% CI, 95% confidence interval; aPaOR, population adjusted odds ratio, adjusted for potential confounding factors as listed in the table.
4 DISCUSSION
Human papillomavirus vaccination has been shown to vary across the United States, with the lowest HPV vaccination rates occurring in the South.7, 18 This study confirms that geographic disparities in HPV vaccination may be problematic, as there were significant geographic differences in vaccine-type HPV prevalence among unvaccinated women. Regions with lower vaccination rates had the highest prevalence of vaccine-type HPV among 14- to 34-year-old unvaccinated women compared to vaccinated women. Similar findings have been reported in a Switzerland-based modeling study, in which higher HPV type 16 prevalence was associated with regions of lower vaccine uptake.19 While this effect may be somewhat mitigated by sexual activity occurring between occupants in different regions of a geographically small nation such as Switzerland, in the larger United States, the majority of residents tend to remain within a single census region. Moves between regions are relatively rare, particularly among populations from lower socioeconomic status groups.20 Thus, uneven vaccination rates could contribute to continuing geographic disparities in HPV-related cancers.21-23
Our study adds further evidence that herd immunity is emerging among unvaccinated women. A reduction in vaccine-type HPV prevalence was seen among unvaccinated young women across time in the post-licensure years, even after controlling for several factors associated with HPV acquisition and persistence. Our findings fit with several prior studies identifying a decrease in HPV prevalence among unvaccinated people in the United States and other countries including Australia and Scotland.24-26 Although herd immunity in the United States has previously been reported, regional variations were not.14 Understanding emerging herd immunity effects at the regional or even local level is important as seemingly strong protection at the national level may belie vulnerability in populations experiencing weaker protection. Recently, clustered outbreaks of measles and pertussis in localized areas with low vaccination rates have caused concerns about how they contribute to perpetuation of these diseases.27-30 It may take more than a decade for the consequences of disparities in HPV immunity to become apparent due to the slow progression from HPV infection to cancer. Nonetheless, the risk of higher regional HPV-related cancer morbidity and mortality warrants greater attention to regional disparities in HPV prevalence, particularly for regions already presenting with greater incidence of HPV-related cancers.
The primary strength of this study is that it used repeated cross-sectional survey data representative of the United States. However, these data also create limitation as they may not be representative of each region. Moreover data on HPV vaccination in NHANES are collected by self-report, which is subject to recall bias. Furthermore, accuracy of adolescent HPV vaccination reports have been found to vary by race/ethnicity, and could potentially vary by region, which could introduce bias within and between regions.31 It is possible that lower vaccine-type HPV in Northeast and West regions may not be due to herd protection related to higher HPV vaccination rates, but rather due to overall lower circulation of HPV in those regions as a result of differing risk behaviors or other factors.
In summary, this study sheds light on the origin of recently reported regional variation in HPV prevalence in the United States. Only among unvaccinated girls and women did vaccine-type HPV prevalence vary by region. Notably, odds of vaccine-type HPV prevalence were higher among unvaccinated young women in the Midwest and South where vaccination rates are not increasing as quickly as in the Northeast. Given the higher prevalence of HPV in the South and Midwest, interventions are needed to increase vaccination rates and to maintain or improve cervical cancer screening in these areas.
ACKNOWLEDGMENTS
Data files were created by Karon C. Lewis at the National Center for Health Statistics Research Data Center.
CONFLICTS OF INTEREST
The authors declare no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
ABB contributed to conceptualization, funding acquisition, project administration, resources, visualization, writing-original draft, and writing-review and editing. JMH contributed to conceptualization, formal analysis, methodology, project administration, supervision, writing-original draft, and writing-review and editing. MC contributed to conceptualization, formal analysis, methodology, project administration, writing-original draft, and writing-review and editing.
PRECIS
Uneven HPV vaccination across the United States may be contributing to continued geographic disparities in HPV-related cancers among unvaccinated young women, as emerging herd immunity may not be as strong in regions with lower vaccination rates.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the Centers for Disease Control and Prevention. Restrictions apply to the availability of these data, which were used under license for this study. Limited data sets are available at https://www.cdc.gov/nchs/nhanes/index.htm. Access to restricted use data is possible with the permission of the National Center for Health Statistics.