Acute hemolytic anemia after hematopoietic stem cell transplantation: An unusual invader
Graphical Abstract
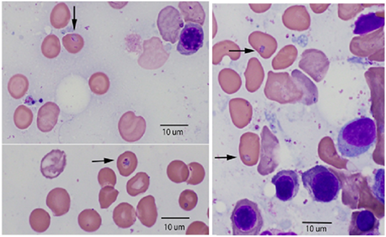
69-year-old man with a history of diffuse large B-cell lymphoma (DLBCL) presented with severe acute hemolytic anemia 27 months after an autologous hematopoietic stem cell transplantation. Bone marrow aspirate revealed intracellular micro-organisms (arrows) located within the cytoplasm of red blood cells confirming the diagnosis of severe babesiosis.
A 69-year-old man with a history of diffuse large B-cell lymphoma (DLBCL) presented to our clinic with extreme fatigue and severe hemolytic anemia, 27 months after an autologous hematopoietic stem cell transplantation (HSCT).
The patient history began 6 years prior to this presentation. He was initially diagnosed with DLBCL and treated with 6 cycles of rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone (R-CHOP). He achieved complete remission (CR) for 3 years before he relapsed. He was treated with 2 cycles of dexamethasone, ifosfamide, cisplatin, and etoposide and achieved CR again. He was then conditioned with rituximab, carmustine, BCNU, etoposide, cytarabine, and melphalan and underwent autologous HSCT achieving CR. Twenty-seven months after the transplant, he presented to our clinic with progressive fatigue, shortness of breath, and fever. Blood tests showed severe normocytic anemia with hemoglobin of 6.7 g/dL (normal 13.7–17.5), platelet count of 76 × 103 per uL (normal 150–450), white blood cells of 3.2 × 103 per uL (normal 3.4–11.2) with an absolute lymphocyte count of 0.7 × 103 per uL (normal 1.18–3.74). Hemolysis workup revealed elevated lactate dehydrogenase to 1019 U/L (normal 118–230), haptoglobin level of 25 mg/dL (normal 40–240), absolute reticulocyte count of 185.3 × 103 per uL (normal 18.8–108.6) with negative direct antiglobulin test. A bone marrow biopsy was done to further investigate the cause of hemolytic anemia. Bone marrow aspirate showed intra-erythrocytic parasite forms consistent with Babesia microti (Figure 1), with a parasitic burden of 6.2% in peripheral blood. The polymerase chain reaction (PCR) for Babesia microti was positive. Buffy coat smear for Anaplasma and Ehrlichia was negative. Due to severe hemolysis, the patient was admitted and treated with whole-blood red cell exchange transfusion which dropped his parasitemia to 1.3%. He was started on azithromycin 1 g daily and atovaquone 750 mg twice daily. One week after admission, the fever abated, and his symptoms improved. He was discharged with continued monitoring of hemolysis labs, the parasite blood smear, and Babesia microti PCR on a weekly basis. His blood smear and hemolysis labs remained positive for three months. The PCR turned negative after 5 months of treatment. Azithromycin and atovaquone were discontinued after confirming 2 consecutive negative PCRs.
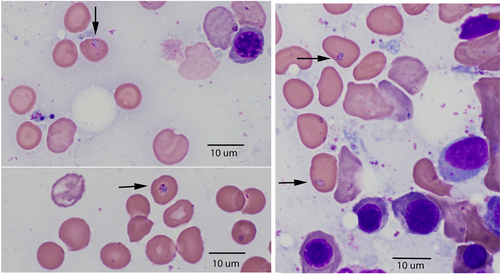
Babesiosis is transmitted by hard-bodied tick vectors (Ixodes spp.), and by blood transfusion.1 By 2019, U.S. Food and Drug Administration recommended regional molecular screening of blood donors utilizing approved assays in 15 identifies Babesia-risk states.2 The patient in this case confirmed a history of tick bites while he was taking many walks in heavily wooded areas known to be harboring ticks 5 weeks before his symptoms appeared. Rarely, babesiosis can complicate the course of HSCT recipients especially in asplenic patients or with patients who received B-cells depletion with anti-CD20 antibodies.3 The most common hematological manifestations include thrombocytopenia, immune, and non-immune hemolytic anemia, and lymphopenia.4 The diagnosis is usually established by the identification of the organisms on a thin blood smear. Identifying Babesia organisms in the bone marrow as demonstrated in our case is rarely reported and it may be associated with severe disease and high parasitic burden. While the disease is manageable in an immunocompetent host, the course in immunocompromised patients can be severe, and require a prolonged treatment course, with a mortality rate reaching up to 20%.1 Early recognition is essential to avoid lethal complications.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data used and/or analyzed during this submission are original and they are available from corresponding author on reasonable request.