Severe delayed graft function in a living-related kidney transplant recipient due to combination of alloimmunity, autoimmunity, and heterologous immunity: A case report
Corresponding Author
Rabab Ali Al Attas
Histocompatibility and Immunogenetic Laboratory (HIL), Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital- Dammam, Dammam, Saudi Arabia
Correspondence
Rabab Ali Al Attas, Department of Pathology and Lab Medicine, King Fahad Specialist Hospital-Dammam (KFSH-D), Al Muraikibat, Amer Bin Thabit St., Building 6, Office 2, PO.BOX:15215, Dammam 31444, Saudi Arabia.
Email: [email protected]
Search for more papers by this authorAlanoud Alshami
Division of Pediatric Nephrology and Kidney Transplant, Liver Transplant Multiorgan Transplant Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorNasreen Mohamed
Division of Anatomic Pathology, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorZuhoor Qahtani
Histocompatibility and Immunogenetic Laboratory (HIL), Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital- Dammam, Dammam, Saudi Arabia
Search for more papers by this authorRafah Bamardouf
Histocompatibility and Immunogenetic Lab, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorSaber Alzahrani
Histocompatibility and Immunogenetic Lab, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorCorresponding Author
Rabab Ali Al Attas
Histocompatibility and Immunogenetic Laboratory (HIL), Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital- Dammam, Dammam, Saudi Arabia
Correspondence
Rabab Ali Al Attas, Department of Pathology and Lab Medicine, King Fahad Specialist Hospital-Dammam (KFSH-D), Al Muraikibat, Amer Bin Thabit St., Building 6, Office 2, PO.BOX:15215, Dammam 31444, Saudi Arabia.
Email: [email protected]
Search for more papers by this authorAlanoud Alshami
Division of Pediatric Nephrology and Kidney Transplant, Liver Transplant Multiorgan Transplant Center, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorNasreen Mohamed
Division of Anatomic Pathology, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorZuhoor Qahtani
Histocompatibility and Immunogenetic Laboratory (HIL), Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital- Dammam, Dammam, Saudi Arabia
Search for more papers by this authorRafah Bamardouf
Histocompatibility and Immunogenetic Lab, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorSaber Alzahrani
Histocompatibility and Immunogenetic Lab, Department of Pathology and Laboratory Medicine, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Search for more papers by this authorAbstract
Background
Delayed graft function is a manifestation of acute kidney injury unique to transplantation usually related to donor ischemia or recipient immunological causes. Ischemia also considered the most important trigger for innate immunity activation and production of non-HLA antibodies. While ischemia is inevitable after deceased donor transplantation, this complication is rare after living transplantation. Heterologous Immunity commonly used to describe the activation of T cells recognizing specific pathogen-related antigens as well unrelated antigens is common post-viral infection. In transplant-setting induction of heterologous immunity that cross-react with HLA-antigens and subsequent reactivation of memory T cells can lead to allograft rejection.
Methods
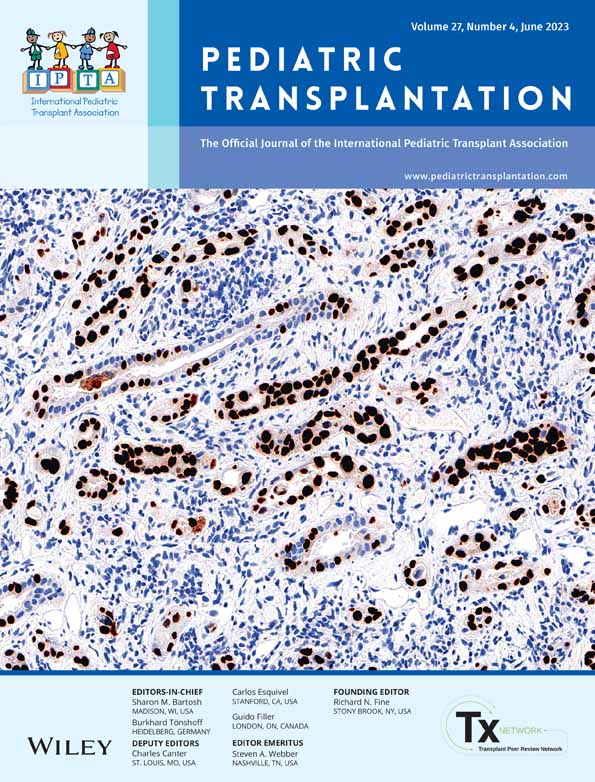
Here we describe a non-sensitized child with ESRD secondary to lupus nephritis and recent history of COVID-19 infection who experienced 17 days of anuria after first kidney living transplantation from her young HLA-haploidentical uncle donor. Graft histology showed acute cellular rejection, evidence of mild antibody-mediated rejection and vascular wall necrosis in some arterioles suggesting possibility of intraoperative graft ischemia. Both pre- and post-transplant sera showed very high level of several non-HLA antibodies.
Results
The patient was treated for cellular and antibody-mediated rejection while maintained on hemodialysis before her graft function started to improve on day seventeen post transplantation.
Conclusion
The cellular rejection likely trigged by ischemia that activated T-cells-mediated immunity. The high level of non- HLA-antibodies further aggravated the damage and the rapid onset of rejection may be partly related to memory T-cell activation induced by heterologous immunity.
CONFLICT OF INTEREST
The authors confirm that there are no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
Supporting Information
| Filename | Description |
|---|---|
| petr14424-sup-0001-AppendixS1.zipZip archive, 857.6 KB |
Appendix S1 |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Eltzschig HK, Eckle T. Ischemia and reperfusion–from mechanism to translation. Nat Med. 2011; 17: 1391-1401.
- 2Salvadori M, Rosso G, Bertoni E. Update on ischemia-reperfusion injury in kidney transplantation: pathogenesis and treatment. World J Transplant. 2015; 5: 52-67.
- 3Park HS, Hong YA, Kim HG, et al. Delayed graft function in living-donor renal transplantation: 10-year experience. Transplant Proc. 2012; 44: 43-46.
- 4Mallon D, Summers D, Bradley J, Pettigrew G. Defining delayed graft function after renal transplantation: simplest is best. Transplantation. 2013; 96(10): 885-889.
- 5Grenda R. Delayed graft function and its management in children. Pediatr Nephrol. 2017; 32: 1157-1167.
- 6Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011; 11: 2279-2296.
- 7Halloran PF, Hunsicker LG. Delayed graft function: state of the art. Summit meeting, Scottsdale, Arizona. Am J Transplant. 2001; 1: 115-120.
- 8Van Arendonk K, Boyarsky B, Orandi BJ, et al. National trends over 25 years in pediatric kidney transplant outcomes. Pediatrics. 2014; 133(4): 594-560.
- 9Ponticelli C. Ischemiareperfusion injury: a major protagonist in kidney transplantation. Nephrol Dial Transplant. 2014; 29: 1134-1140.
- 10Gottlieb R. Cell death pathways in acute ischemia/reperfusion injury. J Cardiovasc Pharmacol Ther. 2011; 16: 233-238.
- 11Awad A, Rouse M, Huang L, et al. Compartmalization of neutrophils in the kidney and lung following acute ischemic kidney injury. Kidney Int. 2009; 75: 689-698.
- 12Fuquay R, Renner B, Kulik L, et al. Renal ischemiareperfusion injury amplifies the humoral immune response. J Am Soc Nephrol. 2013; 24: 1063-1072.
- 13Curci C, Castellano G, Stasi A, et al. Endothelialtomesenchymal transition and renal fibrosis in ischemia/reperfusion injury are mediated by complement anaphylatoxins and Akt pathway. Nephrol Dial Transplant. 2014; 29: 799-808.
- 14Solini S, Aiello S, Cassis P, et al. Prolonged ischemia accelerates cellular and humoral chronic rejection in a rat model of kidney transplantation. Transpl Int. 2012; 25: 347-356.
- 15Al Attas R, Al Abduladheem D, Shawhatti Adel A, et al. The dilemma of DQ HLA-antibodies. Hum Immunol. 2015; 76(5): 324-328. doi:10.1016/j.humimm.2015.03.008
- 16Nashan B, Abbud-Filho M, Citterio F. Prediction, prevention and management of delayed graft function: where are we now? Clin Transplant. 2016; 30: 1198-1208. doi:10.1111/ctr.12832
- 17Sharma AK, Tolani SL, Rathi GL, et al. Evaluation of factors causing delayed graft function in live related donor renal transplantation. Saudi J Kidney Dis Transpl. 2010; 21: 242-245.
- 18Pratschke J, Weiss S, Neuhaus P, et al. Review of nonimmunological causes for deteriorated graft function and graft loss after transplantation. Transpl Int. 2008; 21: 512-522.
- 19Senel FM, Karakayali H, Moray G, et al. Delayed graft unction: predictive factors and impact on outcome in living-related kidney transplantations. Ren Fail. 1998; 20: 589-595.
- 20Zhang Q, Reed EF. The importance of non-HLA antibodies in transplantation. Nat Rev Nephrol. 2016; 12(8): 484-495.
- 21Dragun D, Catar R, Philippe A. Non-HLA antibodies in solid organ transplantation: recent concepts and clinical relevance. Curr Opin Organ Transplant. 2013; 18(4): 430-435.
- 22Cardinal H, Dieudé M, Hébert MJ. The emerging importance of non-HLA autoantibodies in kidney transplant complications. J Am Soc Nephrol. 2017; 28(2): 400-406.
- 23Delville M, Charreau B, Rabant M, Legendre C, Anglicheau D. Pathogenesis of non-HLA antibodies in solid organ transplantation: where do we stand? Hum Immunol. 2016; 77(11): 1055-1062.
- 24Carroll RP, Riceman M, Hope CM, et al. Angiotensin II type1 receptor antibody (AT1Rab) associated humoral rejection and the effect of peri operative plasma exchange and candesartan. Hum Immunol. 2016; 77(12): 1154-1158.
- 25Taniguchi M, Rebellato LM, Cai J, et al. Higher risk of kidney graft failure in the presence of anti-angiotensin II type-1 receptor antibodies. Am J Transplant. 2013; 13(10): 2577-2589.
- 26Banasik M, Boratyńska M, KościelskaKasprzak K, et al. The influence of non-HLA antibodies directed against angiotensin II type 1 receptor (AT1R) on early renal transplant outcomes. Transpl Int. 2014; 27(10): 1029-1038.
- 27Yu S, Huh H, Lee KW, Park J, Kim SJ, Wooseong Huh, et. al. Pre-transplant angiotensin II type 1 receptor antibodies and Anti-endothelial cell antibodies predict graft function and allograft rejection in a Low-risk kidney transplantation setting. Ann Lab Med 2020; 40: 398–408.
- 28SasStrózik A, Krajewska M, Banasik M. The significance of angiotensin II type 1 receptor (AT1 receptor) in renal transplant injury. Adv Clin Exp Med. 2020; 29(5): 629-633.
- 29Philogene MC, Bagnasco S, Kraus ES, et al. Anti-angiotensin II type 1 receptor and anti-endothelial cell antibodies: a cross-sectional analysis of pathological findings in allograft biopsies. Transplantation. 2017; 101: 608-615.
- 30Pearl M, Qiuheng Z, Palma Diaz MF, et al. Angiotensin II type 1 receptor antibodies are associated with inflammatory cytokines and poor clinical outcomes in pediatric kidney transplantation. Kidney Int. 2018; 93(1): 260-269. doi:10.1016/j.kint.2017.06.034
- 31Breimer ME, Rydberg L, Jackson AM, et al. Multicenter evaluation of a novel endothelial cell crossmatch test in kidney transplantation. Transplantation. 2009; 87(4): 549-556.
- 32Niikura T, Yamaoto I, Nakada Y, et al. Probable C4d-negative accelerated acute antibody-mediated rejection due to non-HLA antibodies. Nephrol Ther. 2015; 20(Suppl 2): 75-78.
- 33Fuss A, Hope CM, Deayton S, Bennett GD, et al. C4d-negative antibody-mediated rejection with high anti-angiotensin II type I receptor antibodies in absence of donor-specific antibodies. Nephrol Ther. 2015; 20: 467-473.
- 34Jackson AM, Kuperman MB, Montgomery RA. Multiple hyperacute rejections in the absence of detectable complement activation in a patient with endothelial cell reactive antibody. Am J Transplant. 2012; 12(6): 1643-1649.
- 35Karahan GE, Claas FHJ, Heidt S. Heterologous immunity of virus-specific T cells leading to alloreactivity: possible implications for solid organ transplantation. Viruses. 2021; 13: 2359. doi:10.3390/v13122359
- 36Rowntree LC, van den Heuvel H, Sun J, et al. Preferential HLA-B27 allorecognition displayed by multiple cross-reactive antiviral CD8 (+) T cell receptors. Front Immunol. 2020; 11: 248.
- 37Almeida CA, van Miert P, O'Driscoll K, et al. Stimulation of HIV-specific T cell clonotypes using allogeneic HLA. Cell Immunol. 2017; 316: 32-34.
- 38Nguyen TH, Rowntree LC, Pellicci DG, et al. Recognition of distinct cross-reactive virus-specific CD8+ T cells reveals a unique TCR signature in a clinical setting. J Immunol. 2014; 192: 5039-5049.
- 39D'Orsogna LJ, Roelen DL, van der MeerPrins EM, et al. Tissue specificity of cross-reactive allogeneic responses by EBV EBNA3Aspecific memory T cells. Transplantation. 2011; 91: 494-500.
- 40van den Heuvel H, Heutinck KM, van der Meer-Prins EMW, et al. Allo-HLA cross-reactivities of cytomegalovirus-, influenza-, and varicella zoster virus-specific memory T cells are shared by different healthy individuals. Am J Transplant. 2017; 17(8): 2033-2044.
- 41Valujskikh A, Pantenburg B, Heeger PS. Primed allospecific T cells prevent the effects of costimulatory blockade on prolonged cardiac allograft survival in mice. Am J Transplant. 2002; 2: 501-509.
- 42Heeger PS, Greenspan NS, Kuhlenschmidt S, et al. Pretransplant frequency of donor-specific, IFN-gamma-producing lymphocytes is a manifestation of immunologic memory and correlates with the risk of posttransplant rejection episodes. J Immunol. 1999; 163: 2267-2275.
- 43Lakkis FG, Sayegh MH. Memory T cells: a hurdle to immunologic tolerance. J Am Soc Nephrol. 2003; 14: 2402-2410.
- 44Gill RG, Burrack AL. Diverse routes of allograft tolerance disruption by memory T cells. Front Immunol. 2020; 11:580483.
- 45Adams AB, Williams MA, Jones TR, et al. Heterologous immunity provides a potent barrier to transplantation tolerance. J Clin Investig. 2003; 111: 1887-1895.
- 46Mathews DV, Wakwe WC, Kim SC, et al. Belatacept resistant rejection is associated with CD28+ memory CD8 T cells. Am J Transplant. 2017; 17(9): 2285-2299.
- 47Nickel P, Presber F, Bold G, et al. Enzyme-linked immunosorbent spot assay for donor-reactive interferon-gamma-producing cells identifies T-cell presensitization and correlates with graft function at 6 and 12 months in renal-transplant recipients. Transplantation. 2004; 78: 1640-1646.
- 48Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID19 patients with severe respiratory failure. Cell Host Microbe. 2020; 7(6): 992-1000.
- 49Eggenhuizen PJ, Ng Boaz H, Chang J, et al. Heterologous immunity between SARS-CoV-2 and pathogenic bacteria. Front Immunol. 2022; 27:821595.
- 50Juskewitch E, Stubbs JR, Gandhi MJ. Elevated rate of HLA antibodies in male COVID-19 convalescent plasma donors: a risk factor for transfusion-related acute lung injury. Mayo Clin Proc. 2021; 96(2): 500.