Symptom-orientated oral hygiene for children after heart transplantation: Effectiveness of a standardized prophylactic program
Corresponding Author
Nelly Schulz-Weidner
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Correspondence
Nelly Schulz-Weidner, Department of Pediatric Dentistry, Medical Centre of Odontology, Justus-Liebig University Giessen, Schlangenzahl 14, 35392 Giessen, Germany.
Email: [email protected]
Search for more papers by this authorJulia C. Bulski
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorRachida Siahi-Benlarbi
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorJürgen Bauer
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorThushiha Logeswaran
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorChristian Jux
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorWilli-Eckhard Wetzel
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorNorbert Krämer
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorCorresponding Author
Nelly Schulz-Weidner
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Correspondence
Nelly Schulz-Weidner, Department of Pediatric Dentistry, Medical Centre of Odontology, Justus-Liebig University Giessen, Schlangenzahl 14, 35392 Giessen, Germany.
Email: [email protected]
Search for more papers by this authorJulia C. Bulski
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorRachida Siahi-Benlarbi
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorJürgen Bauer
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorThushiha Logeswaran
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorChristian Jux
Pediatric Heart Centre, Justus Liebig University, Giessen, Germany
Search for more papers by this authorWilli-Eckhard Wetzel
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorNorbert Krämer
Department of Pediatric Dentistry, Medical Centre of Odontology, Justus Liebig University, Giessen, Germany
Search for more papers by this authorAbstract
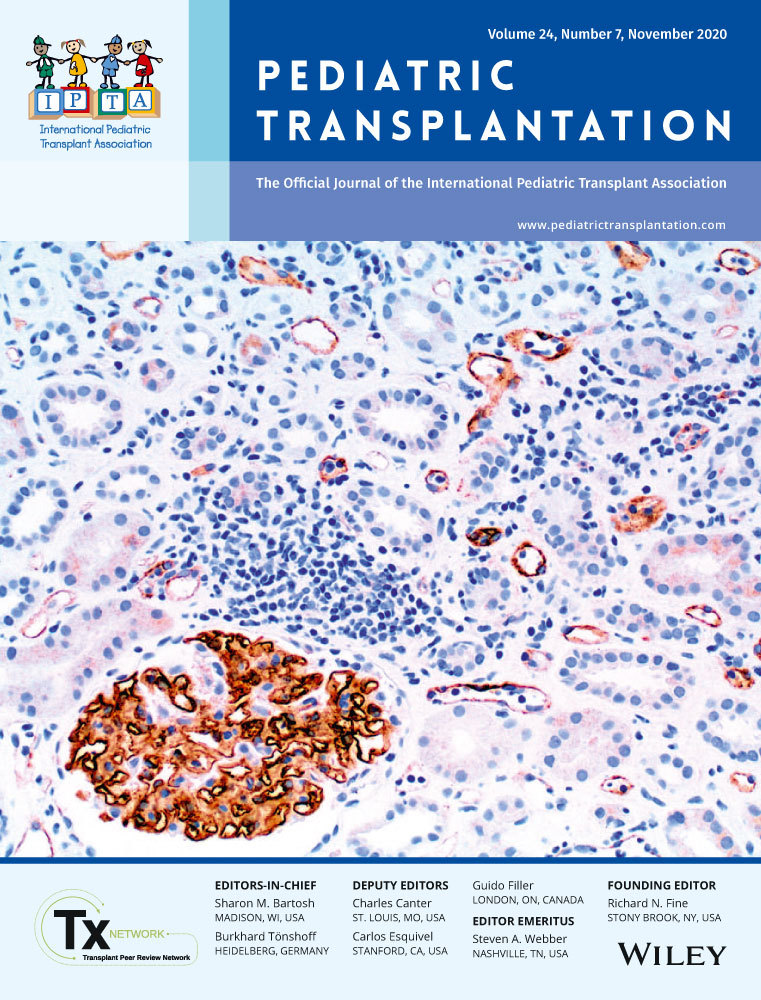
Children with CHD, especially heart-transplanted patients, are predisposed to have caries lesions, gingivitis and other oral findings like gingival hyperplasia. The aim of the study was the implementation of a specific oral hygiene program in these patients and its effect on the improvement of oral health, especially gingival overgrowth. For this, we used a newly developed systematic GHI to evaluate and describe this gingival alteration. Thirty-three children, aged 6 to 15 years with cardiac transplants (9 girls, 24 boys), were examined and introduced into a specific oral hygiene program. Each child showed evidence of gingival hyperplasia. They were randomly divided into three groups with the following oral care measurements: Group ZZ tooth brushing, Group ZZS tooth brushing and mouth rinsing, Group ZZSS tooth brushing, mouth rinsing and the use of an additional single and sulcus toothbrush. A significant decline of all oral health parameters could be proven in all groups. Gingival hyperplasia (GHI) improved as well as plaque accumulation (QHI). The children who used in addition to toothbrushing rinsing solutions and/or additional miniature toothbrushes showed better parameters of the gingival hygiene indexes from the baseline examination until the end of the study. The results show that any infant with cardiac transplant has to be introduced into an individualized oral hygiene program underlining the need of comprehensive dental care in cooperation with pediatric cardiology.
REFERENCES
- 1Lindinger A, Schwedler G, Hense HW. Prevalence of congenital heart defects in newborns in Germany: results of the first registration year of the PAN Study (July 2006 to June 2007). Klin Padiatr. 2010; 222(5): 321-326.
- 2Schwedler G, Lindinger A, Lange PE, et al. Frequency and spectrum of congenital heart defects among live births in Germany: a study of the Competence Network for Congenital Heart Defects. Clin Res Cardiol. 2011; 100(12): 1111-1117.
- 3Sivertsen TB, Assmus J, Greve G, Astrom AN, Skeie MS. Oral health among children with congenital heart defects in Western Norway. Eur Arch Paediatr Dent. 2016; 17(5): 397-406.
- 4Ansari F, Ferring V, Schulz-Weidner N, Wetzel WE. Concomitant oral findings in children after cardiac transplant. Pediatr Transplant. 2006; 10(2): 215-219.
- 5Ali HM, Mustafa M, Hasabalrasol S, et al. Presence of plaque, gingivitis and caries in Sudanese children with congenital heart defects. Clin Oral Investig. 2017; 21(4): 1299-1307.
- 6da Silva DB, Souza IP, Cunha MC. Knowledge, attitudes and status of oral health in children at risk for infective endocarditis. Int J Paediatr Dent. 2002; 12(2): 124-131.
- 7Pourmoghaddas Z, Meskin M, Sabri M, Norousali Tehrani MH, Najafi T. Dental Caries and Gingival Evaluation in Children with Congenital Heart Disease. Int J Prev Med. 2018; 9: 52.
- 8Stecksén-Blicks C, Rydberg A, Nyman L, Asplund S, Svanberg C. Dental caries experience in children with congenital heart disease: a case-control study. Int J Paediatr Dent. 2004; 14(2): 94-100.
- 9Hallett KB, Radford DJ, Seow WK. Oral health of children with congenital cardiac diseases: a controlled study. Pediatr Dent. 1992; 14(4): 224-230.
- 10Siahi-Benlarbi R, Nies SM, Sziegoleit A, Bauer J, Schranz D, Wetzel WE. Caries-, Candida- and Candida antigen/antibody frequency in children after heart transplantation and children with congenital heart disease. Pediatr Transplant. 2010; 14(6): 715-721.
- 11Busuttil Naudi A, Mooney G, El-Bahannasawy E, et al. The dental health and preventative habits of cardiac patients attending the Royal Hospital for Sick Children Glasgow. Eur Arch Paediatr Dent. 2006; 7(1): 23-30.
- 12Suvarna R, Rai K, Hegde AM. Knowledge and Oral Health Attitudes among Parents of Children with Congenital Heart Disease. Int J Clin Pediatr Dent. 2011; 4(1): 25-28.
- 13Hyland PL, McKeown ST, Mackenzie IC, Irwin CR. Regulation of keratinocyte growth factor and scatter factor in cyclosporin-induced gingival overgrowth. J Oral Pathol Med. 2004; 33(7): 391-397.
- 14Hyland PL, Traynor PS, Myrillas TT, et al. The effects of cyclosporin on the collagenolytic activity of gingival fibroblasts. J Periodontol. 2003; 74(4): 437-445.
- 15Chabria D, Weintraub RG, Kilpatrick NM. Mechanisms and management of gingival overgrowth in paediatric transplant recipients: a review. Int J Paediatr Dent. 2003; 13(4): 220-229.
- 16Kilpatrick NM, Weintraub RG, Lucas JO, Shipp A, Byrt T, Wilkinson JL. Gingival overgrowth in pediatric heart and heart-lung transplant recipients. J Heart Lung Transplant. 1997; 16(12): 1231-1237.
- 17Aldemir NM, Begenik H, Emre H, Erdur FM, Soyoral Y. Amlodipine-induced gingival hyperplasia in chronic renal failure: a case report. Afr Health Sci. 2012; 12(4): 576-578.
- 18Wright G, Welbury RR, Hosey MT. Cyclosporin-induced gingival overgrowth in children. Int J Paediatr Dent. 2005; 15(6): 403-411.
- 19Karpinia KA, Matt M, Fennell RS 3rd, Hefti AF. Factors affecting cyclosporine-induced gingival overgrowth in pediatric renal transplant recipients. Pediatr Dent. 1996; 18(7): 450-455.
- 20Farbod F, Kanaan H, Farbod J. Infective endocarditis and antibiotic prophylaxis prior to dental/oral procedures: latest revision to the guidelines by the American Heart Association published April 2007. Int J Oral Maxillofac Surg. 2009; 38(6): 626-631.
- 21Rateitschak KH, Rateitschak EM, Wolf HF. Ätiologie und Pathogenese. In: KH Rateitschak, ed. Parodontologie (Farbatlanten der Zahnmedizin), vol 2. Stuttgart: Georg Thieme Verlag; 1989: 149.
- 22Poveda-Roda R, Jimenez Y, Carbonell E, Gavalda C, Margaix-Munoz MM, Sarrion-Perez G. Bacteremia originating in the oral cavity. A review. Med Oral Patol Oral Cir Bucal. 2008; 13(6): E355-E362.
- 23Somacarrera ML, Lucas M, Cuervas-Mons V, Hernandez G. Oral care planning and handling of immunosuppressed heart, liver, and kidney transplant patients. Spec Care Dentist. 1996; 16(6): 242-246.
- 24Gutierrez JL, Bagan JV, Bascones A, et al. Consensus document on the use of antibiotic prophylaxis in dental surgery and procedures. Med Oral Patol Oral Cir Bucal. 2006; 11(2): E188-E205.
- 25Beaumont J, Chesterman J, Kellett M, Durey K. Gingival overgrowth: Part 1: aetiology and clinical diagnosis. Br Dent J. 2017; 222(2): 85-91.
- 26Franco E, Saunders CP, Roberts GJ, Suwanprasit A. Dental disease, caries related microflora and salivary IgA of children with severe congenital cardiac disease: an epidemiological and oral microbial survey. Pediatr Dent. 1996; 18(3): 228-235.
- 27Suma G, Usha MD, Ambika G. Oral health status of normal children and those affiliated with cardiac diseases. J Clin Pediatr Dent. 2011; 35(3): 315-318.
- 28Oettinger-Barak O, Machtei EE, Peled M, Barak S, IA LN, Laufer D. Cyclosporine A-induced gingival hyperplasia pemphigus vulgaris: literature review and report of a case. J Periodontol. 2000; 71(4): 650-656.
- 29Sezgin Y, Sezgin A. Periodontal status and dental behaviour of heart transplant recipients and healthy controls. Acta Odontol Scand. 2020; 78(1): 20-25.
- 30Saravia ME, Svirsky JA, Friedman R. Chlorhexidine as an oral hygiene adjunct for cyclosporine-induced gingival hyperplasia. ASDC J Dent Child. 1990; 57(5): 366-370.
- 31Guarnelli ME, Zangari F, Manfrini R, Scapoli C, Trombelli L. Evaluation of additional amine fluoride/stannous fluoride-containing mouthrinse during supportive therapy in patients with generalized aggressive periodontitis. A randomized, crossover, double-blind, controlled trial. J Clin Periodontol. 2004; 31(9): 742-748.
- 32Banoczy J, Szoke J, Kertesz P, Toth Z, Zimmermann P, Gintner Z. Effect of amine fluoride/stannous fluoride-containing toothpaste and mouthrinsings on dental plaque, gingivitis, plaque and enamel F-accumulation. Caries Res. 1989; 23(4): 284-288.
- 33Bass L. First steps to dental care. Chronicle. 1965; 28: 187.
- 34 World Health Organization (WHO). Dental caries indices: tooth (DMFT, dmft) and surface levels (DMFS, dmfs). In: World Health Organization (WHO), ed. Oral Health Surveys: Basic Methods, 5th edn. Geneva: WHO Press; 2013: 51-56.
- 35Pieper K, Blumenstein A. Die zahnmedizinische Untersuchung im Rahmen der Gruppenprophylaxe: ein Leitfaden für die EDV-gestützte Erfolgskontrolle. Marburg; 1993.
- 36Fleiss JL, Park MH, Chilton NW, Alman JE, Feldman RS, Chauncey HH. Representativeness of the "Ramfjord teeth" for epidemiologic studies of gingivitis and periodontitis. Community Dent Oral Epidemiol. 1987; 15(4): 221-224.
- 37Ramfjord SP. Indices for Prevalence and Incidence of Periodontal Disease. J Periodontol. 1959; 30(1): 51-59.
10.1902/jop.1959.30.1.51 Google Scholar
- 38Silness J, Loe H. Periodontal Disease in Pregnancy. II. Correlation between Oral Hygiene and Periodontal Condtion. Acta Odontol Scand. 1964; 22: 121-135.
- 39Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962; 65: 26-29.
- 40Siahi-Benlarbi R, Schulz-Weidner N, Krämer N, Wetzel W-E. Symptomorientiertes Oralhygieneprogramm bei immunsupprimierten Patienten nach Herztransplantation (published abstract). Oralprophylaxe & Kinderzahnheilkd. 2011; 33(3): 139.
- 41Angelopoulos AP, Goaz PW. Incidence of diphenylhydantoin gingival hyperplasia. Oral Surg Oral Med Oral Pathol. 1972; 34(6): 898-906.
- 42Miller CS, Damm DD. Incidence of verapamil-induced gingival hyperplasia in a dental population. J Periodontol. 1992; 63(5): 453-456.
- 43Seymour RA, Smith DG, Turnbull DN. The effects of phenytoin and sodium valproate on the periodontal health of adult epileptic patients. J Clin Periodontol. 1985; 12(6): 413-419.
- 44Miranda J, Brunet L, Roset P, Berini L, Farre M, Mendieta C. Prevalence and risk of gingival enlargement in patients treated with nifedipine. J Periodontol. 2001; 72(5): 605-611.
- 45Miranda J, Brunet L, Roset P, Berini L, Farre M, Mendieta C. Prevalence and risk of gingival overgrowth in patients treated with diltiazem or verapamil. J Clin Periodontol. 2005; 32(3): 294-298.
- 46Thumeyer A, Splieth CH. Individuelle Prophylaxe plus Gruppenprophylaxe für eine optimale orale Gesundheit. Quintessenz. 2010; 61(9): 1031-1038.
- 47Thumeyer A. Gruppenprophylaxe für Kinder von 0 bis 6 Jahren. Zahnmedizin up2date. 2018; 12(06): 507-522.
10.1055/a-0673-9855 Google Scholar
- 48Banach J, Wiernicka-Menkiszak M, Mazurek-Mochol M, Trabska-Swistelnicka M, Betlega-Gromada K. The effect of Meridol toothpaste and Meridol mouthrinse on the reduction of bacterial plaque and gingival inflammations. Czas Stommatol. 2007; 60: 11-19.
- 49Aimetti M, Romano F, Priotto P, Debernardi C. Non-surgical periodontal therapy of cyclosporin A gingival overgrowth in organ transplant patients. Clinical results at 12 months. Minerva Stomatol. 2005; 54(5): 311-319.
- 50Somacarrera ML, Lucas M, Scully C, Barrios C. Effectiveness of periodontal treatments on cyclosporine-induced gingival overgrowth in transplant patients. Br Dent J. 1997; 183(3): 89-94.
- 51Barak S, Engelberg IS, Hiss J. Gingival hyperplasia caused by nifedipine. Histopathologic findings. J Periodontol. 1987; 58(9): 639-642.
- 52Tyldesley WR, Rotter E. Gingival hyperplasia induced by cyclosporin-A. Br Dent J. 1984; 157(9): 305-309.
- 53Thomason JM, Seymour RA, Ellis JS, et al. Determinants of gingival overgrowth severity in organ transplant patients. An examination of the role of HLA phenotype. J Clin Periodontol. 1996; 23(7): 628-634.
- 54Greenberg KV, Armitage GC, Shiboski CH. Gingival enlargement among renal transplant recipients in the era of new-generation immunosuppressants. J Periodontol. 2008; 79(3): 453-460.
- 55Seymour RA, Smith DG. The effect of a plaque control programme on the incidence and severity of cyclosporin-induced gingival changes. J Clin Periodontol. 1991; 18(2): 107-110.
- 56Seymour RA, Smith DG, Rogers SR. The comparative effects of azathioprine and cyclosporin on some gingival health parameters of renal transplant patients. A longitudinal study. J Clin Periodontol. 1987; 14(10): 610-613.
- 57Ingles E, Rossmann JA, Caffesse RG. New clinical index for drug-induced gingival overgrowth. Quintessence Int. 1999; 30(7): 467-473.
- 58Liu Z, Yu D, Zhou L, et al. Counseling role of primary care physicians in preventing early childhood caries in children with congenital heart disease. Int J Environ Res Public Health. 2014; 11(12): 12716-12725.
- 59Grahn K, Wikström S, Nyman L, Rydberg A, Stecksén-Blicks C. Attitudes about dental care among parents whose children suffer from severe congenital heart disease: a case-control study. Int J Paediatr Dent. 2006; 16(4): 231-238.
- 60Ali HM, Mustafa M, Nasir EF, et al. Oral-health-related background factors and dental service utilisation among Sudanese children with and without a congenital heart defects. BMC Oral Health. 2016; 16(1): 123.
- 61Sivertsen TB, Astrom AN, Greve G, Assmus J, Skeie MS. Effectiveness of an oral health intervention program for children with congenital heart defects. BMC Oral Health. 2018; 18(1): 50.