Electrogram dispersion–guided driver ablation adjunctive to high-quality pulmonary vein isolation in atrial fibrillation of varying durations
Abstract
Objective
To investigate the role of driver mechanism and the effect of electrogram dispersion–guided driver mapping and ablation in atrial fibrillation (AF) at different stages of progression.
Methods
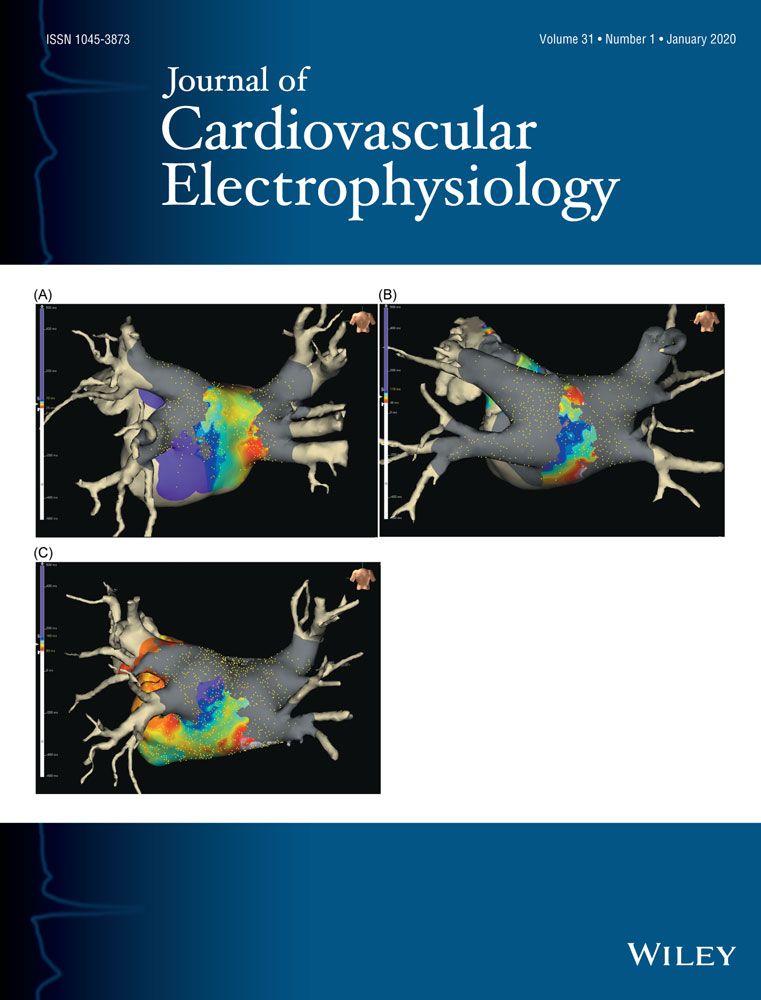
A total of 256 consecutive patients with AF who had undergone pulmonary vein isolation (PVI) plus driver ablation or conventional ablation were divided into three groups: paroxysmal atrial fibrillation (PAF; group A, n = 51); persistent atrial fibrillation (PsAF; group B, n = 38); and long standing–persistent atrial fibrillation (LS-PsAF; group C, n = 39). PVI was performed with the guidance of the ablation index. The electrogram dispersion was analyzed for driver mapping.
Results
The most prominent driver regions were at roof (28.0%), posterior wall (17.6%), and bottom (21.3%). From patients with PAF to those with PsAF and LS-PsAF: the complexity of extra-pulmonary vein (PV) drivers including distribution, mean number, and area of dispersion region increased (P < .001). Patients who underwent driver ablation vs conventional ablation had higher procedural AF termination rate (76.6% vs 28.1%; P < .001). With AF progression, the termination rate gradually decreased from group A to group C, and the role of PVI in AF termination was also gradually weakened from group A to group C (39.6%, 7.4%, and 4.3%; P < .001) in patients with driver ablation. At the end of the follow-up, the rate of sinus rhythm maintenance was higher in patients with driver ablation than those with conventional ablation (89.1% vs 70.3%; P < .001).
Conclusion
The formation of extra-PV drivers provides an important mechanism for AF maintenance with their complexity increasing with AF progression. Electrogram dispersion–guided driver ablation appears to be an efficient adjunctive approach to PVI for AF treatment.