CBC With Differential and Cell Population Data in Prediction of Fever With Thrombocytopenia Syndrome
Funding: This work was supported by National Natural Science Foundation of China (Grant/award number: 82272401), Jiangsu Province Capability Improvement Project through Science and Technology and Education (Grant/award number: ZDXK202239).
Lixia Zhang and Shuxian Yang contributed equally to this work.
ABSTRACT
Introduction
We aimed to identify additional predictors of severe fever with thrombocytopenia syndrome (SFTS), which has a significantly increasing global incidence.
Methods
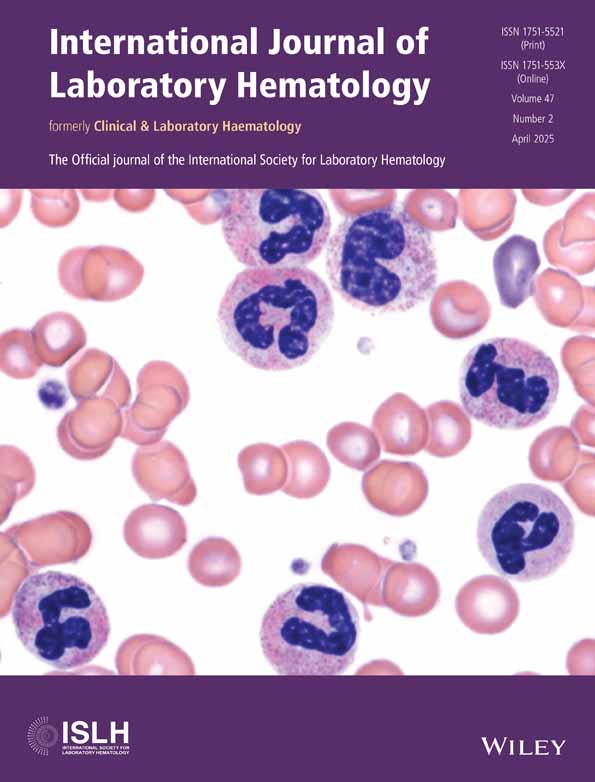
This retrospective study included 95 patients with SFTS and 30 healthy individuals. Complete blood count with differential was performed using Sysmex XN 9000 and Mindray BC-6800 Plus analyzers. Extended leukocyte cell population data (CPD) parameters were acquired using a Mindray BC-6800 Plus analyzer. Peripheral smears were identified, and SFTS virus (SFTSV) RNA was detected using real-time reverse transcription polymerase chain reaction.
Results
Of 95 patients with SFTS at admission, 75.8% (72/95) presented leukopenia and 96.8% (92/95) thrombocytopenia with SFTS. Neutrophil left shift and smudge cells (32.4/WBC ± 28.2/WBC) were observed 100% (57/57) on the blood smear. Only 21.1% (21/57) of the reactive lymphocytes were > 5% (3.24% ± 3.35%). Moreover, 33.3% (19/57) of apoptotic lymphocytes and 8.8% (5/57) of nucleated red blood cells were present. Furthermore, 78.9% (45/57) of reactive plasmacytoid lymphocytes increased 3–5 days after admission and 61.1% (11/18) of the patients who died presented with dust blue inclusions in the neutrophils. Compared to the control group, Neu-Y and all lymphocyte and monocyte CPD parameters were significantly higher in all SFTS groups. Compared to the surviving patients with SFTS, Lym-Y in Group 2 (p < 0.05) was significantly lower, but Neu-Y and Mon-Z in Group 3 were higher (p < 0.001) in the death group.
Conclusions
The cell count, peripheral blood morphology, and CPD parameters described in this study had a strong prompting effect on SFTSV infection.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data in this study are not publicly available The data that support the findings of this study are available from the corresponding author upon reasonable request.