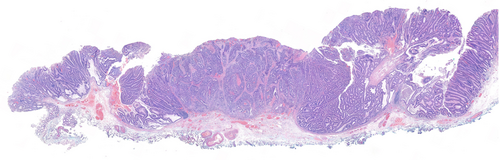
Pitfalls during histological assessment in locally resected pT1 colorectal cancer
Emma J Norton
Department of Cellular Pathology, University Hospital Southampton NHS Foundation Trust, Southampton, UK
Search for more papers by this authorCorresponding Author
Adrian C Bateman
Department of Cellular Pathology, University Hospital Southampton NHS Foundation Trust, Southampton, UK
Address for correspondence: Adrian C Bateman, Department of Cellular Pathology, MP002, Level E, South Block, Southampton General Hospital, Tremona Road, Southampton SO16 6YD, UK. e-mail: [email protected]
Search for more papers by this authorEmma J Norton
Department of Cellular Pathology, University Hospital Southampton NHS Foundation Trust, Southampton, UK
Search for more papers by this authorCorresponding Author
Adrian C Bateman
Department of Cellular Pathology, University Hospital Southampton NHS Foundation Trust, Southampton, UK
Address for correspondence: Adrian C Bateman, Department of Cellular Pathology, MP002, Level E, South Block, Southampton General Hospital, Tremona Road, Southampton SO16 6YD, UK. e-mail: [email protected]
Search for more papers by this authorAbstract
Colorectal cancer (CRC) is a common malignancy worldwide, and the stage of the tumour is closely related to clinical outcome. Bowel cancer screening programmes have resulted in the identification of colorectal cancer at earlier stages. Approximately 10% of patients with the earliest stage of CRC (i.e. pT1) will possess regional lymph node metastases (LNM). Therefore, if these patients have initially been treated by local resection (e.g. polypectomy), this subgroup will require surgical resection. Identification of pathological risk factors for LNM within locally resected pT1 CRC is a very important process during the histological assessment of these lesions. This paper describes the most commonly encountered and clinically significant difficulties in the histological assessment of these cases. These pitfalls are illustrated using four examples of locally resected pT1 CRC that were received by our department during routine diagnostic practice.
Graphical Abstract
This paper describes the most commonly encountered and clinically significant difficulties in the histological assessment of risk factors for regional lymph node metastases in locally resected early (i.e. pT1) colorectal cancer (CRC). These are illustrated using four examples that were received by our department during routine diagnostic practice.
Conflicts of interest
The authors report no relevant conflicts of interest.
Open Research
Data availability statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
- 1Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017; 66; 683–691.
- 2 Cancer Research UK. Bowel cancer statistics. [cited 2024 August 21]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/.
- 3Brierley J, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. Chichester, West Sussex, UK: John Wiley & Sons, Inc., 2017.
- 4Haggar FA, Boushey RP. Colorectal cancer epidemiology: Incidence, mortality, survival, and risk factors. Clin. Colon Rectal Surg. 2009; 22; 191–197.
- 5 National Bowel Cancer Audit. State of the Nation Report. [cited 2024 Jul 17]. Available from: https://www.nboca.org.uk/reports/state-of-the-nation-report/.
- 6Takamatsu M, Yamamoto N, Kawachi H et al. Prediction of lymph node metastasis in early colorectal cancer based on histologic images by artificial intelligence. Sci. Rep. 2022; 12; 2963.
- 7Min S, Hwang SW, Park SH et al. Comparative cost analysis between endoscopic resection and surgery for submucosal colorectal cancer. Dis. Colon Rectum 2023; 66; 723–732.
- 8Borowski DW, Cawkwell S, Amir Zaidi SM et al. The NHS bowel cancer screening Programme achieves the anticipated survival improvement, but participation must be improved. Int. J. Health Care Qual. Assur. 2018; 31; 106–115.
- 9 NHS bowel cancer screening (BCSP) programme. Bowel cancer screening: pathology guidance on reporting lesions. [cited 2024 Jul 17]. Available from: https://www.gov.uk/government/publications/bowel-cancer-screening-reporting-lesions/bowel-cancer-screening-guidance-on-reporting-lesions.
- 10Loughrey MB, Quirke P, Shepherd NA, Royal College of Pathologists. Standards and datasets for reporting cancers. Dataset for histopathological reporting of colorectal cancer. [cited 2024 Jul 17]. https://www.rcpath.org/static/c8b61ba0-ae3f-43f1-85ffd3ab9f17cfe6/c19a5cd7-3485-44c2-b5e1c87154830582/G049-Dataset-for-histopathological-reporting-of-colorectal-cancer.pdf.
- 11Beaton C, Twine CP, Williams GL, Radcliffe AG. Systematic review and meta-analysis of histopathological factors influencing the risk of lymph node metastasis in early colorectal cancer. Color. Dis. 2013; 15; 788–797.
- 12Choi JY, Jung SA, Shim KN et al. Meta-analysis of predictive clinicopathologic factors for lymph node metastasis in patients with early colorectal carcinoma. J. Korean Med. Sci. 2015; 30; 398–406.
- 13Wada H, Shiozawa M, Katayama K et al. Systematic review and meta-analysis of histopathological predictive factors for lymph node metastasis in T1 colorectal cancer. J. Gastroenterol. 2015; 50; 727–734.
- 14Berg KB, Telford JJ, Gentile L, Schaeffer DF. Re-examining the 1mm margin and submucosal depth of invasion: A review of 216 malignant colorectal polyps. Virchows Arch. 2020; 476; 863–870.
- 15Cappellesso R, Nicolè L, Zanco F et al. Synchronous nodal metastatic risk in screening detected and endoscopically removed pT1 colorectal cancers. Pathol. Res. Pract. 2020; 216; 152966.
- 16Dykstra MA, Gimon TI, Ronksley PE et al. Classic and novel histopathologic risk factors for lymph node metastasis in T1 colorectal cancer: A systematic review and meta-analysis. Dis. Colon Rectum 2021; 64; 1139–1150.
- 17Ebbehøj AL, Jørgensen LN, Krarup PM, Smith HG. Histopathological risk factors for lymph node metastases in T1 colorectal cancer: Meta-analysis. Br. J. Surg. 2021; 108; 769–776.
- 18Ichimasa K, Kudo SE, Miyachi H et al. Current problems and perspectives of pathological risk factors for lymph node metastasis in T1 colorectal cancer: Systematic review. Dig. Endosc. 2022; 34; 901–912.
- 19Zwager LW, Bastiaansen BAJ, Montazeri NSM et al. Deep submucosal invasion is not an independent risk factor for lymph node metastasis in T1 colorectal cancer: A meta-analysis. Gastroenterology 2022; 163; 174–189.
- 20Watanabe J, Ichimasa K, Kataoka Y et al. Diagnostic accuracy of highest-grade or predominant histological differentiation of T1 colorectal cancer in predicting lymph node metastasis: A systematic review and meta-analysis. Clin. Transl. Gastroenterol. 2024; 15; e00673.
- 21Norton EJ, Bateman AC. Risk assessment in pT1 colorectal cancer. J. Clin. Pathol. 2024; 77; 225–232.
- 22Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD. Prognostic factors in colorectal carcinomas arising in adenomas: Implications for lesions removed by endoscopic polypectomy. Gastroenterology 1985; 89; 328–336.
- 23Song J, Yin H, Zhu Y et al. Identification of predictive factors for lymph node metastasis in pT1 stage colorectal cancer patients: A retrospective analysis based on the population database. Pathol. Oncol. Res. 2022; 28; 1610191.
- 24Oh JR, Park B, Lee S et al. Nomogram development and external validation for predicting the risk of lymph node metastasis in T1 colorectal cancer. Cancer Res. Treat. 2019; 51; 1275–1284.
- 25Brown I, Zammit AP, Bettington M et al. Pathological features associated with metastasis in patients with early invasive (pT1) colorectal carcinoma in colorectal polyps. Histopathology 2023; 83; 591–606.
- 26Toh E-W, Brown P, Morris E et al. Area of submucosal invasion and width of invasion predicts lymph node metastasis in pT1 colorectal cancers. Dis. Colon Rectum 2015; 58; 393–400.
- 27Shivji S, Conner JR, Barresi V, Kirsch R. Poorly differentiated clusters in colorectal cancer: A current review and implications for future practice. Histopathology 2020; 77; 351–368.
- 28Ebbehøj AL, Smith HG, Jørgensen LN. Prognostic factors for lymph node metastases in pT1 colorectal cancer differ according to tumor morphology: A nationwide cohort study. Ann. Surg. 2023; 277; 127–135.
- 29Guo K, Feng Y, Yuan L et al. Risk factors and predictors of lymph nodes metastasis and distant metastasis in newly diagnosed T1 colorectal cancer. Cancer Med. 2020; 9; 5095–5113.
- 30Haupt B, Ro JY, Schwartz MR, Shen SS. Colorectal adenocarcinoma with micropapillary pattern and its association with lymph node metastasis. Mod. Pathol. 2007; 20; 729–733.
- 31Xu F, Xu J, Lou Z et al. Micropapillary component in colorectal carcinoma is associated with lymph node metastasis in T1 and T2 stages and decreased survival time in TNM stages I and II. Am. J. Surg. Pathol. 2009; 33; 1287–1292.
- 32Bateman AC, Kurn OR, Novelli MR, Rodriguez-Justo M, Shepherd NA, Wong NACS. The bowel cancer screening programme expert board – An analysis of activity during 2017-2020. Histopathology 2022; 80; 782–789.
- 33Loughrey MB, Shepherd NA. The pathology of bowel cancer screening. Histopathology 2015; 66; 66–77.
- 34Yantiss R, Bosenberg M, Antonioli D et al. Utility of MMP-1, p53, E-cadherin, and collagen IV immunohistochemical stains in the differential diagnosis of adenomas with misplaced epithelium versus adenomas with invasive adenocarcinoma. Am. J. Surg. Pathol. 2002; 26; 206–215.
- 35Rosty C, Webster F, Nagtegaal ID. Pathology reporting of colorectal local excision species: Recommendations from the international collaboration on cancer reporting (ICCR). Gastroenterology 2021; 161; 382–387.
- 36Berg KB, Telford JJ, Gentile L, Schaeffer DF. Re-examining the 1-mm margin and submucosal depth of invasion: A review of 216 malignant colorectal polyps. Virchows Arch. 2020; 476; 863–870.
- 37Lugli A, Kirsch R, Ajioka Y et al. Recommendations for reporting tumor budding in colorectal cancer based on the international tumor budding consensus conference (ITBCC) 2016. Mod. Pathol. 2017; 30; 1299.
- 38Fuccio L, Hassan C, Ponchon T et al. Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: A systematic review and meta-analysis. Gastrointest. Endosc. 2017; 86; 74–86.
- 39Santos JB, Nobre MRC, Oliveira CZ et al. Risk factors for adverse events of colorectal endoscopic submucosal dissection: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2021; 33; e33–e41.
- 40Kikuchi R, Takano M, Takagi K et al. Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis. Colon Rectum 1995; 38; 1286–1295.
- 41Tateishi Y, Nakanishi Y, Taniguchi H, Shimoda T, Umemura S. Pathological prognostic factors predicting lymph node metastasis in submucosal invasive (T1) colorectal carcinoma. Mod. Pathol. 2010; 23; 1068–1072.
- 42Nakadoi K, Oka S, Tanaka S et al. Condition of muscularis mucosae is a risk factor for lymph node metastasis in T1 colorectal carcinoma. Surg. Endosc. 2014; 28; 1269–1276.
- 43Miyachi H, Kudo SE, Ichimasa K et al. Management of T1 colorectal cancers after endoscopic treatment based on the risk stratification of lymph node metastasis. J. Gastroenterol. Hepatol. 2016; 31; 1126–1132.
- 44Ueno H, Mochizuki H, Hashiguchi Y et al. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology 2004; 127; 385–394.
- 45Kawachi H, Eishi Y, Ueno H et al. A three-tier classification system based on the depth of submucosal invasion and budding/sprouting can improve the treatment strategy for T1 colorectal cancer: A retrospective multicenter study. Mod. Pathol. 2015; 28; 872–879.
- 46Hashiguchi Y, Muro K, Saito Y et al. Japanese Society for Cancer of the colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int. J. Clin. Oncol. 2020; 25; 1–42.
- 47Kouyama Y, Kudo SE, Miyachi H et al. Practical problems of measuring depth of submucosal invasion in T1 colorectal carcinomas. Int. J. Color. Dis. 2016; 31; 137–146.
- 48Ahadi M, Sokolova A, Brown I, Chou A, Gill AJ. The 2019 World Health Organization classification of appendiceal, colorectal and anal canal tumours: An update and critical assessment. Pathology 2021; 53; 454–461.
- 49van der Schee L, Verbeeck A, Deckers IAG et al. Variation in the detection of lymphovascular invasion in T1 colorectal cancer and its impact on treatment: A nationwide Dutch study. United European Gastroenterol J 2024; 12; 1429–1439.
- 50Suzuki A, Togashi K, Nokubi M et al. Evaluation of venous invasion by Elastica van Gieson stain and tumor budding predicts local and distant metastases in patients with T1 stage colorectal cancer. Am. J. Surg. Pathol. 2009; 33; 1601–1607.
- 51Barel F, Auffret A, Cariou M et al. High reproducibility is attainable in assessing histoprognostic parameters of pT1 colorectal cancer using routine histopathology slides and immunohistochemistry analyses. Pathology 2019; 51; 46–54.
- 52Cooper HS. Pathology of the endoscopically removed malignant colorectal polyp. Curr. Diagn. Pathol. 2007; 13; 423–437.
10.1016/j.cdip.2007.06.002 Google Scholar
- 53Nishishita R, Morohashi S, Seino H et al. Expression of cancer-associated fibroblast markers in advanced colorectal cancer. Oncol. Lett. 2018; 15; 6195–6202.
Online Version of Record before inclusion in an issue