The relationship between excess sodium intake and metabolic syndrome: Worth consideration?
Corresponding Author
Baris Afsar
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Correspondence
Baris Afsar, Department of Nephrology, Saint Louis University, School of Medicine, SSM Health Saint Louis University Hospital, Saint Louis, MO, USA.
Email: [email protected]
Search for more papers by this authorRengin Elsurer Afsar
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorSaid Mowaffaq
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorGeetha Maddukuri
Division of Nephrology and Hypertension, VA Saint Louis Health Care System, Saint Louis, Missouri, USA
Search for more papers by this authorKrista L. Lentine
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorCorresponding Author
Baris Afsar
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Correspondence
Baris Afsar, Department of Nephrology, Saint Louis University, School of Medicine, SSM Health Saint Louis University Hospital, Saint Louis, MO, USA.
Email: [email protected]
Search for more papers by this authorRengin Elsurer Afsar
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorSaid Mowaffaq
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorGeetha Maddukuri
Division of Nephrology and Hypertension, VA Saint Louis Health Care System, Saint Louis, Missouri, USA
Search for more papers by this authorKrista L. Lentine
Division of Nephrology, School of Medicine, Saint Louis University, SSM Health Saint Louis University Hospital, Saint Louis, Missouri, USA
Search for more papers by this authorAbstract
Background
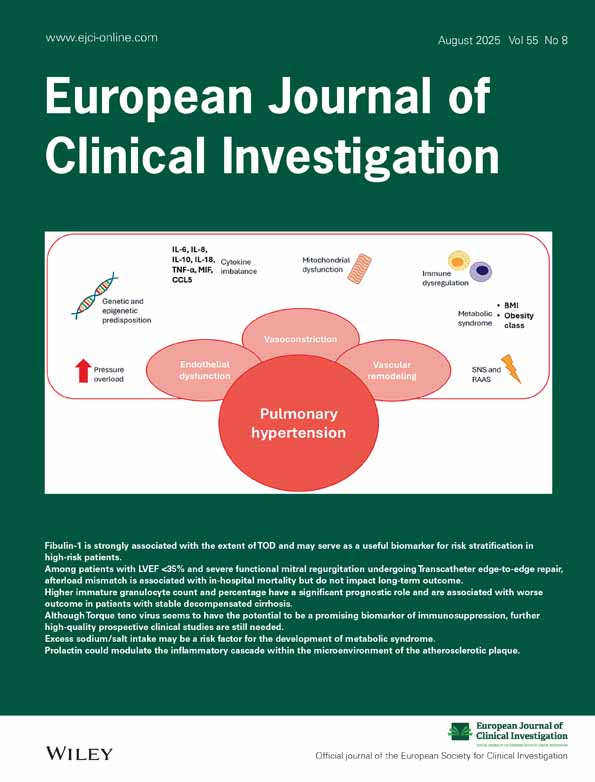
The prevalence of metabolic syndrome (MetS) is increasing worldwide. The change in nutrition and eating patterns contributes partly to this rise. On the other hand, increased sodium intake is common in most of the world. There are some studies showing that increased sodium intake may be associated with MetS.
Methods
To provide an overview of the current evidence regarding the relationship between excess sodium/salt intake and MetS, we performed a literature search of PubMed/Medline, Web of Science and Google Scholar until October 2024 to recruit studies examining the relationship between sodium/salt intake and MetS.
Results
Our review showed that most but not all cross-sectional studies have shown that excess sodium/salt intake is associated with the presence of MetS. Additionally, few longitudinal studies also demonstrated that excess sodium intake is related with the development of new MetS. These studies are mostly observational, and mechanistic studies explaining underlying mechanisms are lacking. The most correlated components of MetS associated with high salt intake were blood pressure and waist circumference, while the correlations between HDL-C, TG and FG were variable.
Conclusions
These findings suggest that excess sodium/salt intake may be a risk factor for the development of MetS.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
This review has no original data to share.
REFERENCES
- 1Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112(17): 2735-2752. doi:10.1161/CIRCULATIONAHA.105.169404
- 2Brey CW, Akbari-Alavijeh S, Ling J, et al. Salts and energy balance: a special role for dietary salts in metabolic syndrome. Clin Nutr. 2019; 38(5): 1971-1985.
- 3Ribeiro NG, Lelis DF, Molina M, et al. The high salt intake in adults with metabolic syndrome is related to increased waist circumference and blood pressure: the Brazilian longitudinal study of adult health study (ELSA-Brasil). Nutrition. 2023; 114:112108. doi:10.1016/j.nut.2023.112108
- 4Soltani S, Kolahdouz Mohammadi R, Shab-Bidar S, Vafa M, Salehi-Abargouei A. Sodium status and the metabolic syndrome: a systematic review and meta-analysis of observational studies. Crit Rev Food Sci Nutr. 2019; 59(2): 196-206.
- 5Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2009; 19(2): 123-128.
- 6Räisänen JP, Silaste ML, Kesäniemi YA, Ukkola O. Increased daily sodium intake is an independent dietary indicator of the metabolic syndrome in middle-aged subjects. Ann Med. 2012; 44(6): 627-634.
- 7Rhee MY, Kim JH, Kim YS, et al. High sodium intake in women with metabolic syndrome. Korean Circ J. 2014; 44(1): 30-36.
- 8Rodrigues SL, Baldo MP, de Sá Cunha R, et al. Salt excretion in normotensive individuals with metabolic syndrome: a population-based study. Hypertens Res. 2009; 32(10): 906-910. doi:10.1038/hr.2009.122
- 9Ohta Y, Tsuchihashi T, Arakawa K, Onaka U, Ueno M. Prevalence and lifestyle characteristics of hypertensive patients with metabolic syndrome followed at an outpatient clinic in fukuoka, Japan. Hypertens Res. 2007; 30(11): 1077-1082.
- 10Baudrand R, Campino C, Carvajal CA, et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin Endocrinol (Oxf). 2014; 80(5): 677-684. doi:10.1111/cen.12225
- 11Unal A, Kocyigit I, Sipahioglu MH, Tokgoz B, Oymak O. The relationship between daily urinary sodium excretion and metabolic syndrome in patients with kidney transplantation. Ann Transplant. 2014; 19: 397-402.
- 12Safa K, Ohori S, Borges TJ, et al. Salt accelerates allograft rejection through serum- and glucocorticoid-regulated kinase-1-dependent inhibition of regulatory T Cells. J Am Soc Nephrol. 2015; 26(10): 2341-2347.
- 13Oh SW, Han KH, Han SY, Koo HS, Kim S, Chin HJ. Association of sodium excretion with metabolic syndrome, Insulin resistance, and body fat. Medicine (Baltimore). 2015; 94(39):e1650.
- 14Won JC, Hong JW, Noh JH, Kim DJ. Association between estimated 24-h urinary sodium excretion and metabolic syndrome in Korean adults: the 2009 to 2011 Korea National Health and Nutrition Examination Survey. Medicine (Baltimore). 2016; 95(15):e3153.
- 15Seo JE, Lee HS, Lee SW, et al. The association between urinary sodium excretion and metabolic syndrome in Korean adults from the 2010-2011 Korean National Health and Nutrition Examination Survey. Korean J Fam Med. 2017; 38(4): 199-205.
- 16Takase H, Hayashi K, Kin F, et al. Dietary salt intake predicts future development of metabolic syndrome in the general population. Hypertens Res. 2023; 46(1): 236-243.
- 17Yin L, Li S, He Y, et al. Impact of urinary sodium excretion on the prevalence and incidence of metabolic syndrome: a population-based study. BMJ Open. 2023; 13(4):e065402.
- 18Teramoto T, Kawamori R, Miyazaki S, Teramukai S. Sodium intake in men and potassium intake in women determine the prevalence of metabolic syndrome in Japanese hypertensive patients: OMEGA Study. Hypertens Res. 2011; 34(8): 957-962.
- 19Huh JH, Lim JS, Lee MY, Chung CH, Shin JY. Gender-specific association between urinary sodium excretion and body composition: Analysis of the 2008-2010 Korean National Health and Nutrition Examination Surveys. Metabolism. 2015; 64(7): 837-844.
- 20Cheng M, Wang H, Wang Z, Du W, Ouyang Y, Zhang B. Relationship between dietary factors and the number of altered metabolic syndrome components in Chinese adults: a cross-sectional study using data from the China Health and Nutrition Survey. BMJ Open. 2017; 7(5):e014911.
- 21Kim BK, Lim YH, Kim SG, Kim YM, Shin J. Relationship between sodium intake and blood pressure according to metabolic syndrome status in the Korean National Health and Nutrition Examination Survey. Blood Press Monit. 2012; 17(3): 120-127.
- 22Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988; 297(6644): 319-328.
- 23He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013; 346:f1325.
- 24Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001; 344(1): 3-10. doi:10.1056/NEJM200101043440101
- 25Uzu T, Kimura G, Yamauchi A, et al. Enhanced sodium sensitivity and disturbed circadian rhythm of blood pressure in essential hypertension. J Hypertens. 2006; 24(8): 1627-1632.
- 26Chen J, Gu D, Huang J, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009; 373(9666): 829-835.
- 27Guyton AC. Blood pressure control--special role of the kidneys and body fluids. Science. 1991; 252(5014): 1813-1816.
- 28Kanbay M, Yilmaz S, Dincer N, et al. Antidiuretic hormone and serum osmolarity physiology and related outcomes: what is old, what is new, and what is unknown? J Clin Endocrinol Metab. 2019; 104(11): 5406-5420.
- 29He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension. 2008; 51(3): 629-634.
- 30Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005; 365(9468): 1415-1428.
- 31Zhao X, An X, Yang C, Sun W, Ji H, Lian F. The crucial role and mechanism of insulin resistance in metabolic disease. Front Endocrinol (Lausanne). 2023; 14:1149239.
- 32Shimamoto K, Hirata A, Fukuoka M, et al. Insulin sensitivity and the effects of insulin on renal sodium handling and pressor systems in essential hypertensive patients. Hypertension. 1994; 23(1 Suppl): I29-I33.
- 33Galletti F, Strazzullo P, Ferrara I, et al. NaCl sensitivity of essential hypertensive patients is related to insulin resistance. J Hypertens. 1997; 15(12 Pt 1): 1485-1491.
- 34Ogihara T, Asano T, Ando K, et al. High-salt diet enhances insulin signaling and induces insulin resistance in Dahl salt-sensitive rats. Hypertension. 2002; 40(1): 83-89.
- 35Chun YH, Han K, Kim DH, et al. Association of Urinary Sodium Excretion with insulin resistance in Korean adolescents: Results from the Korea National Health and Nutrition Examination Survey 2009-2010. Medicine (Baltimore). 2016; 95(17):e3447.
- 36Donovan DS, Solomon CG, Seely EW, Williams GH, Simonson DC. Effect of sodium intake on insulin sensitivity. Am J Phys. 1993; 264(5 Pt 1): E730-E734.
- 37Lopes KL, Furukawa LN, de Oliveira IB, Dolnikoff MS, Heimann JC. Perinatal salt restriction: a new pathway to programming adiposity indices in adult female Wistar rats. Life Sci. 2008; 82(13–14): 728-732.
- 38Fonseca-Alaniz MH, Takada J, Andreotti S, et al. High sodium intake enhances insulin-stimulated glucose uptake in rat epididymal adipose tissue. Obesity (Silver Spring). 2008; 16(6): 1186-1192.
- 39Prada P, Okamoto MM, Furukawa LN, Machado UF, Heimann JC, Dolnikoff MS. High- or low-salt diet from weaning to adulthood: effect on insulin sensitivity in Wistar rats. Hypertension. 2000; 35(1 Pt 2): 424-429.
- 40Okamoto MM, Sumida DH, Carvalho CR, et al. Changes in dietary sodium consumption modulate GLUT4 gene expression and early steps of insulin signaling. Am J Physiol Regul Integr Comp Physiol. 2004; 286(4): R779-R785.
- 41Prada PO, Coelho MS, Zecchin HG, et al. Low salt intake modulates insulin signaling, JNK activity and IRS-1ser307 phosphorylation in rat tissues. J Endocrinol. 2005; 185(3): 429-437. doi:10.1677/joe.1.06028
- 42Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2011; 9(11):Cd004022.
- 43Melander O, Groop L, Hulthén UL. Effect of salt on insulin sensitivity differs according to gender and degree of salt sensitivity. Hypertension. 2000; 35(3): 827-831.
- 44Oh H, Lee HY, Jun DW, Lee SM. Low salt diet and insulin resistance. Clin Nutr Res. 2016; 5(1): 1-6.
- 45Wu Q, Burley G, Li LC, Lin S, Shi YC. The role of dietary salt in metabolism and energy balance: insights beyond cardiovascular disease. Diabetes Obes Metab. 2023; 25(5): 1147-1161.
- 46Sierra-Ramos C, Velazquez-Garcia S, Vastola-Mascolo A, Hernández G, Faresse N, Alvarez de la Rosa D. SGK1 activation exacerbates diet-induced obesity, metabolic syndrome and hypertension. J Endocrinol. 2020; 244(1): 149-162.
- 47Mansley MK, Wilson SM. Effects of nominally selective inhibitors of the kinases PI3K, SGK1 and PKB on the insulin-dependent control of epithelial Na+ absorption. Br J Pharmacol. 2010; 161(3): 571-588.
- 48Dobrian AD, Schriver SD, Lynch T, Prewitt RL. Effect of salt on hypertension and oxidative stress in a rat model of diet-induced obesity. Am J Physiol Renal Physiol. 2003; 285(4): F619-F628.
- 49Fonseca-Alaniz MH, Brito LC, Borges-Silva CN, Takada J, Andreotti S, Lima FB. High dietary sodium intake increases white adipose tissue mass and plasma leptin in rats. Obesity (Silver Spring). 2007; 15(9): 2200-2208.
- 50Ghadge AA, Khaire AA. Leptin as a predictive marker for metabolic syndrome. Cytokine. 2019; 121:154735.
- 51Madeira I, Bordallo MA, Rodrigues NC, et al. Leptin as a predictor of metabolic syndrome in prepubertal children. Arch Endocrinol Metab. 2017; 61(1): 7-13. doi:10.1590/2359-3997000000199
- 52Mendoza-Herrera K, Florio AA, Moore M, et al. The leptin system and diet: a mini review of the current evidence. Front Endocrinol (Lausanne). 2021; 12:749050.
- 53Mancia G, Bousquet P, Elghozi JL, et al. The sympathetic nervous system and the metabolic syndrome. J Hypertens. 2007; 25(5): 909-920.
- 54Moreira MC, Pinto IS, Mourão AA, et al. Does the sympathetic nervous system contribute to the pathophysiology of metabolic syndrome? Front Physiol. 2015; 6:234. doi:10.3389/fphys.2015.00234
- 55Quarti Trevano F, Dell'Oro R, Biffi A, et al. Sympathetic overdrive in the metabolic syndrome: meta-analysis of published studies. J Hypertens. 2020; 38(4): 565-572.
- 56Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol. 2019; 15(6): 367-385.
- 57Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension: focus on the brain. Curr Opin Nephrol Hypertens. 2017; 26(2): 106-113.
- 58Putnam K, Shoemaker R, Yiannikouris F, Cassis LA. The renin-angiotensin system: a target of and contributor to dyslipidemias, altered glucose homeostasis, and hypertension of the metabolic syndrome. Am J Physiol Heart Circ Physiol. 2012; 302(6): H1219-H1230.
- 59Bitkin EC, Boyraz M, Taşkın N, et al. Effects of ACE inhibitors on insulin resistance and lipid profile in children with metabolic syndrome. J Clin Res Pediatr Endocrinol. 2013; 5(3): 164-169. doi:10.4274/Jcrpe.1020
- 60Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013; 36(8): 657-660.
- 61Nizar JM, Bhalla V. Molecular mechanisms of sodium-sensitive hypertension in the metabolic syndrome. Curr Hypertens Rep. 2017; 19(8): 60.
- 62Majid DS, Prieto MC, Navar LG. Salt-sensitive hypertension: perspectives on intrarenal mechanisms. Curr Hypertens Rev. 2015; 11(1): 38-48.
- 63Masenga SK, Kabwe LS, Chakulya M, Kirabo A. Mechanisms of oxidative stress in metabolic syndrome. Int J Mol Sci. 2023; 24(9):7898.
- 64Afsar B, Kuwabara M, Ortiz A, et al. Salt intake and immunity. Hypertension. 2018; 72(1): 19-23.
- 65Ertuglu LA, Mutchler AP, Yu J, Kirabo A. Inflammation and oxidative stress in salt sensitive hypertension; the role of the NLRP3 inflammasome. Front Physiol. 2022; 13:1096296.
- 66Ma Y, He FJ, MacGregor GA. High salt intake: independent risk factor for obesity? Hypertension. 2015; 66(4): 843-849.
- 67Lee SK, Kim MK. Relationship of sodium intake with obesity among Korean children and adolescents: Korea National Health and Nutrition Examination Survey. Br J Nutr. 2016; 115(5): 834-841.
- 68Lee J, Hwang Y, Kim KN, et al. Associations of urinary sodium levels with overweight and central obesity in a population with a sodium intake. BMC Nutr. 2018; 4: 47. doi:10.1186/s40795-018-0255-6
- 69Zhu H, Pollock NK, Kotak I, et al. Dietary sodium, adiposity, and inflammation in healthy adolescents. Pediatrics. 2014; 133(3): e635-e642.
- 70Lanaspa MA, Kuwabara M, Andres-Hernando A, et al. High salt intake causes leptin resistance and obesity in mice by stimulating endogenous fructose production and metabolism. Proc Natl Acad Sci USA. 2018; 115(12): 3138-3143.
- 71Grimes CA, Riddell LJ, Campbell KJ, Nowson CA. Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics. 2013; 131(1): 14-21.
- 72Larsen SC, Ängquist L, Sørensen TI, Heitmann BL. 24h urinary sodium excretion and subsequent change in weight, waist circumference and body composition. PLoS One. 2013; 8(7): e69689.
- 73Murakami K, Livingstone MB, Sasaki S, Uenishi K. Ability of self-reported estimates of dietary sodium, potassium and protein to detect an association with general and abdominal obesity: comparison with the estimates derived from 24 h urinary excretion. Br J Nutr. 2015; 113(8): 1308-1318.
- 74Li Q, Jin R, Yu H, et al. Enhancement of neural salty preference in obesity. Cell Physiol Biochem. 2017; 43(5): 1987-2000. doi:10.1159/000484122
- 75Bolhuis DP, Costanzo A, Newman LP, Keast RS. Salt promotes passive overconsumption of dietary fat in humans. J Nutr. 2016; 146(4): 838-845.
- 76Villatoro-Santos CR, Ramirez-Zea M, Villamor E. Urinary sodium, iodine, and volume in relation to metabolic syndrome in Mesoamerican children and their parents. Nutr Metab Cardiovasc Dis. 2022; 32(7): 1774-1783.
- 77Shen Y, Shi Y, Cui J, He H, Ren S. Effects of dietary salt intake restriction on blood glucose levels: a meta-analysis of crossover study. Nutr Res Pract. 2023; 17(3): 387-396.
- 78Patel SM, Cobb P, Saydah S, Zhang X, de Jesus JM, Cogswell ME. Dietary sodium reduction does not affect circulating glucose concentrations in fasting children or adults: findings from a systematic review and meta-analysis. J Nutr. 2015; 145(3): 505-513.
- 79Luther JM, Byrne LM, Yu C, Wang TJ, Brown NJ. Dietary sodium restriction decreases insulin secretion without affecting insulin sensitivity in humans. J Clin Endocrinol Metab. 2014; 99(10): E1895-E1902.
- 80Garg R, Williams GH, Hurwitz S, Brown NJ, Hopkins PN, Adler GK. Low-salt diet increases insulin resistance in healthy subjects. Metabolism. 2011; 60(7): 965-968.
- 81Ruivo GF, Leandro SM, do Nascimento CA, et al. Insulin resistance due to chronic salt restriction is corrected by alpha and beta blockade and by L-arginine. Physiol Behav. 2006; 88(4–5): 364-370. doi:10.1016/j.physbeh.2006.04.006
- 82Feng J, Lu S, Ou B, et al. The role of JNk signaling pathway in obesity-driven insulin resistance. Diabetes Metab Syndr Obes. 2020; 13: 1399-1406.
- 83Premilovac D, Richards SM, Rattigan S, Keske MA. A vascular mechanism for high-sodium-induced insulin resistance in rats. Diabetologia. 2014; 57(12): 2586-2595.
- 84Keske MA, Przewlocka-Kosmala M, Woznicka AK, et al. Role of skeletal muscle perfusion and insulin resistance in the effect of dietary sodium on heart function in overweight. ESC Heart Fail. 2021; 8(6): 5304-5315.
- 85Licht CM, de Geus EJ, Penninx BW. Dysregulation of the autonomic nervous system predicts the development of the metabolic syndrome. J Clin Endocrinol Metab. 2013; 98(6): 2484-2493.
- 86González SA, Forcada P, de Cavanagh EM, et al. Sodium intake is associated with parasympathetic tone and metabolic parameters in mild hypertension. Am J Hypertens. 2012; 25(5): 620-624. doi:10.1038/ajh.2012.10
- 87Fliser D, Nowack R, Allendorf-Ostwald N, Kohl B, Hübinger A, Ritz E. Serum lipid changes on low salt diet. Effects of alpha 1-adrenergic blockade. Am J Hypertens. 1993; 6(4): 320-324.
- 88Harsha DW, Sacks FM, Obarzanek E, et al. Effect of dietary sodium intake on blood lipids: results from the DASH-sodium trial. Hypertension. 2004; 43(2): 393-398. doi:10.1161/01.HYP.0000113046.83819.a2
- 89Krikken JA, Dallinga-Thie GM, Navis G, Dullaart RP. Short term dietary sodium restriction decreases HDL cholesterol, apolipoprotein A-I and high molecular weight adiponectin in healthy young men: relationships with renal hemodynamics and RAAS activation. Nutr Metab Cardiovasc Dis. 2012; 22(1): 35-41.
- 90Choi JW, Park JS, Lee CH. Interactive effect of high sodium intake with increased serum triglycerides on hypertension. PLoS One. 2020; 15(4):e0231707.
- 91Hirano T, Ebara T, Furukawa S, Nagano S, Takahashi T. Mechanism of hypertriglyceridemia in Dahl salt-sensitive rats, an animal model of spontaneous nephrotic syndrome. Metabolism. 1994; 43(2): 248-256.
- 92Kang YJ, Wang HW, Cheon SY, Lee HJ, Hwang KM, Yoon HS. Associations of obesity and dyslipidemia with intake of sodium, fat, and sugar among Koreans: a qualitative systematic review. Clin Nutr Res. 2016; 5(4): 290-304.
- 93Campino C, Baudrand R, Valdivia CA, et al. Sodium intake is associated with endothelial damage biomarkers and metabolic dysregulation. Am J Hypertens. 2018; 31(10): 1127-1132. doi:10.1093/ajh/hpy097
- 94Cavalcante KVN, Ferreira-Junior MD, Moreira M, et al. Skinny fat model of metabolic syndrome induced by a high-salt/sucrose diet in young male rats. Br J Nutr. 2025; 133(2): 171-181. doi:10.1017/S0007114524002927
- 95Lee M, Sorn SR, Lee Y, Kang I. Salt induces adipogenesis/lipogenesis and Inflammatory adipocytokines secretion in adipocytes. Int J Mol Sci. 2019; 20(1): 160.
- 96Lanaspa MA, Ishimoto T, Li N, et al. Endogenous fructose production and metabolism in the liver contributes to the development of metabolic syndrome. Nat Commun. 2013; 4: 2434.
- 97Frieler RA, Vigil TM, Song J, Leung C, Lumeng CN, Mortensen RM. High-fat and high-sodium diet induces metabolic dysfunction in the absence of obesity. Obesity (Silver Spring). 2021; 29(11): 1868-1881.
- 98Uetake Y, Ikeda H, Irie R, et al. High-salt in addition to high-fat diet may enhance inflammation and fibrosis in liver steatosis induced by oxidative stress and dyslipidemia in mice. Lipids Health Dis. 2015; 14: 6.
- 99Cogswell ME, Mugavero K, Bowman BA, Frieden TR. Dietary sodium and cardiovascular disease risk—measurement matters. N Engl J Med. 2016; 375(6): 580-586.
- 100McLean RM, Farmer VL, Nettleton A, Cameron CM, Cook NR, Campbell NRC. Assessment of dietary sodium intake using a food frequency questionnaire and 24-hour urinary sodium excretion: a systematic literature review. J Clin Hypertens (Greenwich). 2017; 19(12): 1214-1230.
- 101Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014; 36:e2014009.
- 102Bentley B. A review of methods to measure dietary sodium intake. J Cardiovasc Nurs. 2006; 21(1): 63-67.
- 103Ortega RM, Pérez-Rodrigo C, López-Sobaler AM. Dietary assessment methods: dietary records. Nutr Hosp. 2015; 31(Suppl 3): 38-45.
- 104Cobb LK, Anderson CA, Elliott P, et al. Methodological issues in cohort studies that relate sodium intake to cardiovascular disease outcomes: a science advisory from the American Heart Association. Circulation. 2014; 129(10): 1173-1186. doi:10.1161/CIR.0000000000000015
- 105Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014; 371(7): 624-634.
- 106Tao J, Quan J, El Helali A, Lam WWT, Pang H. Global trends indicate increasing consumption of dietary sodium and fiber in middle-income countries: a study of 30-year global macrotrends. Nutr Res. 2023; 118: 63-69.
- 107Santos JA, Tekle D, Rosewarne E, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutr. 2021; 12(5): 1768-1780.
- 108Chen X, Du J, Wu X, Cao W, Sun S. Global burden attributable to high sodium intake from 1990 to 2019. Nutr Metab Cardiovasc Dis. 2021; 31(12): 3314-3321.
- 109Hall JJ, Eurich DT, Nagy D, Tjosvold L, Gamble JM. Thiazide diuretic-induced change in fasting plasma glucose: a meta-analysis of randomized clinical trials. J Gen Intern Med. 2020; 35(6): 1849-1860.
- 110Reungjui S, Roncal CA, Mu W, et al. Thiazide diuretics exacerbate fructose-induced metabolic syndrome. J Am Soc Nephrol. 2007; 18(10): 2724-2731.
- 111Sandsdal RM, Juhl CR, Jensen SBK, et al. Combination of exercise and GLP-1 receptor agonist treatment reduces severity of metabolic syndrome, abdominal obesity, and inflammation: a randomized controlled trial. Cardiovasc Diabetol. 2023; 22(1): 41. doi:10.1186/s12933-023-01765-z
- 112Chatterjee S, Ghosal S, Chatterjee S. Glucagon-like peptide-1 receptor agonists favorably address all components of metabolic syndrome. World J Diabetes. 2016; 7(18): 441-448.
- 113Kim M, Platt MJ, Shibasaki T, et al. GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure. Nat Med. 2013; 19(5): 567-575.
- 114Skov J, Holst JJ, Gøtze JP, Frøkiær J, Christiansen JS. Glucagon-like peptide-1: effect on pro-atrial natriuretic peptide in healthy males. Endocr Connect. 2014; 3(1): 11-16.
- 115Crajoinas RO, Oricchio FT, Pessoa TD, et al. Mechanisms mediating the diuretic and natriuretic actions of the incretin hormone glucagon-like peptide-1. Am J Physiol Renal Physiol. 2011; 301(2): F355-F363.
- 116Wilcox CS. Antihypertensive and renal mechanisms of SGLT2 (sodium-glucose linked transporter 2) inhibitors. Hypertension. 2020; 75(4): 894-901.
- 117Yamamoto C, Miyoshi H, Ono K, et al. Ipragliflozin effectively reduced visceral fat in Japanese patients with type 2 diabetes under adequate diet therapy. Endocr J. 2016; 63(6): 589-596.
- 118Ferrannini E, Baldi S, Frascerra S, et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes. 2016; 65(5): 1190-1195.
- 119Xu L, Ota T. Emerging roles of SGLT2 inhibitors in obesity and insulin resistance: focus on fat browning and macrophage polarization. Adipocytes. 2018; 7(2): 121-128.
- 120Cheng L, Fu Q, Zhou L, et al. Dapagliflozin, metformin, monotherapy or both in patients with metabolic syndrome. Sci Rep. 2021; 11(1): 24263.
- 121González-Ortiz M, Méndez-Del Villar M, Martínez-Abundis E, Ramírez-Rodríguez AM. Effect of dapagliflozin administration on metabolic syndrome, insulin sensitivity, and insulin secretion. Minerva Endocrinol. 2018; 43(3): 229-235.
- 122 Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III). JAMA. 2001; 285(19): 2486-2497.
- 123Matsuzawa Y. Metabolic syndrome—definition and diagnostic criteria in Japan. J Atheroscler Thromb. 2005; 12(6): 301.
- 124Kim HM, Kim DJ, Jung IH, Park C, Park J. Prevalence of the metabolic syndrome among Korean adults using the new International Diabetes Federation definition and the new abdominal obesity criteria for the Korean people. Diabetes Res Clin Pract. 2007; 77(1): 99-106.
- 125Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006; 23(5): 469-480.
- 126Oh HY, Kim MK, Lee M, Kim YO. Macronutrient composition and sodium intake of diet are associated with risk of metabolic syndrome and hypertension in Korean women. PLoS One. 2013; 8(10):e78088.
- 127Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120(16): 1640-1645. doi:10.1161/CIRCULATIONAHA.109.192644
- 128Kimura T, Hashimoto Y, Tanaka M, et al. Sodium-chloride difference and metabolic syndrome: a population-based large-scale cohort study. Intern Med. 2016; 55(21): 3085-3090.
- 129Lee SY, Park HS, Kim DJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75(1): 72-80.
- 130Li X, Guo B, Jin D, et al. Association of dietary sodium:potassium ratio with the metabolic syndrome in Chinese adults. Br J Nutr. 2018; 120(6): 612-618.
- 131Naser AM, Rahman M, Unicomb L, et al. Past sodium intake, contemporary sodium intake, and cardiometabolic health in southwest coastal Bangladesh. J Am Heart Assoc. 2020; 9(18):e014978.
- 132Baek SY, Kim HK. Association of dietary sodium-to-potassium ratio with cardiometabolic risk factors in Korean adults: findings from the Korean National Health and Nutrition Examination Survey. Nutrients. 2023; 15(14):3134.
- 133Choi B, Kim J, Kim Y, Shin J, Lee SA. Calcium- and sodium-rich food intake among Koreans with and without metabolic syndrome: cross-sectional analysis of the Korean genome and epidemiology study. Nutrients. 2024; 16(15):2439.