Health-related quality of life is dynamic in alcoholic hepatitis and responds to improvement in liver disease and reduced alcohol consumption
Funding information
APD is funded by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number K23 DK123408. Collection of serum samples and analysis was funded by the National Institutes on Alcohol Abuse and Alcoholism award number U01 AA021840-07S1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the funder: The funder was not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Abstract
Background
The impact of alcoholic hepatitis (AH) on health-related quality of life (HRQOL) remains inadequately described. We aimed to characterize HRQOL in AH and heavy drinkers (HD), and its associations with clinical variables and outcomes.
Methods
This is a post hoc analysis of participants in the Translational Research and Evolving Alcoholic Hepatitis Treatment 001 study (NCT02172898). HRQOL was measured using Short Form Health Survey (SF-36). Mean SF-36 scores were compared in AH and HD with two-sample t-tests. Associations among clinical characteristics, 30-day mortality, and SF-36 mental and physical component scores (MC, PC) were investigated with generalized linear and logistic multivariate regression models. Trends of MC and PC scores were analyzed using one-way ANOVA.
Results
Participants with AH (n = 258) and HD (n = 181) were similar demographically. AH cases had a mean Model for End-stage Liver Disease (MELD) score of 23 (7). AH cases had lower PC scores [37 (10) vs. 48 (11), p < 0.001] but higher MC scores [37 (13) vs. 32 (13), p < 0.001]. MC scores were independently associated with age, male gender, and daily alcohol consumption; PC scores were independently associated with age, BMI, alanine aminotransferase concentration, alkaline phosphatase concentration, white blood cell counts, and the presence of ascites. With each 5-point decrease in the baseline PC score, the adjusted odds of dying within 30 days increased by 26.7% (95% CI 1% to 46%). Over time, HRQOL in AH improved (day 0 to day 180 delta PC score: 4.5 ± 1.7, p = 0.008; delta MC score: 9.8 ± 2.0, p < 0.001). Participants with a MELD score <15 by day 180 had greater increases in PC scores than those with MELD score ≥15 (delta PC score 7.1 ± 1.8 vs. −0.7 ± 2.3, p = 0.009), while those abstinent by day 180 had greater increases in MC scores than those who were not abstinent (delta MC score 9.1 ± 1.8 vs. 2.8 ± 2.4, p = 0.044).
Conclusions
HRQOL is poor in AH and HD in a domain-specific pattern. Independent of MELD score, lower baseline HRQOL is associated with higher 30-day mortality. Over time, HRQOL improves with greater gains seen in individuals with improved MELD scores and those who were abstinent.
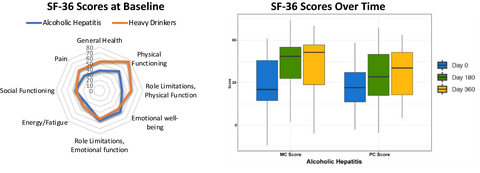
Graphical Abstract
We measured health related quality of life (HRQOL) in alcoholic hepatitis and heavy drinkers using the Short Form Health Survey (SF-36). We show that mental component (MC) scores were associated with demographic characteristics while physical component (PC) scores were associated with liver disease parameters. Over 1-year, HRQOL improved in alcoholic hepatitis; PC scores increased with improved MELD and MC scores increased with abstinence. There were larger increases in both PC and MC scores with resolution of ascites and hepatic encephalopathy.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest. For full disclosure, Dr. Naga Chalasani has ongoing paid consulting activities (or had in the preceding 12 months) with NuSirt, Abbvie, Afimmune (DS Biopharma), Allergan (Tobira), Madrigal, Siemens, Foresite, Galectin, Zydus, and La Jolla. These consulting activities are generally in the areas of nonalcoholic fatty liver disease and drug hepatotoxicity. Dr. Chalasani receives research grant support from Exact Sciences, Intercept, and Galectin Therapeutics, where his institution receives the funding. Over the last decade, Dr. Chalasani has served as a paid consultant to more than 35 pharmaceutical companies, and these outside activities have regularly been disclosed to his institutional authorities. Remaining authors have no disclosures to report.