Influence of Initial Treatment Strategy on Outcomes for Children With Rectal Prolapse
The authors report no conflicts of interest.
Data Access: All data supporting this study are included within the article and/or supporting materials
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
Abstract
Objective:
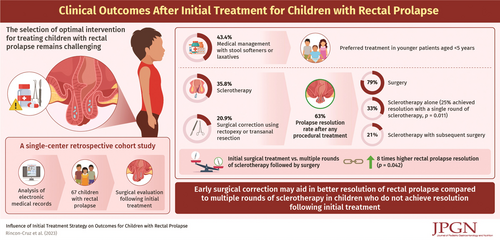
Pediatric rectal prolapse is a common and often self-limited condition with multiple management options. Selecting the optimal approach requires personalization and remains a challenge for pediatricians and pediatric surgeons.
Methods:
A single-center retrospective review of 67 children with rectal prolapse undergoing surgical evaluation between 2010 and 2021. Patients with anorectal malformations, Hirschsprung disease, inflammatory bowel disease, and cystic fibrosis were excluded. We used multivariable logistic regression to compare medical management, sclerotherapy, and surgical correction (rectopexy or transanal resection) as initial treatment strategies, with a primary endpoint of prolapse resolution.
Results:
Younger patients (<5 years) were more likely to be initially treated with medical management alone (P < 0.001). Patients with a psychiatric diagnosis were more likely to be offered either sclerotherapy or surgery upfront (P = 0.009). The resolution rate with surgery as initial management was 79% (n = 11/14). The resolution rate with sclerotherapy as initial management was 54% (n = 13/24), with 33% (n = 8/24) resolving with sclerotherapy alone and 21% (n = 5/24) resolving after a subsequent surgical procedure (P = 0.011). Patients who underwent initial surgical management had an adjusted odds ratio of 8.0 (95% CI: 1.1–59.1; P = 0.042) for resolution of prolapse compared to patients who underwent sclerotherapy initially. Markers of severity (bleeding, need for manual reduction) were not associated with initial therapy offered (P = 0.064).
Conclusions:
Surgical intervention (sclerotherapy, rectopexy, transanal resection) resolved rectal prolapse in most children (63%). Surgery as an initial management approach had a significantly higher success rate than sclerotherapy, even after controlling for severity of disease, psychiatric diagnosis, need for manual reduction, and age.