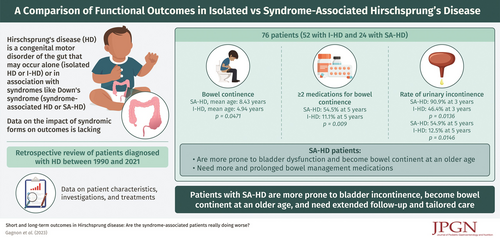
Short and Long-Term Outcomes in Hirschsprung Disease: Are the Syndrome-Associated Patients Really Doing Worse?
The authors report no conflicts of interest.
This article has been developed as a Journal CME and MOC Part II Activity by NASPGHAN. Visit https://learnonline.naspghan.org/ to view instructions, documentation, and the complete necessary steps to receive CME and MOC credits for reading this article.
Abstract
Introduction:
Given the lack of data to help caregivers in the follow-up of Hirschsprung disease (HD), this study aimed to compare the functional outcomes of isolated Hirschsprung disease (I-HD) to syndrome-associated Hirschsprung disease (SA-HD) at 1, 3, 5, and 10 years.
Methods:
A retrospective chart review of patients diagnosed with HD between January 1990 and May 2021 at our pediatric center was performed to collect data on patient characteristics, investigations, and treatments. Ninety-five patients were identified, of whom 76 were included in the study. SA-HD is defined as a syndrome known to be associated with HD or cognitive impairment.
Results:
Patient characteristics were comparable between groups (P > 0.05). There were 52 patients with I-HD and 24 with SA-HD. The patients median age was 9 days at diagnosis and 1.5 month at surgery. SA-HD patients became bowel continent at a significantly older age (mean age 8.43 vs 4.94 years, P = 0.0471) and received more bowel continence medications. At 5 years, SA-HD patients requiring ≥2 medications for bowel continence represented 54.5% versus 11.1% of I-HD patients (P = 0.009). Lastly, SA-HD patients had urinary incontinence at a significantly older age (P = 0.0136, 5 years).
Conclusion:
Clinicians should be aware that SA-HD patients are more prone to bladder dysfunction and became bowel continent at an older age than I-HD patients. They need more and prolonged bowel management medications, and other important complications need to be addressed in patient care. These results should prompt a longer follow-up period for these patients, especially in SA-HD.