Endomyocardial biopsy in pediatric heart transplant recipients: A useful exercise? (Analysis of 1169 biopsies)
Abstract
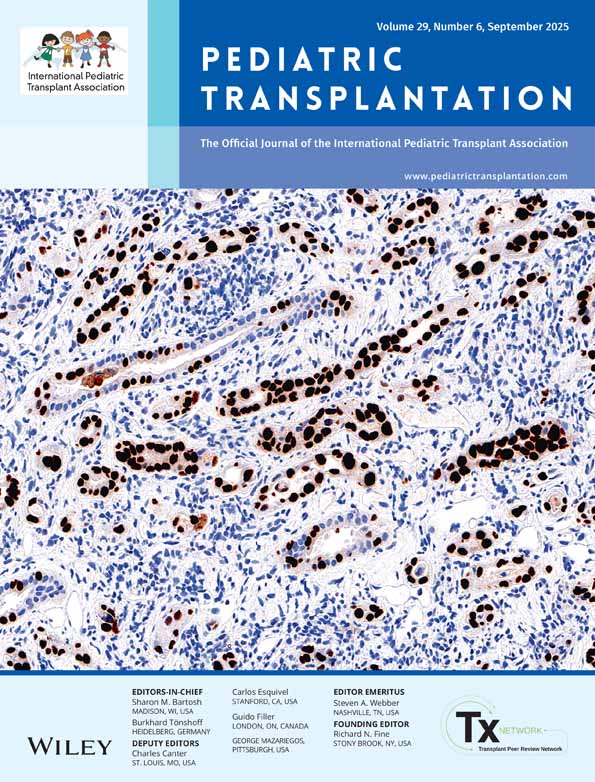
Abstract: The objective of this study was to define the diagnostic yield for endomyocardial biopsy (EMB) procedures performed for various indications in a large pediatric heart transplant population. Endomyocardial biopsy procedure has been employed as the ‘gold standard’ for rejection surveillance. Previous studies have questioned the value of surveillance EMB beyond the early post-transplant period. We retrospectively reviewed data on 82 pediatric heart transplant recipients with serial EMB. A total of 1169 EMB were performed during a follow-up period of 2–149 months (median 41 months). EMB were classified by age at transplantation, time from transplant, immunosuppressive regimen used [tacrolimus vs. cyclosporin A (CsA)] and indication, i.e. surveillance, follow-up after rejection or lowering of immunosuppression, non-specific clinical symptoms and graft dysfunction. During the first year after heart transplantation, surveillance EMB demonstrated significant rejection [International Society for Heart and Lung Transplantation (ISHLT) grade ≥ 3A] in 18% of biopsies with the yield being 14–43% for all other indications. Surveillance EMB 1–5 yr post-transplantation were found to have a lower diagnostic yield in infants (4% vs. 13% in children) and in patients with favorable first-year rejection history (9% vs. 17% in ‘frequent rejectors’). Tacrolimus-based immunosuppression was associated with significantly less rejection, but only in the first year post-transplantation (14% in tacrolimus vs. 24% in CsA surveillance EMB, p = 0.035). Surveillance EMB remains an important diagnostic tool for rejection surveillance during the first 5 years after pediatric heart transplantation. Endomyocardial biopsy is particularly warranted after reduction of immunosuppression and for monitoring for ongoing rejection after treatment of acute rejection episodes.