Latissimus dorsi myocutaneous free flap for post-sacrectomy reconstruction: Outcomes compared with gluteal muscle flap
Abstract
Background
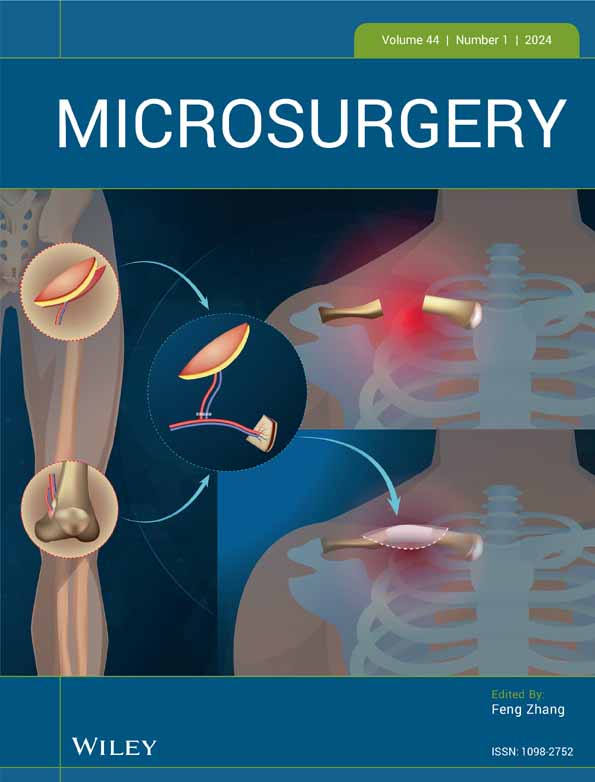
Excision of sacral tumor results in extensive defects and vital organ exposure, requiring soft tissue reconstruction for dead space obliteration. Diverse reconstruction options, mainly regional flaps, have been utilized but are limited by high postoperative morbidity. A reliable reconstructive method with low morbidity and facilitated recovery has yet been sought for. In this study, we aimed to evaluate the use of free latissimus dorsi (LD) flap for post-sacrectomy defect reconstruction by comparing its outcomes with local gluteus maximus (GM) flap.
Methods
A retrospective review was conducted of all patients with sacral malignancy who underwent partial or total sacrectomy and immediate reconstruction with LD or GM flap between 2013 and 2022. Nineteen patients were analyzed, including 10 GM flaps and nine LD flaps. Postoperative outcomes were compared between the two groups.
Results
The average size of LD flaps was 173.8 cm2. Seven patients developed complication in the GM group and two patients in the LD group. Complication rate at sacrectomy site was lower in the LD group (p = .003) showing complication-free sacrectomy site and two donor site seromas. The LD group resulted in shorter hospital stay (p = .033) and earlier ambulation than the GM group (p = .001). Mean follow-up period was 63 months for GM group and 17 months for LD group. Three patients in the GM group underwent re-operation, while no delayed complication was observed in the LD group.
Conclusion
Free LD flaps may provide reliable outcomes with early recovery and may be considered an effective option for sacrectomy defect reconstruction.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.