Concurrent management of lymphedema and breast reconstruction with single-stage omental vascularized lymph node transfer and autologous breast reconstruction: A case series
Abstract
Introduction
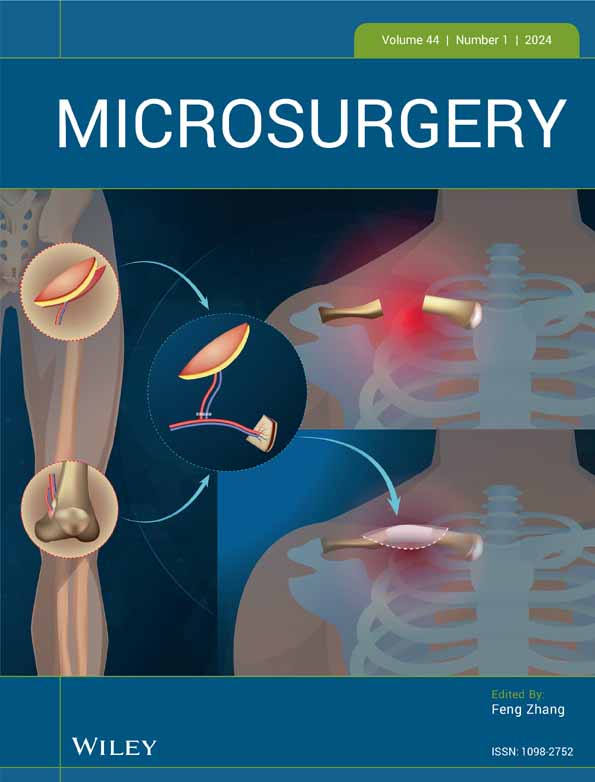
The omentum has gained recent popularity in vascularized lymph node transfers (VLNT) as well as its novel use as a free flap for autologous breast reconstruction. The omentum has multiple unique advantages. It can be harvested laparoscopically or in an open fashion when utilized with abdominally-based free flaps. Additionally, it can be split into multiple flaps for simultaneous autologous breast reconstruction with VLNT or for multiple sites of VLNT. We present the safe and advantageous use of the omentum for VLNT with simultaneous autologous breast reconstruction in a series of patients.
Methods
From the years 2019–2022, patients who underwent breast reconstruction with deep inferior epigastric artery perforator (DIEP) or muscle sparing tram (MS-TRAM) flaps with concurrent omental VLNT through a mini-laparotomy or breast reconstruction with Omental Fat-Augmented Free Flap (O-FAFF) with concurrent laparoscopic harvesting of omental VLNT were studied. Patient demographics included age, gender, comorbidities, prior radiation or chemotherapy, body mass index, complications, hospital length of stay, and surgical outcomes.
Results
A total of seven patients underwent omental VLNT with breast reconstruction for a total of 12 breasts and eight limbs treated. Three of the patients underwent autologous breast reconstruction using omental free flap. The mean age was 52.3 (range 40–75) years and mean body mass index (BMI) was 29.3 (range 23–38) kg/m2. The flap survival rate was 100%. All the patients had successful reduction of extremity circumference and improvement of symptoms. The range of follow-up was 5 to 19 months, with an average follow-up of 14.6 months. There was only one complication among our 7 patients: a patient with a BMI of 38 developed a post-surgical abdominal wound treated with local wound care. Otherwise, post-operative courses were uneventful, and no further complications were reported.
Conclusion
We demonstrate here additional evidence to the growing body of literature of the versatility and safety of the omentum to be utilized as an independent tool for surgical treatment of lymphedema as well as its simultaneous use with autologous breast reconstruction.
CONFLICT OF INTEREST STATEMENT
None.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.