Prognostic value of p16-INK4A protein in women with negative or CIN1 histology result: A follow-up study
Novelty and impact: P16 overexpression has been proposed as a prognostic marker for CIN progression, but a few prospective studies tested the prognostic value of histological p16 in post-colposcopy follow up. In a 2 years cohort study, we found low prognostic sensitivity for CIN2+ (6/13), but a 5.5 relative risk (95% CI 1.7–17.4) for women p16 positive at baseline compared to negative. P16 overexpression is a good candidate for modulating follow up intensity after a negative colposcopy.
Conflicts of interest: PGR is the principal investigator of a project sponsored by the Italian Ministri of Health and data owner. For this project, PGR in contact with ROCHE DIAGNOSTICS, HOLOGIC-GEN Probe, QUIAGEN, for tests at reduced price or free of cost. All other authors have no conflicts of interest
Abstract
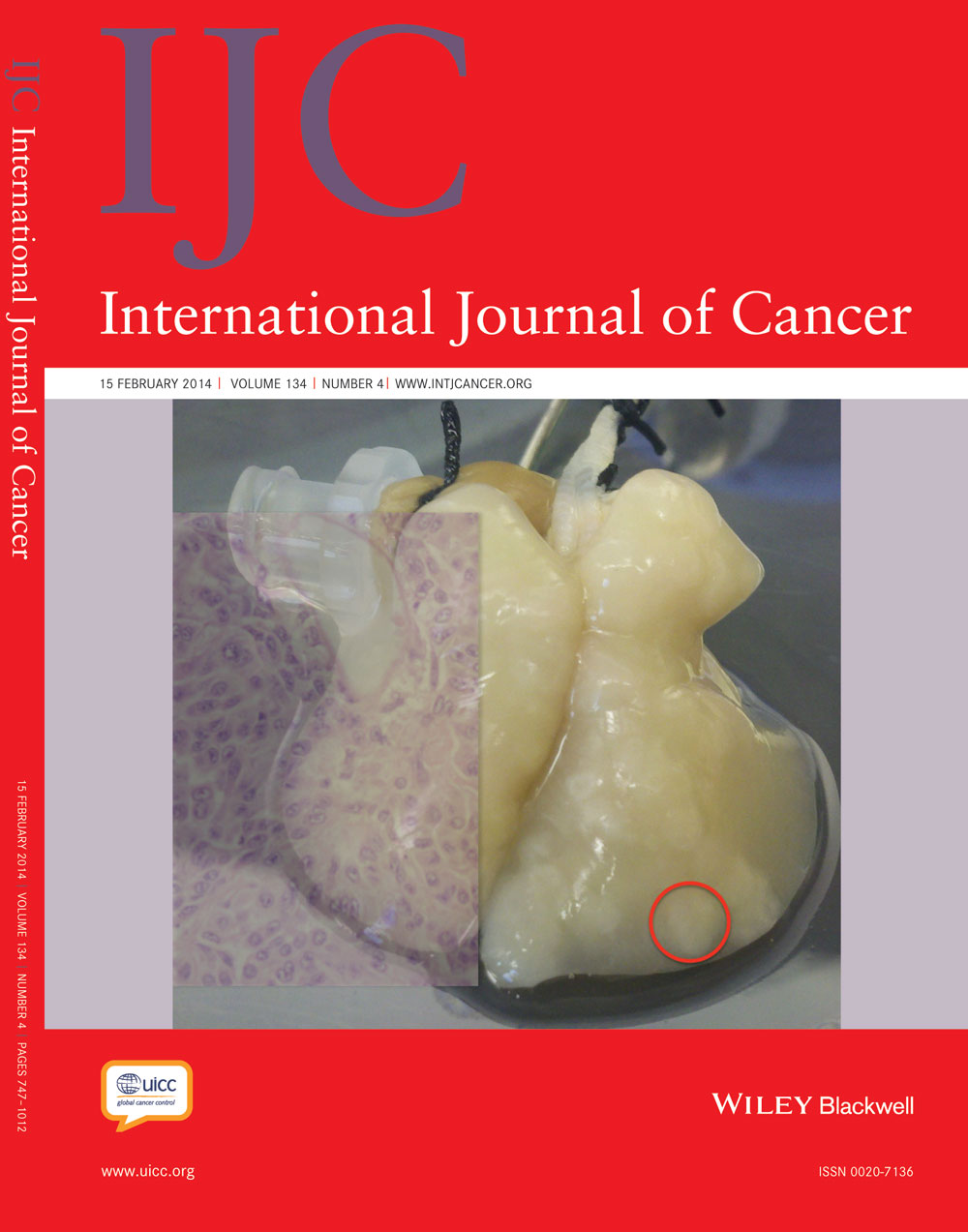
P16-INK4A overexpression has been proposed as a prognostic marker to manage the follow up of women with positive cytology and/or HPV test but without high-grade cervical intraepithelial neoplasia (CIN2+). This study measures the relative risk (RR) of CIN2+ of p16 positive versus negative in these women. All the women referred to colposcopy from October 2008 to September 2010 with negative or CIN1 colposcopy-guided biopsy were included in the study; women surgically treated or having a CIN2–3 were excluded. All baseline biopsies were dyed with hematoxylin and eosin and p16. Women were followed up according to screening protocols, with cytology or colposcopy at 6 or 12 months. CIN2/3 RRs and 95% confidence intervals (95%CI) were computed. Of 442 eligible women, 369 (83.5%) had at least one follow-up episode. At baseline, 113 (30.6%) were CIN1, 248 (67.2%) negative, and 8 (2.2%) inadequate histology; 293 (79.4%) were p16-negative, 64 (17.3%) p16 positive and 12 (3.2%) not valid. During follow up, we found ten CIN2 and three CIN3; of these, six were p16 positive (sensitivity 46%, 95% CI 19–75). The absolute risk among p16 positives was 9.4/100 compared to 1.7/100 of the p16 negatives (RR 5.5; 95% CI 1.7–17.4). The risk was also higher for CIN1 than for histologically negative women (RR 4.4; 95% CI 1.3–14.3). The RR for p16 in CIN1 did not change (RR 5.2; 95% CI 0.6–47.5). P16 overexpression is a good candidate for modulating follow-up intensity after a negative colposcopy but is limited by its low prospective sensitivity.
Abstract
What's new?
Women with low-grade cervical intraepithelial neoplasia 1 (CIN1) detected by positive Pap smear but accompanied by negative colposcopic biopsy present unique challenges for follow-up, especially since CIN1 is known to often regress. The situation could be helped in part through the use of a biomarker for CIN1 progression, such as p16 overexpression. This study shows that p16 has low prognostic sensitivity for patients with CIN2+ (CIN2 or worse) but is associated with elevated risk for these advanced conditions. The data suggest that p16 overexpression may be useful in evaluating the intensity of follow-up needed after a negative colposcopy.