Transcatheter aortic valve replacement-related aortic dissection: A clinical case series
Abstract
Objectives
We review our experience with 13 periprocedural aortic dissection (AD) cases caused by transcatheter aortic valve replacement (TAVR).
Background
AD is a potentially lethal complication of TAVR; however, only sporadic case reports have been published to date.
Methods
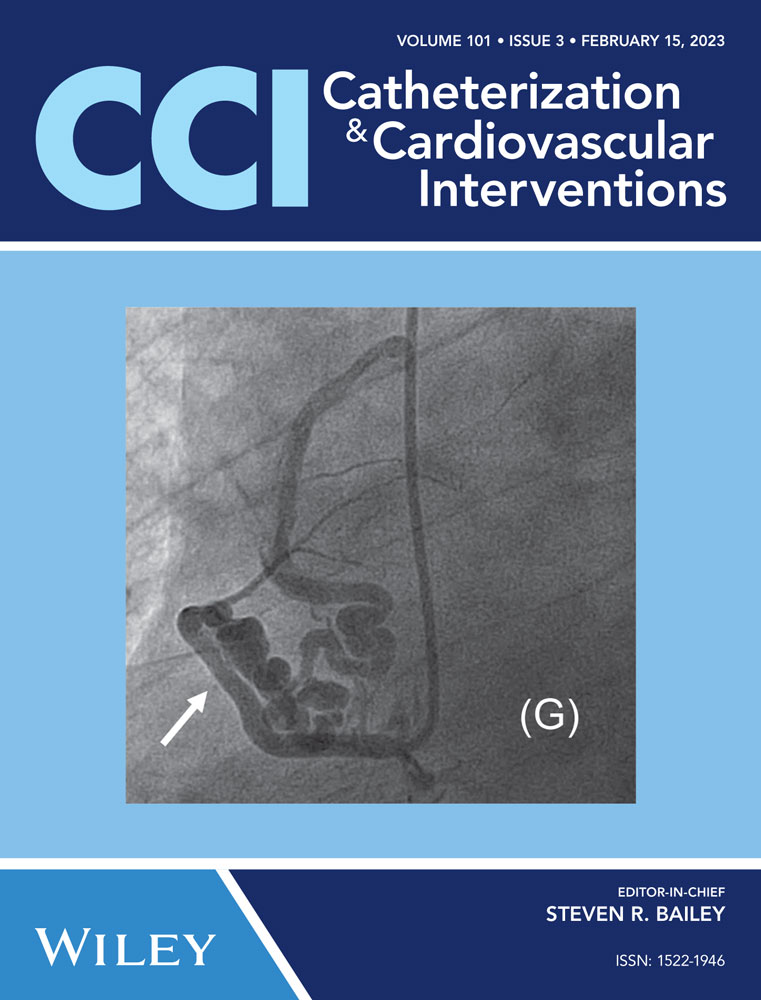
Among 1335 consecutive patients who underwent TAVR in 2013–2021, we retrospectively extracted 13 patients (1.0%) with TAVR-related AD (Stanford type A in 6 [46%], type B in 7 [54%]). AD was defined as a new-onset dissected layer of the aortic wall and diagnosed by aortography, computed tomography, or transesophageal echocardiography.
Results
Five of the six type A AD cases (83%) were detected during TAVR versus only one of the seven type B AD cases (14%). Four of the seven type B AD cases (57%) were asymptomatic and incidentally detected on computed tomography. The presumed causes of AD were injury by the delivery sheath (39%), delivery catheter (23%), valve implantation (15%), stent edge (15%), and pre-dilation balloon (8%). Complicated AD occurred in only one patient (8%). Considering the patient's age and prohibitive surgical risk, all patients were treated conservatively and free of any aortic-related deaths or interventions during a follow-up of 1087 days.
Conclusions
TAVR-related AD is a rare but life-threatening condition that may be underdiagnosed. Its optimal therapy remains unclear, and conservative management might be an option for selected patients. Further studies are needed to elucidate the incidence, risk factors, effective screening, optimal therapy, and outcomes of TAVR-related AD.
Open Research
DATA AVAILABILITY STATEMENT
Data cannot be made publicly available for ethical reasons, for example, public availability would compromise patient confidentiality.