The Potential of Food Protein-Derived Bioactive Peptides against Chronic Intestinal Inflammation
Abstract
Inflammation can cause various chronic diseases like inflammatory bowel diseases. Various food protein-derived bioactive peptides (BAPs) with anti-inflammatory activity have the potential to manage these diseases. The aim of this paper is to overview the mechanisms and the molecular targets of BAPs to exert anti-inflammatory activity. In this review, the in vitro and in vivo effects of BAPs on intestinal inflammation are highlighted. The mechanism, pathways, and future perspectives of BAPs as the potential sources of therapeutic treatments to alleviate intestinal inflammation are provided, including nuclear factor-κB, mitogen-activated protein kinase, Janus kinase-signal transducer and activator of transcription, and peptide transporter 1 (PepT1), finding that PepT1 and gut microbiota are the promising targets for BAPs to alleviate the intestinal inflammation. This review provides a comprehensive understanding of the role of dietary BAPs in attenuating inflammation and gives a novel direction in nutraceuticals for people or animals with intestinal inflammation.
1. Introduction
Inflammation is a normal immune defense that is generated from the immune system responding to pathogen and infection. Inflammation can cause various chronic diseases, such as inflammatory bowel diseases (IBD), asthma, cancer, cardiovascular diseases, obesity, and diabetes [1]. The intestinal mucosa can be damaged by IBD with chronic inflammatory disorders, including ulcerative colitis (UC) and Crohn’s disease (CD). UC is an inflammation of the colon mucosa and submucosa continuity affecting the rectal area, while CD is a full-thickness inflammation discontinuity affecting the terminal ileum and colon or anus [2]. Until now, the aetiology of intestinal inflammation and IBD remains unclear.
In the intestines of human and animals, dietary proteins are digested into free amino acids and peptides by enzymatic hydrolysis. Some peptides consisting of 2–20 AAs with biological function are named bioactive peptides (BAPs), such as anti-inflammation, antihypertension, antioxidation, antidiabetics, anticancer, antimicrobics, antiadhesion, dipeptidyl peptidase IV inhibition, opioid, and immunomodulation [3]. Conventional drug treatments have adverse side effects, such as potential toxicity and immunogenicity [4]. In recent years, BAPs have attracted more and more attention to treat chronic inflammation diseases as a result of their safety [1, 5].
However, limited information of the anti-inflammatory mechanisms of the action of these BAPs is available. In this review, food protein-derived BAPs against intestinal inflammation in vitro and in vivo are discussed. Their molecular targets and the action pathways are overviewed and highlighted. Understanding of the anti-inflammatory actions of BAPs can facilitate further research on managing chronic intestinal inflammation and diseases. Therefore, the purpose of this paper is to highlight the roles of BAPs in anti-inflammatory activity and provide future perspectives for the application of BAPs as potential sources of therapeutic management of chronic intestinal diseases.
2. Intestinal Inflammation
Inflammation can activate protective proinflammatory mediators, such as interleukin- (IL-) 1, IL-6, IL-8, IL-12, interferon-γ (INF-γ), and tumor necrosis factor-α (TNF-α) in immune responses, which include T and B lymphocytes. The activated B lymphocytes can produce antibodies, such as IgA, IgG, IgM, and IgE. The T lymphocyte cells consist of CD4+ and CD8+ T cells. CD4+ T cells, named helper T lymphocytes (Th), have immune regulatory function by secreting cytokines, being classified into Th1 and Th2. Th1 can release IL-2, IFN-γ, and TNF-α to promote cellular immunological response, whereas Th2 can release IL-4 and IL-10 to improve immunoresponse, while CD8+ T cells have the function to kill the target cells [6].
Progression of inflammation has four steps: inducers, pathways, mediators, and inflammatory response [7]. The inducers (LPS, dextran sodium sulfate (DSS), 2,4,6-trinitrobenzene sulfonic acid (TNBS), or toxicant) stimulate the sensors that can activate pathways, including nuclear factor-κB (NF-κB) and mitogen-activated protein kinase (MAPK). Then, inflammatory mediators (IL-8, TNF-α, monocyte chemoattractant protein-1 (MCP-1), or reactive oxygen species (ROS)) are released, leading to the inflammatory response [7]. Proinflammatory cytokines produced mainly by macrophages and mast cells lead to inflammation, while anti-inflammatory cytokines, such as IL-4, IL-10, and transforming growth factor β (TGF-β), reduce the production of procytokines in macrophage cells as agonists of toll-like receptor [7]. In in vivo studies, TNBS and DSS are commonly used to induce intestinal inflammation in animal models, causing immune alterations, gut physiology and morphology changes, and colitis symptoms [8]. Moreover, administration of DSS can lead to higher intraluminal IgG [9]. In UC patients, IgG production is dramatically high in the gut; therefore, IgG is an index to grade IBD. Thus, these cytokines with pathology may be the targets for BAPs to prevent chronic inflammation. In addition, it is also known that oxidative stress is associated with chronic intestinal inflammation, and it can decrease antioxidant defenses in the colonic mucosa. Additionally, ROS are released from immune cells and can be overwhelmed by oxidative stress. Therefore, antioxidative BAPs are the candidates for antioxidant defense in inflammatory gut [10], such as IRW [11], IQW [12], EAMAPK, and AVPYPQ [13]. Soybean-derived lunasin can also enhance antioxidant defenses and inhibit inflammation [14, 15].
3. Anti-Inflammatory Peptides Derived from Food Proteins
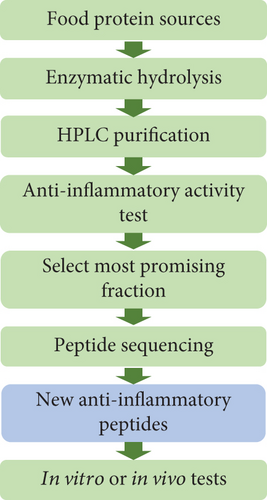
In the gut of human or animals, the BAPs encrypted in parent proteins can be released by various enzymatic digestion. However, there are several classical steps toward the in vitro production of novel BAPs from various food protein sources: enzymatic hydrolysis, purification by high-performance liquid chromatography, selection of most promising fraction, peptide sequencing, and final in vitro or in vivo bioactivity test (Figure 1) [5, 7, 16]. Due to their safety, the anti-inflammation potential of food-derived BAPs has become an active research area, and the intestinal tract is a main target of BAPs.
Recent knowledge of anti-inflammatory BAPs in in vitro studies with a concentration of 20-1000 μM was evaluated using mammalian cells induced by TNF-α, LPS, or H2O2, such as murine RAW 264.7 macrophages and human intestinal epithelial cell line Caco-2 cells (Table 1). There are many food-derived BAPs that can inhibit inflammation via the MAPK or NF-κB pathway (Table 1), such as CR, FL, HC, LL, MK [17], DEDTQAMPFR, DEDTQAMPF [18], DYKKY [19], EAMAPK, AVPYPQ [13], FLV [20], GPETAFLR [21], GPR [22], IPAV [23], IRW [24], IQW [12], LDAVNR, MMLDF [25], MLGATSL, MSYSAGF [18], PAY [26], PRRTRMMNGGR, MGPAMMRTMPG [27], QCQQAVQSAV [28], QQQQQGGSQSQ, QEPQESQQ, QQQQQGGSQSQSQKG, PETMQQQQQQ [29], SSEDIKE [30], VPP [31], IPP [32], VPY [33], VH, LAN, IA, AL [34], β-Ala-His [35], and pyroGlu-Leu [36]. Egg ovotransferrin-derived tripeptide IRW exhibits the anti-inflammatory effect through the NF-κB pathway by inhibiting p65 and p50 [24]. Moreover, whey protein-derived tetrapeptide IPAV can reduce IL-8 production via the NF-κB and MAPK pathways [23]. While BAPs have shown potential as anti-inflammatory agents in cultured cells, further in vivo studies and underlying mechanism are still necessary to verify their effectiveness in managing chronic inflammation [2].
| Peptides | Origin | Object | Administration | Activities | Results | Reference |
|---|---|---|---|---|---|---|
| CR, FL, HC, LL, MK | Egg ovotransferrin | TNF-α-induced Caco-2 cells | 0.05-2 mg/mL egg white digest | Reduce IL-8 secretion and expressions of TNF-α, IL-8, IL-6, IL-1β, and IL-12 and increase IL-10 expression | Inhibit intestinal inflammation | [17] |
| DEDTQAMPFR, DEDTQAMPF, MLGATSL, MSYSAGF | Egg white protein | TNF-α-induced Caco-2 cells | 0.25 mg/mL peptide | Inhibit expressions of TNF-α, IL-8, IL-6, IL-1β, IL-12, JNK, IκB, and p38 and increase IL-10 expression | Inhibit inflammation via the MAPK pathway | [18] |
| DYKKY | Milk whey protein | RAW 264.7 cells | 10 and 100 μg/mL | Inhibit expressions of IL-1β, COX-2, and TNF-α and productions of IL-1β and TNF-α and inhibit p38, p65, and IκBα degradation | Inhibit inflammation via the NF-κB pathway | [19] |
| EAMAPK, AVPYPQ | Milk casein | H2O2-induced IEC-6 cells | 5-150 g/mL peptide | Reduce ROS levels and increase SOD and Nrf2 activities | Antioxidation | [13] |
| FLV | Soybean protein | TNF-α-induced RAW 264.7 and 3T3-L1 cells | 0.1-1 μM FLV | Inhibit productions of TNF-α, IL-6, and MCP-1 and expressions of JNK, IKK, and IκBα | Inhibit inflammation | [20] |
| GPETAFLR | Lupine protein | THP-1-derived macrophages | 100-500 μg/mL GPETAFLR | Reduce expressions of TNF-α, IL-1β, and CCL2 and increase IL-10 expression | Prevent chronic inflammation | [21] |
| GPR | Amaranth protein | LPS-induced THP-1 and RAW 264.7 cells | 1 mg/mL hydrolysate | Inhibit TNF-α secretion | Inhibit inflammation via the NF-κB pathway | [22] |
| IPAV | Milk whey protein | TNF-α-induced Caco-2 cells | 25-200 μM IPAV | Reduce IL-8 and inhibit expressions of NF-κB, ERK1/2, JNK1/2, Syk, and p38 | Inhibit intestinal inflammation via PepT1 | [23] |
| IRW | Egg ovotransferrin | TNF-α-induced human endothelial cells | 50 μM IRW | Inhibit ICAM-1, VCAM-1, MCP-1, and NF-κB pathway | Inhibit vascular inflammation | [24] |
| IRW, IQW | Egg ovotransferrin | HUVECs | 50 μM IRW or IQW | Inhibit expressions of ICAM-1, VCAM-1, and NF-κB pathway | Inhibit endothelial inflammation and oxidative stress | [12] |
| LDAVNR, MMLDF | Spirulina maxima | RBL-2H3 mast cells and EA.hy926 cells | 200 μM peptide | Reduce histamine release, IL-8 production, and ROS production | Inhibit inflammation | [25] |
| Lunasin | Defatted soybean meal protein | LPS-induced RAW 264.7 cells | 100 μM lunasin | Inhibit NO and PGE2 production and COX-2 and iNOS expressions | Inhibit inflammation | [14] |
| PAY | Salmon protein | LPS-induced RAW 264.7 cells | 0.25-0.75 mM PAY | Reduce productions or expressions of NO, PGE2, TFN-α, IL-6, IL-1β, iNOS, and COX-2 | Inhibit inflammation | [26] |
| PRRTRMMNGGR, MGPAMMRTMPG | Juice of cooked tuna | LPS-induced RAW 264.7 cells | 100 μg/mL hydrolysate | Inhibit secretions of IL-2, TNF-α, and IFN-γ | Inhibit inflammation | [27] |
| QCQQAVQSAV | Ruditapes philippinarum hydrolysate | LPS-induced RAW 264.7 cells | 10-100 μg/mL peptide | Inhibit NO production | Inhibit inflammation | [28] |
| QQQQQGGSQSQ, QEPQESQQ, QQQQQGGSQSQSQKG, PETMQQQQQQ | Germinated soybean protein | LPS-induced RAW 264.7 cells | 2 mg/mL fraction | Inhibit NO and PGD2 production | Inhibit inflammation | [29] |
| SSEDIKE | Amaranth protein | Caco-2 cells | 100-200 μg/mL SSEDIKE | Reduce CCL20 and NF-κB expressions | Inhibit inflammation | [30] |
| VPP | Milk casein | 3T3-L1 adipocyte cells | 1 mM VPP | Inhibit TNF-α expression | Inhibit inflammation via ACE-dependent cascade | [31] |
| VPP, IPP | Milk casein | 3T3-F442A cells | 50 μM VPP or IPP | Upregulate PPARγ, activate NF-κB, and reduce adipokine | Inhibit inflammation | [32] |
| VPY | Soybean protein | Caco-2 and THP-1 cells | 0.1-4 mM VPY | Inhibit IL-8 and TNF-α secretions | Treat IBD via PepT1 | [33] |
| VH, LAN, IA, AL | Velvet antler protein from red deer | LPS-induced RAW 264.7 cells | 100-500 μg/mL peptide | Inhibit NO production | Inhibit inflammation | [34] |
| β-Ala-His | Meat products | H2O2-induced Caco-2 cells | — | Inhibit IL-8 and p38 and ERK activation | Inhibit inflammation via the MAPK and PepT1 pathways | [35] |
| pyroGlu-Leu | Wheat gluten | LPS-induced RAW 264.7 cells | 200-800 μg/mL peptide | Inhibit NO production, TNF-α, IL-6, and IκBα degradation, and JNK, ERK, and p38 phosphorylation | Inhibit inflammation via the NF-κB and MAPK pathways | [36] |
- 3T3-L1: mouse preadipocytes; ACE: angiotensin-converting enzyme; Caco-2: human colorectal adenocarcinoma-derived intestinal epithelial cells; COX-2: cyclooxygenase-2; EA.hy926: human umbilical vein endothelial cells; PPARγ: peroxisome proliferator-activated receptor gamma; RAW264.7: a mouse macrophage cell line; RAS: renin-angiotensin system; RBL-2H3: rat basophilic leukemia cells; ROS: reactive oxygen species; SOD: superoxide dismutase; THP-1: a human monocytic cell line; TNF-α: tumor necrosis factor α; HUVECs: human umbilical vein endothelial cells; ICAM-1: intercellular adhesion molecule-1; IL-1β: interleukin-1β; JNK: c-Jun N-terminal kinase; MAPK: mitogen-activated protein kinase; MCP-1: monocyte chemoattractant protein-1; NF-κB: nuclear factor-κB; NO: nitric oxide; VCAM-1: vascular cell adhesion molecule-1.
4. Pathways Involved in the Inhibition of Chronic Intestinal Inflammation by BAPs
There are four possible mechanism pathways for BAPs to attenuate chronic intestinal inflammation: NF-κB, MAPK, Janus kinase-signal transducer and activator of transcription (JAK-STAT), and peptide transporter 1 (PepT1) (Figure 2) [2, 7, 10, 20, 37–41]. Through inhibiting these pathways, BAPs can act the anti-inflammatory function in intestinal cells.
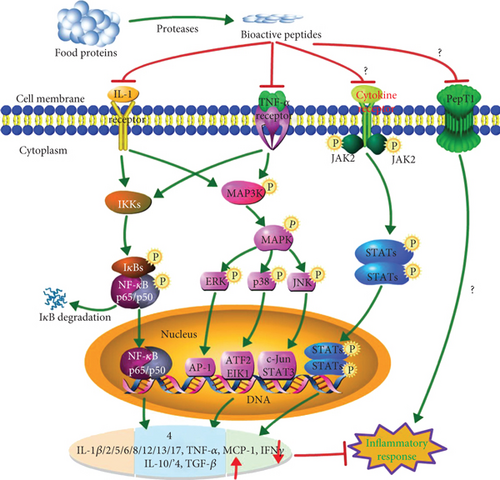
Among these pathways, the NF-κB and MAPK pathways are two main pathways for BAPs to inhibit inflammation [7]. The NF-κB is a key regulator of the expression and secretion of inflammatory cytokines (TNF-α, IL-1β, IL-6, and IL-8) and also plays a vital role in the expressions of cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) [42]. Inflammatory stimuli (IL-1β, LPS, TNF-α, viruses, or oxidative stress) activate inhibitory κB kinases (IKKα, IKKβ, and IKKγ), leading to phosphorylation of a potential cytoplasmic transcription factor that contains an inhibitor of κB (IκBα, IκBβ, and IκBγ) and IκBα degradation [42]. NF-κB is a family of transcription factor proteins, including five subunits: p65 (RelA), p50, p52, Rel, and RelB. After dimer p65/p50 is released into the cytosol, it can be translocated into the nucleus and initiates target gene transcription for proinflammatory factors, causing inflammation (Figure 2) [2, 42]. Many food-derived BAPs can inhibit inflammation via this NF-κB pathway, such as DYKKY [19], GPR [22], IRW [24], IQW [12], MLGATSL, MSYSAGF [18], pyroGlu-Leu [36], and TMKLLLVTL [43].
Another major signaling pathway, MAPK, can regulate many cellular activities, including proliferation, differentiation, death, and immune response. The stimulus and MAP3K phosphorylation can mediate the phosphorylation of the downstream MAP2K and MAPK, which contain three subfamilies: p38, extracellular signal-regulated kinases (ERK1 and ERK2), and c-Jun N-terminal kinase (JNK). In unstimulated cells, JNK mainly exists in the cytoplasm, but there is also some distribution in the nucleus. After being stimulated, JNK accumulates in the nucleus and causes the corresponding gene (IL-1 and TNF-α) expression, resulting in inflammatory response (Figure 2) [44]. Various food protein-derived BAPs can inhibit inflammation via this MAPK pathway, such as DEDTQAMPFR, DEDTQAMPF [18], FLV [20], MLGATSL, MSYSAGF [18], β-Ala-His [35], pyroGlu-Leu [36], DIKTNKPVIF [45], VPP [46], WH [41], γ-EC, and γ-EV [47].
Along with the above two pathways, the JAK-STAT pathway is also important for inflammatory response and can regulate hematopoietic cell development and inflammatory cytokines. Phosphorylation of JAK and STATs can form the dimer translocated to the nucleus [38]. BAPs can attenuate inflammation by inhibiting phosphorylation of JAK and STATs. However, the role of this pathway needs further verification for the anti-inflammation of BAPs. The translocations and activation of the substrate proteins from the above three pathways, including transcription factors in the nucleus (AP-1, ATF-2, EIK1, and c-Jun), cause the change of target genes, reducing the productions of proinflammatory cytokines, including IL-1β, IL-2, IL-5, IL-8, IL-12, IL-13, IL-17, TNF-α, MCP-1, and IFN-γ. The overexpression of these proinflammatory mediators and the downexpression of anti-inflammatory cytokines (IL-4, IL-10, and TGF-β) can lead to intestinal inflammation. Through regulating these pathways and cytokines, BAPs can attenuate chronic intestinal inflammation and diseases.
5. Mechanism of Food-Derived Anti-Inflammatory Peptides to Exert Bioactivities
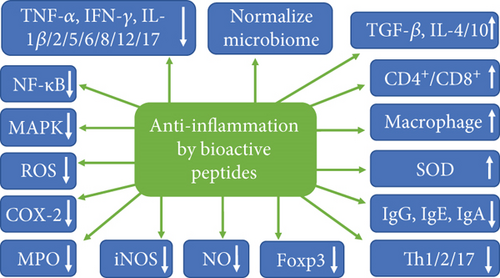
The potential anti-inflammatory mechanisms of BAPs derived from food proteins through regulating various cytokines or systems are shown in Figure 3 [7, 48]. The secretions and expressions of proinflammatory cytokines IL-1β, IL-2, IL-5, IL-6, IL-8, IL-12, IL-17, TNF-α, and IFN-γ can be inhibited by BAPs, as well as the activations of NF-κB and MAPK pathways, COX-2, ROS, iNOS, and nitric oxide (NO). ROS are associated with inflammatory diseases, and NO is synthesized by NO synthase (NOS) enzyme (iNOS), and the inhibition of iNOS and ROS activities can suppress NO production. BAPs can also inhibit the expression and release of a transcription factor that drives treg phenotypic differentiation (Foxp3) and T-helper-cell-associated cytokines (Th1, Th2, and Th17) and the secretions of IgG, IgE, and IgA. On the other side, secretions and expressions of anti-inflammatory cytokines (IL-4, IL-10, and TGF-β), CD4+/CD8+, numbers of macrophages, and superoxide dismutase (SOD) activity can be increased by BAPs. In addition, the gut microbiome, which is an active topic in health, can be normalized by BAPs [7, 48]. In conclusion, these cytokines and pathways are the molecular targets and mechanisms for BAPs to regulate the intestinal inflammation of human and animals.
Milk-derived VPP and IPP can exhibit beneficial effect in an animal colitis model through anti-inflammatory action for these targets [49]. VPP also reduced TNF-α and IL-1β expression and macrophage accumulation and activation, inhibited adipose inflammation in mice via angiotensin-converting enzyme-dependent cascade [31], and moderated monocyte adhesion to inflamed endothelia via the MAPK-JNK pathway [50]. In addition, tripeptides IRW and IQW downregulated the expression of inflammatory proteins via the NF-κB pathway [12, 24]. Generally, these BAPs can inhibit the expression of cytokines and mediate the NF-κB and MAPK pathways [1].
6. The In Vivo Studies of BAPs on Inflammation
For the in vivo studies of BAPs, various inflammatory models have been used, typically colitis in mice induced by DSS and TNBS. As observed in human CD, the administration of TNBS to mice can release proinflammatory cytokines, followed by infiltration of T cell CD4+ phenotype. In these studies, the mice with colitis were orally administered with BAPs mostly with an amount of 50-500 mg/kg body weight/day for several days to weeks (Table 2). Then, the tissues are collected for common evaluation of anti-inflammation of BAPs using morphological, immunological, and biochemical assays [51], such as body weight, colonic length, disease activity index (DAI), lymphocyte proliferation, CD4+/CD8+ determination, secretory-immunoglobulin-A (s-IgA) measurement, immunoglobulin (IgA, IgM, and IgG) determination, and cytokine (IL-1, IL-2, IL-6, IL-8, IL-10, TNF-α, and IFN-γ) measurements (Table 2).
| Peptides | Origin | Object | Administration | Activities | Results | Reference |
|---|---|---|---|---|---|---|
| AQ | Synthesis | Early-weaned calves | Intravenous infusion 1.01 g/kg BW/d AQ | Increase concentrations of CD2+ and CD4+ lymphocytes, CD4+/CD8+ ratio, and IgA, IgG, and s-IgA and improve intestinal integrity | Improve gain performance and decrease diarrhea occurrence | [52] |
| AQ | Synthesis | DSS-induced colitis C57BL/6 mice | Inject 75 mg/kg BW/d AQ | Reduce Th1/Th2/Th17, haptoglobin, IgG, chemokine, and MPO activity | Attenuate colitis | [9] |
| AQ | Synthesis | DSS-induced colitis C57BL/6 mice | Inject 75 mg/kg BW/d AQ | Increase colon length, TLR4, NF-κB activation, and expressions of mucin 2, IL-17, and TNF-α and reduce IgG, DAI, and haptoglobin | Inhibit inflammation and enhance mucosa recovery | [53] |
| AQ | Synthesis | DSS-induced colitis C57BL/6 mice | Inject 75 mg/kg BW/d AQ | Reduce IL-17, Th17, and macrophage | Inhibit inflammation | [54] |
| DIKTNKPVIF | Potato protein hydrolysate | HFD-fed SAMP8 mice | Oral and intraperitoneal injection | Reduce expressions of p-p38, FGF-2, TNF-α, and IL-6 | Attenuate proinflammatory reaction via the MAPK pathway | [45] |
| EWP | Egg white protein | DSS-induced IBD in piglets | Infuse 150 mg/kg BW EWP for 5 days | Reduce weight loss, crypt distortion, and expressions of TNF-α, IL-6, IL-1β, IFN-γ, IL-8, and IL-17 and restore gut barrier function | Manage IBD | [55] |
| GLTSK | Phaseolus vulgaris | AOM/DSS-induced colitis BALB/c mice | Oral 50 mg/kg BW/d GLTSK | Reduce DAI and neoplasms and enhance colon length | Attenuate colitis | [56] |
| Glycomacropeptide | Milk κ-casein | TNBS-induced ileitis rat | Oral 500 mg/kg BW/d peptide | Reduce DAI, MPO, alkaline phosphatase, iNOS, IL-1β, IL-17, and TNF | Attenuate ileitis via reducing IL-17 | [57] |
| Glycomacropeptide | Milk κ-casein | DSS-induced colitis C57BL/6 female mice | Gavage 500 mg/kg BW/d peptide | Reduce DAI and normalize colonic expressions of IL-1β, IL17, IL23, IL6, TGF-β, IL10, and Foxp3 | Inhibit inflammation | [58] |
| Glycomacropeptide | Milk κ-casein | DSS-induced colitis mice | Gavage 15 mg/d peptide | Increase BW and reduce DAI, CD4+, IFN-γ, and MPO activity | Inhibit colitis inflammation | [59] |
| Glycomacropeptide | Milk κ-casein | Oxazolone-induced ulcerative colitis BALB/c mice | Oral 50 mg/kg BW/d peptide | Inhibit NF-κB and MAPK activations and reduce serum IL-1β, IL-5, IFN-γ, TNF-α, and IL-10 production | Attenuate colitis | [60] |
| Lunasin | Soybean protein | LPS-induced airway inflammation mice | Intranasal 20 μg/mice lunasin | Reduce infiltration, goblet cell metaplasia, and Th2 cytokine expression | Alleviate inflammation | [15] |
| IRW | Egg ovotransferrin | Spontaneously hypertensive rat | Oral 15 mg/kg BW/d IRW | Reduce ICAM-1 and VCAM-1 expression | Inhibit inflammation and hypertension via the NF-κB pathway | [11] |
| IRW | Egg ovotransferrin | LPS-induced inflammatory peritonitis in rat | Oral 40 mg/kg IRW in feed | Reduce serum TNF-α and IL-6 and MPO activity, increase Shannon index, and decrease Simpson indices | Attenuate inflammation | [61] |
| IRW, IQW | Egg ovotransferrin | DSS-induced colitis in mice | Drink water with 30 mg/mL peptide | Increase antioxidant enzyme activities and microbial diversity and abundance | Attenuate colitis | [63] |
| IRW, IQW | Egg ovotransferrin | DSS-induced colitis in mice | Oral 0.03% peptide in diet | Reduce TNF-α and IL-17 | Inhibit colonic inflammation | [64] |
| IRW, IQW | Egg ovotransferrin | Citrobacter rodentium-induced colitis in mice | Oral 0.03% peptide in diet | Regulate intestinal microorganisms | Inhibit colonic inflammation | [62] |
| KGHYAERVG | Rice | Autoimmune encephalitis mice | Oral 100 mg/kg peptide | Reduce productions of IL-17, IFN-γ, IL-23, and IL-12 and increase T cells | Attenuate autoimmune encephalitis | [65] |
| KPV | C-terminal sequence of α-melanocyte stimulating hormone | DSS- and TNBS-induced colitis in mice | Drink water with 100 μM KPV | Decrease expressions of IL-6, IL-12, IFN-γ, and IL-1β | Reduce intestinal inflammation via PepT1 | [66] |
| PTGADY | Alaska pollock hydrolysates | Hydrogenated cortisone-treated mice | Oral 50-200 mg/kg BW/d hydrolysate | Increase productions of IL-2, IL-4, and IL-6 | Immunomodulation | [67] |
| QCQCAVEGGL | Crassostrea gigas | DSS-induced colitis mice | Oral 50 mg/kg BW/d hydrolysate | Reduce IgE and increase spleen CD4+/CD8+ | Attenuate colitis | [68] |
| QEPVL, QEPV | Milk casein | LPS-induced mice | Oral 200 mg/kg BW/d peptide | Reduce NO release, increase IL-4 and IL-10 production, and decrease IFN-γ and TNF-α production | Inhibit inflammation | [6] |
| RILSILRHQNLLKELQDLAL | Chromogranin A | DSS-induced colitis in mice | Intracolonic injection 2.5 mg/kg/day peptide | Reduce IL-18, active macrophages, increase TJ proteins | Attenuate colitis | [69] |
| SSEDIKE | Amaranth seeds | IgE-mediated food allergy mouse | Gavage 100 μg SSEDIKE | Reduce productions of IgE, IgG, IL-5, IL-13, and NF-κB and increase TGF-β and Foxp3 expressions | Inhibit intestinal inflammation | [70] |
| TMKLLLVTL | Corn silk extract | LPS-induced inflammatory mice | Oral 1 mg/kg peptide | Inhibit IL-β, IKKβ, and IκB phosphorylation and NF-κB activation | Inhibit inflammation via the IKKβ-NF-κB pathways | [43] |
| VPP | Milk casein | HFD-induced adipose inflammation mice | Drink water with 0.3 mg/mL VPP for 10 weeks | Reduce monocytes, macrophages, CD18, IL-6, and MCP-1 | Attenuate inflammation via the MAPK-JNK pathway | [46] |
| VPP | Milk casein | Obesity-induced adipose inflammation C57BL/6J mice | Drink water with 0.1% VPP for 4 months | Reduce TNF-α and IL-1β expression and macrophage accumulation and activation | Attenuate inflammation | [31] |
| VPP, IPP | Milk casein | Apolipoprotein E-deficient mice | Oral 60.2 or 125 μmol/kg BW/d peptide | Reduce IL-6, IL-1β, and oxidized low-density lipoprotein receptor | Attenuate atherosclerosis | [71] |
| VPP, IPP | Milk κ-casein | L-NAME-treated rats | Drink water with 0.3 mg/mL VPP or IPP | Increase vasorelaxation and nitrite and nitrate and reduce cardiac and renal damage | Attenuate arterial dysfunction | [72] |
| VPY | Soybean protein | DSS-induced colitis BALB/C female mice | Drink water with 1 mg/mL VPY (100 mg/kg BW/d) | Reduce DAI, weight loss, and MPO activity and expressions of TNF-α, IL-6, IL-1β, IFN-γ, and IL-17 | Treat IBD via PepT1 | [33] |
| WH | Sardine muscle hydrolysate | DSS-induced colitis BALB/c mice | Oral 100 or 250 mg/kg BW/d WH for 14 d | Reduce DAI, cytokine expression, MAPK and IκBα activation, and IL-8 secretion | Inhibit intestinal inflammation | [41] |
| Milk casein hydrolysates | Lactobacillus fermentation | TNBS-induced colitis mice | Oral 150 μg/d hydrolysate | Reduce BW loss, microbial translocation, colonic DAI, and IFN-γ production | Treat colitis | [73] |
| Di- and tripeptides | Soybean protein | DSS-induced colitis pig | Infuse 250 mg/kg BW/d peptides | Reduce the expressions of IFNG, IL-1B, IL-12B, TNF, and IL-17A and MPO activity and increase Foxp3 expression and CD4+CD25+ T cells | Attenuate colon and ileum inflammation | [74] |
| Peptide P-317 | Cyclic analog of morphiceptin | TNBS/DSS-induced colonic mice | Intraperitoneal 0.2 or oral 2 mg/kg BW/d peptide | Inhibit TNF-α and IL-1β expression and MPO activity | Treat IBD | [75] |
| pyroGlu-Leu | Wheat gluten | DSS-induced colitis mice | Gavage 0.01-10 mg/kg BW/d peptide | Reduce DAI and normalize colonic Bacteroidetes and Firmicutes | Treat IBD via gut microbiota | [76] |
| β-Casofensin | Milk protein | NMS-induced intestinal barrier alteration rat | Oral 10 μL/kg BW/d peptide (0.01-100 μM) | Reduce intestinal damages and prevent neonatal stress | Protect gut barrier | [77] |
| γ-EC, γ-EV | Beans and yeast extracts | DSS-induced BALB/C female mice | Gavage 50 or 150 mg/kg BW/d peptide | Inhibit IκBα and JNK activation and the expressions of TNF-α, IL-6, INF-γ, IL-1β, and IL-17 and increase IL-10 expression | Inhibit colitis inflammation via the TNF-α pathway | [47] |
- ACE: angiotensin-converting enzyme; AOM: azoxymethane; BW: body weight; CD4+/CD8+: splenic T lymphocyte subpopulations; DAI: disease activity index; DSS: dextran sulfate sodium; Foxp3: a transcription factor that drives treg phenotypic differentiation; glycomacropeptide: a 64-amino acid peptide in stomach casein hydrolysis; HFD: high-fat diet; IBD: inflammatory bowel diseases; iNOS: inducible oxide nitric synthase; IFN: interferon; IKKβ: inhibitory κB kinase-β; IL-1β: interleukin-1β; KC: keratinocyte-derived chemokine; LPS: lipopolysaccharide; L-NAME: N(G)-nitro-L-arginine methyl ester hydrochloride; MCP-1: monocyte chemoattractant protein-1; MPO: myeloperoxidase; NF-κB: nuclear factor-κB; NMS: neonatal maternal separation; NO: nitric oxide; PPARγ: peroxisome proliferator-activated receptor gamma; RAW264.7: a mouse macrophage cell line; SAMP8: senescence-accelerated mice prone 8; TGF-β: transforming growth factor β; TJ: tight junction; TLR4: toll-like receptor 4; Th1/2/17: T-helper-cell-associated cytokine 1/2/17; TNBS: 2,4,6-trinitrobenzene sulfonic acid.
Numbers of BAPs derived from various food proteins (milk, plant, egg, soybean, meat, wheat, rice, potato, corn silk, fish, etc.) have been found to be well suited to treat inflammation or IBD symptoms in vivo (Table 2), such as Ala-Gln (AQ) [9, 52–54], DIKTNKPVIF [45], EWP [55], GLTSK [56], glycomacropeptide [57–60], lunasin [15], IRW [11, 61–63], IQW [62–64], KGHYAERVG [65], KPV [66], PTGADY [67], QCQCAVEGGL [68], QEPVL, QEPV [6], RILSILRHQNLLKELQDLAL [69], SSEDIKE [70], TMKLLLVTL [43], VPP [31, 46, 71, 72], IPP [71, 72], VPY [33], WH [41], casein hydrolysates [73], soybean dipeptides and tripeptides [74], peptide P-317 [75], pyroGlu-Leu [76], β-Casofensin [77], γ-EC, and γ-EV [47]. These studies suggest that oral administration of food-derived BAPs have anti-inflammatory effects, and they can be the therapeutic agents for inflammatory-related diseases, including IBD [78].
Oral administration of dipeptide AQ reduced inflammatory cytokine expression, enhancing the mucosa recovery in DSS-induced mice [53]. Likewise, intravenous infusion with AQ to calves with early weaned stress can increase concentrations of IgA, IgG, s-IgA, CD2+ and CD4+ lymphocytes, and CD4+/CD8+ ratio; therefore, the diarrhea occurrence was decreased [52]. Bean protein is also a rich resource for BAPs. For example, bean- and yeast extract-derived flavor peptide γ-EC and γ-EV can inhibit the inflammation in IBD mice [47]. Soybean-derived dipeptides and tripeptides decreased the colonic expressions of proinflammatory IFNG, IL-1B, IL-12B, TNF, and IL-17A and MPO activity and increased Foxp3 expression and CD4+CD25+ T cells; therefore, the colon and ileum inflammation of piglets with DSS-induced colitis was attenuated [74]. In addition, with the infusion of 150 mg/kg of egg white protein-derived EWP, weight loss, crypt distortion, IL-6 and TNF-α concentrations, and expressions of IL-1β, IL-8, IL-17, and IFN-γ in the colon of piglets with DSS-induced colitis can be reduced, and gut barrier function was restored [55], as well as the barrier protection effects of milk-derived β-Casofensin [77] and dipeptide AQ [53]. Therefore, food-derived BAPs can contribute to disease treatment through modifying intestinal barrier function [79].
In DSS-induced mice, antioxidant enzyme activities and microbial diversity and abundance were increased and the colitis was attenuated by egg white protein-derived IRW and IQW [63]. Oral administration of corn silk extract-derived TMKLLLVTL suppressed IKKβ activity, IκB phosphorylation, NF-κB activity, and IL-1β production in LPS-induced inflammatory mice [43]. Drinking water with soybean-derived tripeptide VPY can reduce DAI, weight loss, MPO activity, and expressions of IL-1β, IL-6, IL-17, IFN-γ, and TNF-α in colitis mice [33], suggesting that VPY can treat IBD. In addition, sardine muscle hydrolysate-derived dipeptide WH can reduce DSS-induced colitis symptoms, colonic cytokine expression, MAPK and IκBα activation, and IL-8 secretion in colitis mice, indicating that WH can inhibit intestinal inflammation [41]. Favor peptide γ-EC and γ-EV inhibited IκBα and JNK activation and expressions of IL-1β, IL-6, IL-17, INF-γ, and TNF-α and increased IL-10 expression in IBD mice [47]. Moreover, tripeptide KPV reduced intestinal inflammation by decreasing IL-1β, IL-6, IL-12, and IFN-γ expressions and attenuated colitis via PepT1 [66].
Milk protein is a rich source for BAPs, which has potential beneficial effects to the gut of humans and animals [80, 81]. Milk casein-derived VPP and IPP are two famous BAPs with antihypertensive and anti-inflammatory activities. Proinflammatory IL-6 and IL-1β were reduced, and atherosclerosis was attenuated by oral administration of VPP and IPP [71]. Arterial dysfunction was attenuated by drinking water with VPP and IPP through increasing vasorelaxation and nitrite and nitrate and reducing pulse wave velocity and cardiac and renal damage [72]. It was reported that VPP attenuated inflammation via the MAPK-JNK pathway by reducing monocytes, macrophages, CD18, IL-6, and MCP-1 in adipose inflammatory mice [46]. Milk casein-derived QEPVL and QEPV reduced nitric oxide (NO) release, increased anti-inflammatory IL-4 and IL-10 production, and decreased productions of IFN-γ and TNF-α in LPS-induced mice [6]. Milk κ-casein-derived glycomacropeptide inhibited inflammation and attenuated colitis via normalizing the inflammatory cytokine and the NF-κB and MAPK pathways in previous studies [57–60].
From these in vivo studies, the evidences that the intestinal inflammation can be attenuated by oral administration of food protein-derived BAPs have been presented. As many studies have been performed recently, large-scale human and animal trials are still lacking [2]. It has been reviewed that numbers of BAPs can be transported into the bloodstream of humans or animals to exert bioactivities [3, 81]. However, there is still limitation for such in vivo studies due to the possible degradation of BAPs by peptidases in the gut and plasma or insufficient absorption [82]. In the future, more studies of humans and animals are needed to evaluate the anti-inflammatory effects of BAPs, as well as the doses, times, and kinetics in the body.
7. Peptide Transporter PepT1
The peptide transporter 1 (PepT1) can transport small peptides from the intestine into the bloodstream of humans or animals [83–85], particularly di- and tripeptides, and its expression in intestinal epithelial cells is increased when the intestine is suffering from inflammation [86], indicating that PepT1 is a gateway to inflammatory response [87]. Similarly, PepT1 can transport various BAPs into intestinal epithelial cells to exert bioactivities [3, 81], such as IPAV [23], KPV [66], LKP, IQW [88], LSW [89], IWH, IW [90], and VPY [33].
It was reported that anti-inflammatory tripeptide KPV can attenuate intestinal inflammation associated with PepT1 expression, and KPV lost the anti-inflammatory function without PepT1 expression, suggesting that PepT1 mediates the anti-inflammation of KPV [66]. It was reported that soy protein-derived tripeptide VPY exerted anti-inflammatory activity in cells also through PepT1, which can transport VPY into cells [33]. In addition, pharmacological inhibition of PepT1 can counteract the inhibition of IL-8 expression mediated by peptide IPAV [23]. Moreover, the anti-inflammatory effect of meat-derived carnosine (β-Ala-His) was inhibited by dipeptide Gly-Sar, a PepT1 substrate [35]. These findings indicate that PepT1 is a promising target to treat intestinal inflammation by transporting sufficient short-chain BAPs into colonic cells [10]. In conclusion, PepT1 is a possible mechanism for the inhibition of intestinal inflammation by BAPs. However, this PepT1 pathway involved in anti-inflammation of BAPs still needs to be verified by further researches in the future (Figure 2).
8. Impact of Anti-Inflammatory Peptides on Gut Microbiota
When intestinal inflammation or IBD occurs, the gut microbial community would also change, such as the decrease of Firmicutes (particularly Clostridium groups) and the increase of Bacteroides, Lactobacillus, Eubacterium, and Proteobacteria [91]. In DSS-induced colitis mice, compositions and varieties of the gut microorganism (Anaerotruncus, Bacteroides, Enterobacteriaceae, Lactobacilli, and Parabacteroides) have changed [92]. In general, when defensins decline, the abundance of bacteria from Bacteroides and Firmicutes would be increased [93].
It was reported that BAPs can exert anti-inflammation via changing the gut microbiota in several studies [62, 63, 76]. For example, oral administration of anti-inflammatory peptide pyroGlu-Leu derived from wheat gluten can normalize the population of Bacteroidetes and Firmicutes in the colon of colitis mice [76]. Shannon and Simpson indices represent species richness and species evenness, respectively. The Simpson index and the abundance of Coprococcus-1, Desulfovibrio, and Ruminococcaceae-UCG-014 were increased by tripeptides IRW and IQW. Additionally, IQW decreased the abundance of Bacteroides and increased Parabacteroides, while the levels of Anaerotruncus, Ruminiclostridium-9, and Oscillibacter were increased by IRW [63]. Firmicutes and Actinobacteria species were increased, and the proportions of Bacteroidetes and Proteobacteria species were decreased by oral administration of IRW and IQW; therefore, the colonic inflammation was inhibited via regulation of intestinal microorganisms [62]. In addition, dietary dipeptide GQ changed the gut microbiota beneficially through increasing alpha diversity, bacterial loading, abundance of anaerobes and fiber-degrading bacteria (Phylum Fibrobacteres), and short-chain fatty acids in the gut [94].
In conclusion, the gut microbiota is a promising mechanism for BAPs to inhibit intestinal inflammation. However, the information of the mechanism underlying the effects of BAPs on gut microbiota is still lacking, and it needs more studies to explore the interaction between anti-inflammation of BAPs and gut microbiota in the future.
9. Conclusions and Future Perspectives
In this review, the mechanism and pathways of food protein-derived BAPs to exert anti-inflammatory bioactivities were highlighted, including pathways (NF-κB, MAPK, and JAK-STAT), PepT1, inflammatory mediators, and gut microbiota. Moreover, various in vitro and in vivo studies of BAPs on inflammation were reviewed, finding that PepT1 and gut microbiota are promising targets for the inhibition of BAPs on intestinal inflammation; however, their roles still need more further studies to be verified in the future.
The discovery of novel BAP sequences and their corresponding action mechanisms as well as gut microbiota and PepT1 involved in the mediation can provide new opportunities for better targeting of intestinal inflammation. More in vivo data, including pharmacokinetics and proper dosage and time of administration of BAPs, are needed before their application to humans and animals. The role of dietary BAPs in inhibiting intestinal inflammation represents a novel direction in nutraceuticals for people or animals with intestinal inflammation.
Conflicts of Interest
The authors declare that they have no competing interests.
Acknowledgments
This work was supported by grants from the State Key Laboratory of Animal Nutrition (2004DA125184F1906) and the Fundamental Research Funds for the Central Universities (2662019QD021).