A cross-sectional study on gender differences in body dysmorphic concerns in patients with skin conditions in relation to sociodemographic, clinical and psychological variables
Abstract
Background
Dysmorphic concern is an overconcern with an imagined or slight defect in physical appearance that can be a symptom of body dysmorphic disorder (BDD). Appearance-related concerns are frequently reported by people with dermatological conditions. However, relatively little remains known about the relationship between dysmorphic concern and other variables within persons with different skin conditions.
Objectives
The aim of this multicentre, cross-sectional study was to investigate gender differences regarding dysmorphic concern and the prevalence of BDD in a large sample of patients with skin conditions, in relation to sociodemographic, clinical and psychological variables.
Methods
Participants aged ≥18 years with skin conditions were consecutively enrolled in dermatological clinics of 22 European centres. Dysmorphic concern and the possible presence of BDD were measured using the Dysmorphic Concern Questionnaire (DCQ) and compared between men and women in relation to sociodemographic, clinical and psychological variables, and separately for each skin condition.
Results
The DCQ questionnaire was completed by 5290 dermatological patients. In all categories, mean scores were significantly higher in women than in men. Mean DCQ scores were also higher in women for most skin conditions, with the highest effect size in vitiligo. The percentage of patients who screened positive for BDD on the DCQ was 10.5%, 7.7% of men and 12.7% of women. The prevalence of BDD positive was 6.9% in patients with mild clinical severity, 11.1% for moderate and 19.1% for severe condition. In the multivariate model in patients with mild skin condition, the presence of BDD was positively associated with stress and stigma both in men and in women.
Conclusions
Dysmorphic concern and BDD were more frequent in women than in men with skin conditions. Both received and actual stigmatization might have an impact on body-related concerns, in particular in women, who may be more at risk for sociocultural reasons.
Graphical Abstract
Why was the study undertaken?
Body appearance and body image are crucial characteristics for the self-evaluation in contemporary Western societies. The research question was to investigate dysmorphic concern and body dysmorphic disorders (BDD) in subgroups of dermatological patients with regard to sociodemographic, clinical, and psychological variables.
What does this study add?
Both dysmorphic concerns and BDD were significantly more prevalent in women than in men, consistently across different categories of sociodemographic, clinical and psychological variables, and in almost all participating countries.
What are the implications of this study for disease understanding and/or clinical care?
This study highlights the higher prevalence of dysmorphic concerns and BDD in women among dermatological patients, emphasizing their association with stress and stigma, and the need for gender-specific, multidisciplinary approaches to improve clinical care.
INTRODUCTION
Dysmorphic concern is an overconcern with an imagined or slight defect in physical appearance that can be a symptom of body dysmorphic disorder (BDD). BDD is a psychiatric condition characterized by an excessive concern about perceived defects in physical appearance.1 To be diagnosed as BDD, the preoccupation with non-existent or slight appearance flaws must cause clinically significant distress or clinically significant impairment in functioning. BDD is more frequent in dermatological settings, with an estimated prevalence of 11.3%,2 than in the general population, where the prevalence has been estimated around 2%.2 In fact, although patients with BDD may be worried about any parts of the body, skin, hair and nose are the most frequent areas of concern.3 Patients with BDD repeatedly consult dermatologists and aesthetic surgeons, with high costs for healthcare systems; however, they are often dissatisfied with both dermatological and surgical treatments.4
Moreover, BDD is often associated with other psychological symptoms, such as depression and low self-esteem.5 In a previous publication using the same data set,6 we reported a prevalence of BDD (i.e. patients who screened positive for the disorder BDD on the Dysmorphic Concern Questionnaire (DCQ)7-10) of 10.5% in dermatology patients, five times higher than in healthy controls, with women reporting a higher prevalence than men. Studies on gender differences in BDD prevalence reported conflicting results. For example, a higher prevalence in women was observed by Buhlmann et al.,11 while in other studies there were no significant differences,12 and in a study the prevalence was higher in men.13 However, those data were extracted from samples of the general population. In dermatology and plastic surgery patients, there is a clear majority of women reporting BDD. In the meta-analysis by Ribeiro,14 only 3 studies out of 33 reported a higher prevalence in men. Some differences between men and women exist in body perception. It has been observed that women are more likely to report concerns regarding their skin, weight, body shape, and facial features, while men tend to be more preoccupied with genitals, muscle size and hair loss.3 To the best of our knowledge, a thorough analysis of gender differences in dysmorphic concerns and BDD among dermatological patients has not been performed.
Thus, the present study is the first to analyse gender differences in dysmorphic concern and BDD in subgroups of dermatological patients with regard to sociodemographic, clinical and psychological variables.
MATERIALS AND METHODS
This study is part of a series of studies conducted by the European Society for Dermatology and Psychiatry (ESDaP) on psychological aspects of patients with dermatological conditions.15, 16 Study design, participants and methodology of this cross-sectional study have been previously described in detail.6, 15 The study was conducted in 17 European countries including consecutive dermatological patients aged ≥18 years. A group of controls with no skin conditions was recruited among hospital staff and visitors. The study was approved by the Institutional Review Board of the Department of Medicine at the University of Giessen (protocol number 87/17), and at each recruitment centre, and conducted in accordance with the Declaration of Helsinki.
Collected data
Sociodemographic and clinical variables
Participants completed a questionnaire including sex, age, marital status, educational level, income, height and weight. Disease severity was assessed by the dermatologist as ‘mild’, ‘moderate’ or ‘severe’. Localization of flares, itch in the last 24 h and the presence of comorbidities were also recorded. The condition was defined as visible, if flares were in the face/on the neck, scalp and/or hands/arms.
Body dysmorphic concerns
The Dysmorphic Concern Questionnaire (DCQ)7-10is a validated, self-reported screening instrument, largely conceptualized according to the criteria of DSM-IV for BDD. It consists of seven items measuring concerns on one's body appearance (score range 0–21). In its original form, when used as a dimensional measure, the DCQ identifies individuals with dysmorphic concerns. Even though excessive concerns may also be indicative of the presence of BDD, it is important to highlight that DCQ is not the gold standard tool for diagnosing or screening for BDD, but it has been shown to have a high sensitivity for BDD diagnosis in general population,10, 17 and in dermatologic settings.18 A validation study9 showed that the optimal cut-off score to classify patients with BDD in dermatological conditions was 14 (i.e. a score of 14 or higher indicates BDD), with a sensitivity of 72% and a specificity of 90.7%. Cronbach's α in the present sample was 0.89.
Psychological and general health variables
The presence of symptoms of depression and anxiety was screened using the 2-item Patient-Health-Questionnaire (PHQ-2)19 and the 2-item General Anxiety Disorder (GAD-2)20 (range score for each item: 0–3). For each instrument, a score of 3 points is the preferred cut-off for identifying possible cases. In our sample, Cronbach's α were 0.80 and 0.82 for the depression and the anxiety scale, respectively. Perceived stigmatization was assessed with the 21-item Perceived Stigmatization Questionnaire (PSQ),21 consisting of three subscales: ‘absence of friendly behavior’, ‘confused/staring behavior’ and ‘hostile behaviour’ (total score range: 0–84, with higher scores indicating higher perceived stigmatization). In our sample, the reliability of the PSQ was good (Cronbach's α = 0.89). The Perceived Stress Scale (PSS)22 evaluates stress perception with 20 items rated on a 5-point Likert scale (from 0 ‘never’ to 4 ‘very often’; total score range: 0–80, with higher scores indicating higher perceived stress). In our sample, its Cronbach's α was 0.84. Stress was also evaluated using the question ‘Have you had any stressful life events during the last 6 months (serious illness, death of close friend or family member, accident, divorce or other events)?’, with the answer-categories yes/no. Current health state was assessed by the EuroQol 5-D23 (visual analogue scale [VAS]) from 100 (‘The best health you can imagine’) to 0 (‘The worst health you can imagine’). The dermatologist recorded physical comorbidities and in particular cardiovascular, respiratory and rheumatological diseases, and diabetes.
Statistical analysis
Categorical variables were described as number and percentages and continuous variables as means and standard deviations. Tertiles of age distribution were calculated (<37, 37–57 and >57 years). BMI was classified as underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9) and obese (≥30). The presence of comorbidities was defined as the presence of at least one comorbidity. Due to skewness of the DCQ scores, differences in the DCQ distributions between men and women were evaluated using the Mann–Whitney U non-parametric test for two categories, and Kruskal–Wallis test for more than two categories. The prevalence of positive answers (‘more than most people’/‘much more than most people’) in each DCQ item was compared between men and women, using the chi-square test. For the mean differences, Cohen's d effect size was calculated, assuming a cut-off of 0.2 for ‘very small/small’, of 0.50 for ‘medium’ and of 0.80 for ‘large’, effect.
Multivariate logistic regression analysis was conducted with the dichotomized DCQ score (cut-off = 14) as dependent variable, to investigate the association between BDD and clinical variables and psychological status, while adjusting for possible confounders. Variables included in the model as independent variables were as follows: age, marital status (single/married), education, BMI, skin disease severity, visible flare (yes/no), comorbidities (yes/no), stress (PSS), stigma (PSQ), depression (PHQ, yes/no), anxiety (GAD, yes/no) and VAS health. The same analysis was performed only on patients with mild clinical severity.
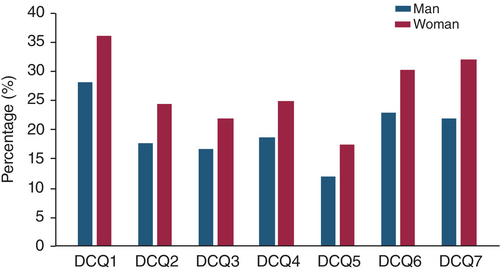
RESULTS
In total, 5847 participants with skin conditions were enrolled in the study, and 5290 (90.5%) of them completed the BDD questionnaire. Patients without missing data on gender were 5253, 56.8% of whom were women. Mean (SD) age was 48.7 (17.6) years (range 18–100), 49.3 (17.9) years in men and 47.7 (17.2) years in women. The percentage of patients who screened positive for the disorder BDD on the DCQ was 10.5% (553/5253), 7.7% of males (174/2268) and 12.7% of females (379/2985), p < 0.001 from Fisher test. The prevalence of BDD positive was 6.9% in patients with mild clinical severity, 11.1% for moderate and 19.1% for severe condition. Table 1 reports mean DCQ scores (range 0–21) for men and women separately, also considering sociodemographic, clinical and psychological variables for subgroup determination. In all categories, mean scores were significantly higher in women than in men, except for BMI < 18 and VAS-EQ between 50 and 59.9. The effect size for the comparisons was generally around 0.30. Mean DCQ scores were also higher in women for most skin conditions (Table 2), that is acne, allergies, atopic dermatitis, benign tumours, malignant melanoma, metabolic and systemic disease, nevi, non-melanoma skin cancer, prurigo, psoriasis, rosacea, scaly conditions, urticaria and vitiligo. The highest effect size was observed for vitiligo, followed by alopecia, hyperhidrosis and urticaria. Mean DCQ scores were compared between men and women also in the different countries (results not shown): scores were significantly higher in women in all countries, except Macedonia, Poland, Russia and Turkey, where the difference was not significant. The frequency of the answers ‘more than most people’/‘much more than most people’ was higher in women than in men for all items (Figure 1). The logistic regression model (Table 3) in men showed that BDD was negatively associated with age and positively associated with education level, stress (PSS score), stigma (PSQ score) and anxiety (GAD y/n). In women, BDD was negatively associated with age and positively associated with stress (PSQ score), stigma (PSQ score) and depression (PHQ, y/n). The logistic regression model applied to patients with a mild skin condition (Table 4) showed a positive association between BDD and stress (PSQ score) and stigma (PSQ score) in both men and women.
| Men | Women | p * | Effect size (Cohen's d) | |||
|---|---|---|---|---|---|---|
| N (% in each category) | Mean (sd) | N (% in each category) | Mean (sd) | |||
| Overall | 2268 | 5.3 (4.8) | 2985 | 6.7 (5.1) | <0.001 | 0.28 |
| Age (years) | ||||||
| <39 | 722 (31.8) | 6.5 (4.9) | 1003 (33.6) | 8.1 (5.3) | <0.001 | 0.31 |
| 39–57 | 721 (31.8) | 5.9 (5.0) | 1049 (35.1) | 6.9 (5.0) | <0.001 | 0.20 |
| >57 | 825 (36.4) | 3.6 (4.0) | 933 (31.3) | 5.1 (4.6) | <0.001 | 0.35 |
| Marital status | ||||||
| Single | 715 (32.2) | 6.0 (4.8) | 1009 (34.7) | 7.2 (5.4) | <0.001 | 0.23 |
| With partner | 1507 (67.8) | 4.9 (4.7) | 1896 (65.3) | 6.5 (5.0) | <0.001 | 0.33 |
| Education | ||||||
| No college | 662 (31.0) | 4.7 (4.7) | 813 (28.9) | 5.9 (5.2) | <0.001 | 0.24 |
| College | 680 (31.8) | 5.6 (4.8) | 905 (32.2) | 7.3 (5.2) | <0.001 | 0.34 |
| University | 795 (37.2) | 5.6 (4.8) | 1095 (38.9) | 7.0 (4.9) | <0.001 | 0.29 |
| Income | ||||||
| Low | 554 (25.1) | 6.1 (5.1) | 873 (30.2) | 7.1 (5.5) | 0.001 | 0.19 |
| Middle | 1413 (64.1) | 5.1 (4.6) | 1787 (61.8) | 6.6 (4.9) | <0.001 | 0.31 |
| High | 236 (10.7) | 4.5 (4.8) | 230 (8.0) | 6.6 (4.9) | <0.001 | 0.43 |
| BMI | ||||||
| <18.5 | 21 (0.9) | 8.3 (7.0) | 93 (3.2) | 7.1 (5.5) | 0.634 | 0.19 |
| 18.5–24.9 | 754 (33.8) | 5.4 (4.7) | 1270 (43.1) | 6.7 (5.0) | <0.001 | 0.27 |
| 25–29.9 | 928 (41.6) | 5.0 (4.8) | 845 (28.7) | 6.4 (5.0) | <0.001 | 0.29 |
| ≥30 | 529 (23.7) | 5.5 (4.8) | 736 (25.0) | 7.2 (5.2) | <0.001 | 0.34 |
| Clinical severity | ||||||
| Mild | 955 (43.6) | 4.3 (4.3) | 1084 (37.8) | 5.9 (4.7) | <0.001 | 0.35 |
| Moderate | 883 (40.3) | 5.8 (4.9) | 1292 (45.1) | 6.9 (5.0) | <0.001 | 0.22 |
| Severe | 354 (16.1) | 7.0 (5.2) | 489 (17.1) | 8.4 (5.8) | <0.001 | 0.25 |
| Visible area | 1660 (74.1) | 5.6 (4.8) | 2150 (72.7) | 7.2 (5.2) | <0.001 | 0.32 |
| Comorbidities | 1040 (46.9) | 5.1 (4.8) | 1382 (40.5) | 6.6 (5.2) | <0.001 | 0.30 |
| Stressful event** | 887 (40.5) | 6.4 (5.2) | 1398 (47.9) | 7.7 (5.3) | <0.001 | 0.25 |
| Depression (PHQ ≥ 3) | 471 (21.2) | 8.0 (5.5) | 834 (28.5) | 9.1 (5.6) | <0.001 | 0.20 |
| Anxiety (GAD ≥ 3) | 469 (20.7) | 8.4 (5.5) | 890 (30.3) | 9.2 (5.5) | 0.016 | 0.14 |
| Stigma (PSQ ≥ 14) | 1168 (53.0) | 6.7 (5.2) | 1534 (52.6) | 8.3 (5.4) | <0.001 | 0.30 |
| VAS EQ-5D | ||||||
| ≥75 | 1183 (52.2) | 4.1 (4.1) | 1289 | 5.5 (4.6) | <0.001 | 0.32 |
| 60–74.9 | 564 (24.9) | 6.0 (4.9) | 819 | 7.0 (5.1) | <0.001 | 0.20 |
| 50–59.9 | 223 (9.8) | 6.5 (5.1) | 438 | 7.3 (5.1) | 0.058 | 0.16 |
| <50 | 298 (13.1) | 7.7 (5.3) | 430 | 9.3 (5.7) | 0.001 | 0.29 |
- Abbreviations: BMI, Body Mass Index; GAD, General Anxiety Disorder; PHQ, Patient Health Questionnaire; PSQ, Perceived Stigmatization Questionnaire; VAS EQ-5D, Visual Analogue Scale EuroQol 5-D.
- * From Mann–Whitney non-parametric test.
- ** ‘Have you had any stressful life events during the last 6 months (serious illness, death of close friend or family member, accident, divorce or other events)?’ Possible answer yes/no.
| Men | Women | p * | Effect size (Cohen's d) | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | sd | n | Mean | sd | |||
| Acne | 73 | 6.5 | 4.8 | 160 | 8.1 | 5.3 | 0.037 | 0.32 |
| Allergies/hypersensitive reactions | 54 | 3.5 | 4.2 | 62 | 4.3 | 3.0 | 0.023 | 0.22 |
| Alopecia areata | 28 | 8.0 | 5.1 | 55 | 8.9 | 5.7 | 0.512 | 0.17 |
| Alopecia (other) | 23 | 6.1 | 4.8 | 42 | 9.0 | 5.1 | 0.028 | 0.59 |
| Atopic dermatitis | 159 | 6.6 | 4.9 | 185 | 8.9 | 5.4 | <0.001 | 0.45 |
| Benign tumours | 86 | 4.1 | 4.0 | 128 | 5.8 | 4.4 | 0.003 | 0.40 |
| Bullous disorders | 66 | 5.2 | 5.5 | 72 | 4.8 | 5.2 | 0.709 | 0.07 |
| Connective tissue disease | 48 | 4.2 | 4.1 | 160 | 5.2 | 4.0 | 0.063 | 0.25 |
| Dermatitis/eczema (other) | 105 | 5.0 | 4.6 | 135 | 6.0 | 4.9 | 0.082 | 0.21 |
| Hand eczema | 25 | 5.8 | 4.7 | 46 | 4.8 | 4.6 | 0.309 | 0.21 |
| Hidradenitis suppurativa | 39 | 10.1 | 5.5 | 95 | 9.2 | 5.4 | 0.364 | 0.16 |
| Hyperhidrosis | 7 | 9.7 | 6.7 | 19 | 12.9 | 4.2 | 0.231 | 0.57 |
| Infections | 132 | 4.4 | 4.7 | 110 | 5.2 | 4.4 | 0.050 | 0.18 |
| Malignant melanoma | 46 | 3.3 | 3.6 | 51 | 5.1 | 4.3 | 0.029 | 0.45 |
| Metabolic and systemic disease | 28 | 4.5 | 4.6 | 73 | 7.3 | 6.1 | 0.033 | 0.52 |
| Nevi | 85 | 3.8 | 3.8 | 139 | 5.7 | 4.6 | 0.002 | 0.45 |
| NMSC | 219 | 2.9 | 3.5 | 222 | 4.2 | 4.0 | <0.001 | 0.35 |
| Prurigo | 52 | 4.7 | 4.3 | 74 | 6.5 | 5.1 | 0.022 | 0.38 |
| Pruritus | 52 | 4.1 | 4.0 | 56 | 5.4 | 4.3 | 0.102 | 0.31 |
| Psoriasis | 684 | 6.5 | 5.0 | 684 | 7.8 | 5.1 | <0.001 | 0.26 |
| Rosacea | 35 | 4.8 | 5.0 | 54 | 6.7 | 4.3 | 0.014 | 0.41 |
| Scaly conditions | 44 | 4.2 | 4.0 | 73 | 6.1 | 4.7 | 0.030 | 0.43 |
| Seborrheic dermatitis | 28 | 4.9 | 4.3 | 28 | 7.1 | 4.6 | 0.092 | 0.49 |
| Skin malformations | 13 | 5.1 | 3.6 | 36 | 4.8 | 4.7 | 0.509 | 0.07 |
| Urticaria | 54 | 4.0 | 3.4 | 113 | 6.3 | 5.2 | 0.016 | 0.52 |
| Venous insufficiency | 25 | 5.0 | 4.7 | 44 | 6.1 | 5.2 | 0.491 | 0.22 |
| Vitiligo | 18 | 4.8 | 5.1 | 29 | 8.5 | 5.2 | 0.012 | 0.72 |
- * From Mann–Whitney non-parametric test.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| B | Exp (B) | 95% CI | B | Exp (B) | 95% CI | |
| Age (cont.) | −0.020** | 0.980 | 0.966–0.994 | −0.023** | 0.977 | 0.967–0.987 |
| Marital status (single/married) | 0.260 | 1.297 | 0.850–1.979 | −0.011 | 0.990 | 0.743–1.319 |
| Education (cont.) | 0.274* | 1.315 | 1.025–1.687 | 0.090 | 1.095 | 0.917–1.307 |
| BMI (cont.) | −0.012 | 0.989 | 0.952–1.027 | 0.009 | 1.009 | 0.986–1.033 |
| Severity (cont.) | −0.117 | 0.890 | 0.664–1.193 | 0.115 | 1.122 | 0.913–1.379 |
| Visible flare (n/y) | −0.012 | 0.988 | 0.595–1.641 | 0.300 | 1.349 | 0.937–1.944 |
| Comorbidities (n/y) | −0.148 | 0.862 | 0.559–1.329 | −0.078 | 0.925 | 0.683–1.252 |
| Stress (PSS, cont.) | 0.077** | 1.080 | 1.041–1.120 | 0.095** | 1.099 | 1.070-1.130 |
| Stigma (PSQ, cont.) | 0.067** | 1.069 | 1.051–1.088 | 0.053** | 1.054 | 1.042-1.066 |
| Depression (PHQ, n/y) | 0.170 | 1.185 | 0.731–1.920 | 0.373* | 1.453 | 1.033-2.043 |
| Anxiety (GAD, n/y) | 0.719** | 2.053 | 1.284–3.283 | 0.090 | 1.094 | 0.774–1.547 |
| VAS health (cont.) | −0.001 | 0.999 | 0.988–1.010 | −0.004 | 0.996 | 0.989–1.004 |
- Abbreviations: BMI, Body Mass Index; CI, Confidence Interval; cont., continuous variable; GAD, General Anxiety Disorder; PHQ, Patient Health Questionnaire; PSQ, Perceived Stigmatization Questionnaire; PSS, Perceived Stress Scale; VAS, Visual Analogue Scale.
- * p < 0.05.
- ** p < 0.01.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| B | Exp (B) | 95% CI | B | Exp (B) | 95% CI | |
| Age (cont.) | −0.019 | 0.981 | 0.955–1.008 | −0.019 | 0.981 | 0.962–1.001 |
| Marital status (single/married) | 0.087 | 1.091 | 0.515–2.312 | 0.336 | 1.399 | 0.791–2.474 |
| Education (cont.) | 0.367 | 1.443 | 0.906–2.299 | 0.116 | 1.123 | 0.803–1.570 |
| BMI (cont.) | 0.071* | 1.073 | 1.001-1.150 | 0.037 | 1.038 | 0.990–1.087 |
| Visible flare (n/y) | −0.126 | 0.882 | 0.430–1.808 | 0.396 | 1.486 | 0.822–2.685 |
| Comorbidities (n/y) | −0.352 | 0.703 | 0.310–1.595 | −0.496 | 0.609 | 0.331–1.119 |
| Stress (PSS, cont.) | 0.116** | 1.123 | 1.055-1.196 | 0.097** | 1.102 | 1.045-1.162 |
| Stigma (PSQ, cont.) | 0.068** | 1.070 | 1.037-1.104 | 0.057** | 1.059 | 1.035-1.083 |
| Depression (PHQ, n/y) | 0.623 | 1.864 | 0.809–4.293 | 0.283 | 1.327 | 0.684–2.574 |
| Anxiety (GAD, n/y) | 0.171 | 1.186 | 0.511–2.754 | 0.321 | 1.379 | 0.724–2.626 |
| VAS health (cont.) | 0.020 | 1.020 | 0.993–1.047 | 0.001 | 1.001 | 0.986–1.016 |
- Abbreviations: BMI, Body Mass Index; CI, Confidence Interval; cont., continuous variable; GAD, General Anxiety Disorder; PHQ, Patient Health Questionnaire; PSQ, Perceived Stigmatization Questionnaire; PSS, Perceived Stress Scale; VAS, Visual Analogue Scale.
- * p < 0.05.
- ** p < 0.01.
DISCUSSION
In this study, we observed that, in a dermatological patient population, both body dysmorphic concerns and BDD were significantly more prevalent in women than in men. This difference was observed when considering different categories of sociodemographic, clinical and psychological variables, and in almost all participating countries. In the general population, the review by Veale et al2 reported for BDD a sex ratio of 1.27 for women to men. In dermatological populations, different studies reported a higher prevalence of BDD in women than men.14, 24. Studies reporting a higher prevalence in men usually concerned general cosmetic surgery settings and rhinoplasty settings.2
There is a growing recognition of the psychological impact of appearance-related concerns due to a skin condition. Contemporary culture, in fact, still considers flawless appearance as a sign of canonical beauty.25 Both men and women may have body concerns reinforced by adverts, popular culture and social media. Such observations relate to self-objectification theory,26 according to which people may internalize an observer perspective and treat themselves as object to be evaluated based upon appearance. Social expectations may also explain differences in body concerns in men and women. In fact, women seem to be more worried about skin-specific aspects (e.g. appearance, tone, colour and uniformity) than men, who are more focused on body build, genitals appearance, height and hair loss related to their sexual identities.3, 27, 28 The results of the present work could be also elucidated in a sociocultural perspective. According to Tiggerman,29 body appearance and body image become crucial characteristics for the self-evaluation in contemporary Western societies. This strong emphasis on appearance, in fact, is continuously prompted in a wide range of everyday activities, and a ‘normative’ body dissatisfaction mindset seems to be the only accepted way to speak and think about bodies, especially in women.
In a group of female medical students in Saudi Arabia,30 among the body features related to BDD, the skin occupied a predominant place. We can speculate that the desire to adhere to the models suggested by the mass media, and the social expectation about the physical appearance, leads people to notice every little imperfection of their body and want to change it. Evaluative behaviours involve both seeking information and making judgements about the self in relation to other, as already defined for similar phenomena by the Social Comparison Theory,31which suggests that we value our own personal and social worth by making comparisons between ourselves and others. Moreover, according to social comparison theory, individuals tend to compare themselves with others perceived as superior or inferior in term, for example, of beauty. These appearance comparisons have been established as predictors of body dissatisfaction, body-shaming, and are considered as an important mechanism in the way individuals with a stigmatized identity evaluate themselves.32
The diversity of concerns in men and women could reflect the social patterns of muscular men and thin, well-groomed women.33, 34 We can hypothesize that the difference between men and women could also depend on the fact that it is more distressing and feels more shameful for males to reveal and discuss body image concerns.
In our study, in univariate analysis, women, with few exceptions, reported more dysmorphic concerns than men in all subgroups. It must be emphasized that, since the sample is very large, statistical significance is obtained even with small differences. For this reason, we calculated the effect size, which was generally around 0.20–0.30, indicating a small to medium effect. However, the mean DCQ scores were consistently higher in women; thus, it would be fair to say that there could be a trend for women to experience more dysmorphic concerns than men.
We analysed the variables associated with BDD both in the whole sample and only in patients with mild clinical severity. In fact, in the new DSM-5 criteria,1 also patients with severe defects may be included (category Other Specified Obsessive–Compulsive and Related Disorders, Body dysmorphic-like disorder with actual flaws), and thus, we analysed the whole population independently from the severity level of the skin condition. On the other side, the main diagnosis of BDD in the DSM-51 still includes only patients without a defect or only a slight defect, which in our population may be represented by patients with a mild skin condition. In the multivariate model on the whole population, associations between BDD and the other variables differed between men and women. Indeed, in men the association was significant between BDD and education level, stress, stigma and anxiety, while in women BDD was negatively associated with age and positively associated with stress, stigma and depression. In a previous study,35 an association was observed between BDD and depression, anxiety and stress. In another study,36 53%–81% of BDD cases presented with comorbid major depressive disorder, comorbid anxiety disorders and an increased likelihood of having comorbid major depressive disorder. Suicide attempts occur in 24%–28% of individuals with BDD.37 In men and women, these associations may differ. For example, similarly to our study, in a study of a group of female students in Saudi Arabia30 no association was found between BDD and anxiety, even though it must be considered that the population was younger than ours. However, when considering only patients with mild clinical severity, the associations were the same in men and women, namely between BDD and stress, and between BDD and stigma.
Due to the cross-sectional nature of the study, we cannot establish a causal relationship between BDD and anxiety or depression, or stress. It has previously been seen38 that most persons with BDD developed major depression and substance use disorders after the onset of BDD, whereas a majority developed social phobia before the onset of BDD. Depression can result from anxiety and shame related to BDD and the resulting social dysfunction.3
Statistically significant differences in dysmorphic concern among genders, with small to medium effect size, have been reported in more than half of the observed skin conditions. The most significant difference in dysmorphic concern was observed for patients with vitiligo.
Although it is clear that differences between men and women exist regarding dissatisfaction with appearance,34, 39, 40 the psychosocial mechanisms underlying this phenomenon are not fully understood. A large number of studies indicate that psychosocial variables are likely to account for the difference.41 Moreover, recent studies suggest that interpersonal relationships, low mood and individual self-esteem may play an important role in shaping how people feel about their bodies42, 43; thus, the conditions of avoidant behaviour, isolation, depression and stigmatization typically experienced by persons with skin disease could worsen dysmorphic concerns and BDD, particularly in women. Further investigation, for example the performance of qualitative studies, is warranted to clarify the reasons for the observed gender differences in BDD.
A limitation of our study is that BDD was not diagnosed by a clinician. Also, the study population included patients who attended dermatological clinics and thus is not representative of the general population of persons with skin conditions. Another limitation is that reliability data for the clinical severity scale are not available. However, to our knowledge this is the first study investigating dysmorphic concerns and BDD in such a large population of dermatological patients.
In conclusion, body-related concerns are frequent among dermatological patients, in particular in women. Clinicians should be able to detect these concerns and their comorbidities, and adopt a holistic, multidisciplinary approach to improve the well-being of patients.
ACKNOWLEDGEMENTS
The authors are grateful to the participants who took part in the study. We would also like to acknowledge all the researchers who have assisted in collecting data.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
F. Sampogna received consultant fees from Abbvie and is Secretary General of the European Society for Dermatology and Psychiatry (ESDaP); T. Samela has no conflicts of interest to declare; D. Abeni has no conflicts of interest to declare; C. Schut received a grant from the university clinic of Giessen and Marburg, had a contract with Mahana Therapeutics, USA, received speakers honoraria from Novartis, UKM, support from the ESDaP to attend a meeting, and is board member of the German working group on psychodermatology (Arbeitskreis Psychosomatische Dermatologie) of the German Dermatological Association; J. Kupfer has no conflicts of interest to declare; A.P. Bewley received ad hoc royalties from Wiley for publication of Practical Psychodermatology, ad hoc consultancy fees and honoraria from Almirall, AbbVie, Novartis, Sanofi, UCB, Galderma, Janssen, Leo Pharma, Pfizer, BMS and Janssen, travel grants from AbbVie, Almirall, Janssen and Novartis to attend dermatology meetings, is part of the EADV UK Board Member, immediate Past President of ESDaP, and has various advisory roles within the British Association of Dermatologists; A. Y. Finlay is joint copyright owner of several quality of life questionnaires and royalties for the use of quality of life measures are paid to Cardiff University, that gives a share of these to AYF under standard university policy; U. Gieler received an educational grant from Beiersdorf GmbH Germany, consulting fees from Incyte, honoraria from AbbVie. Almirall, Incyte, Janssen, Léo Pharma, Lilly, Novartis, Pfizer and UCB, support for attending meetings from KenVIe; A.R. Thompson is Trustee for the charity Changing Faces; T. Gracia-Cazaña received grants, consulting fees and honoraria from Léo Pharma, Pfizer, Abbvie, Lilly, Novartis, Janssen, Celgene, UCB, Almirall, Dermofarm, L'Oréal and Galderma, support for attending meetings from Abbvie, Novartis, UCB, Celgene, Pfizer and Almirall, participated on advisory boards for Léo Pharma, Pfizer, Abbvie, Lilly, Novartis, Janssen, Celgene, UCB, Almirall and Dermofarm, received medical equipment from Léo Pharma, Pfizer, Abbvie, Lilly, Novartis, Janssen, Celgene, UCB and Almirall; F. Balieva has no conflicts of interest to declare; B.R. Ferreira has no conflicts of interest to declare; G.B. Jemec received grants from Abbvie, LeoFoundation, Novartis, UCB, CSL Behring, Regeneron, Sanofi, Boehringer-Ingelheim, Union therapeutics, Toosonix and Henlez, consulting fees from LeoPharma and Incyte, is copyright holder of the HISQOL, Vice President of the EHSF, chair of the CHORD, has stocks of Henlez; L. Lien has no conflicts of interest to declare; L. Misery has no conflicts of interest to declare; S.E. Marron has no conflicts of interest to declare; S. Ständer received grants from Almirall, Beiersdorf, Leo Pharma, Galderma and Sanofi, consulting fees from AbbVie, Almirall, Beiersdorf, Clexio, Escient, Galderma, Grünenthal, Incyte, IntegrityCE, Kiniksa, Klinge Pharma, Lilly, P.G. Unna Academy, Pfizer, Sanofi, TouchIME, Vifor and WebMD, honoraria from AbbVie, BMS, FomF, Galderma, LeoPharma, L'Oreal, MEDahead, Moroscience, Novartis, Sanofi, P. G. Unna Academy, Pfizer, UCB and Vifor, support for attending meetings from Lilly, Novartis, P.G. Unna Academy, Sanofi and Vifor, participation on boards for AbbVie, Almirall, Galderma, Lilly, Pfizer, Sanofi and Vifor; C. Zeidler received honoraria from Almirall, Beiersdorf, Galderma, Sanofi, Novartis and Abbvie, support for attending meetings from Almirall, Beiersdorf, Galderma and Sanofi; C. Szabó has no conflicts of interest to declare; J.C. Szepietowski received consulting fees from AbbVie, Leo Pharma, Novartis, Pfizer, Sanofi-Genzyme, Trevi, UCB and Vifor, honoraria from AbbVie, Almirall, Janssen-Cilag, Eli-Lilly, Leo Pharma, Novartis, Pfizer, Sanofi-Genzyme and UCB, support for attending meetings from Novartis and Sanofi-Genzyme, is President of the Polish Dermatological Society, and is an investigator for AbbVie, Almirall, Amgen, AnaptysBio, BMS, Boehringer Ingelheim, Celtrion, Galderma, Galapagos, Helm AG, Kliniksa, Incyte, InfraRX, Janssen-Cilag, Leo Pharma, Medimmune, Menlo Therapeutics, Merck, Novartis, Pfizer, Regeneron, UCB, Teva and Trevi; A. Reich has worked as a consultant or speaker for AbbVie, Bausch Health, Bioderma, Celgene, Chema Elektromet, Eli Lilly, Galderma, Janssen, Leo Pharma, Medac, Menlo Therapeutics, Novartis, Pierre-Fabre, Sandoz and Trevi, and participated as principal investigator or sub-investigator in clinical trials sponsored by AbbVie, AnaptysBio, Argenx, CellTrion, Drug Delivery Solutions Ltd, Galderma, Genentech, InflaRx, Janssen, Kymab Limited, Leo Pharma, Menlo Therapeutics, MetrioPharm, MSD, Novartis, Pfizer, Trevi, UCB and VielaBio; A. Svensson has no conflicts of interest to declare; I.K. Altunay has no conflicts of interest to declare; F.J. Legat received consulting fees from Almirall, Celgene, Eli Lilly, Galderma, Menlo Therapeutics, Novartis, Pelpharma, Pfizer, Sanofi, Trevi Therapeutics and Vifor Pharma, honoraria from Almirall, Celgene, Eli Lilly, Galderma, Novartis, Pelpharma, Pfizer, Sanofi and Vifor Pharma, support for attending meetings from Amgen, AbbVie, Celgene, Eli Lilly, Galderma, Janssen-Cilag, Leo Pharma, Novartis, Pelpharma, Pfizer and Sanofi; V. Grivcheva-Panovska has no conflicts of interest to declare; D.V. Romanov has no conflicts of interest to declare; A.N. Lvov received grants from Abbvie, Galderma, Pfizer, Leo Pharma, Bayer, Sun Pharma, Sanofi, L'Oreal and Teva, consulting fees from Abbvie, Pfizer and Sanofi, honoraria from Abbvie, Galderma, Pfizer, Leo Pharma, Bayer, Sun Pharma, Sanofi, LOreal and Teva; G. Titeca received grants from Léo Pharma, Novartis, Pfizer, Abbvie, Lilly, Janssen, Celgene, UCB and Almirall, consulting fees from Janssen, Novartis, Léo pharma, Celgene and Almirall, honoraria from Novartis, Pfizer, Lilly, UCB, Almirall, Celgene and Janssen, support for attending meetings from Abbvie, Novartis, UCB, Celgene, Pfizer and Almirall, participation on an advisory board for Léo Pharma, and received medical equipment from Léo Pharma, Novartis, Pfizer, Abbvie, Lilly, Janssen, Celgene, UCB and Almirall; N.C. Vulink has no conflicts of interest to declare; L. Tomás-Aragones has no conflicts of interest to declare; S. van Beugen has no conflicts of interest to declare; A.W.M. Evers received research grants from the European Research Council, Dutch Research Organisation (NOW) and Dutch health charity associations (e.g. Hartstichting, Diabetesfonds, ReumaNL and Nierstichting), is President Society for Interdiscipinary Placebo Studies, member of the supervisory board of Vrije Universiteit Amsterdam, member of the Societal Impact Team Covid and other pandemics, member of the Scientific Advisory Board of Nierstichting, Diabetesfonds, board member of the Special Interest Group (SIG) Placebo and Pain IASP, Advisory Board Member of ESDAP, board member of LVMP, PGMP, and member of KNAW and KHMW; F.J. Dalgard has no conflicts of interest to declare.
ETHICAL APPROVAL
The study was approved by the Institutional Review Board of the Department of Medicine at the University of Giessen (protocol number 87/17), and at each recruitment centre, and conducted in accordance with the Declaration of Helsinki.
ETHICS STATEMENT
All participants signed a written informed consent.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.