Changing landscape of diabetes in Asia – What are the unmet needs?
ABSTRACT
The incidence rates of type 2 diabetes among adults in Asia have been stable, but the rates in youth and young adults have increased. In territory-wide surveillance in Hong Kong, Special Administrative Region of People's Republic of China, all-cause mortality rates among people with diabetes have exhibited a declining trend in the past 15 years, with a narrowing in the mortality gap between people with and without diabetes. At the same time, the improvement in survival resulted in a changing age structure and disease profile of people with diabetes, towards an increasing proportion of older people with long diabetes duration and multi-morbidities. Reductions in event rates were not observed in the youngest age group who also had the least gains in risk factor control and uptake in organ protective drugs over time. A young age at diabetes diagnosis, associated with exposure to high glycemic burden from an early age, predicted higher risks of complications and premature mortality compared with later-onset of diabetes. People presenting with type 2 diabetes below 40 years of age were 5-fold more likely to die and their life expectancy was shortened by 8 years than age-matched counterparts without diabetes. Analysis of population-based data in Hong Kong Chinese identified hypertension followed by chronic kidney disease as the leading contributor to mortality in young people, indicating that efforts to optimize non-glycemic risk factors and organ protection are as important in young individuals as it is in the older population.
The world's population with diabetes is steadily increasing. In the latest estimate by the International Diabetes Federation in 2021, approximately 537 million people are living with diabetes globally, with 38% of them residing in the Western Pacific region1. The prevalence rate of diabetes in the Western Pacific is 11.9%, higher than the rate of 10.5% globally1. Diabetes is associated with increased risks of cardiovascular disease, kidney disease, blindness, and lower-extremity amputation, resulting in major disability and impaired quality of life. Medical conditions including infection, cancer, liver disease, and mental health disorders are emerging complications of diabetes supported by recent literature. Advances in pharmacotherapeutics, medical devices and diagnostics have promised to revolutionalize the care of people with diabetes. However, the adoption of new drugs and technology has proved to be slow, especially in low-to-middle income countries where healthcare resources are stretched. Even in high-income countries, the management of diabetes remains suboptimal, with the majority of people not meeting glucose and other metabolic targets, particularly among young people with diabetes.
The Lancet Commission on Diabetes recommended using registry and administrative data, in addition to data from randomized clinical trials, to inform decision making at the system, provider, and patient level2. Whilst registries provide disease-specific data collected systematically, administrative data are less susceptible to volunteer bias and loss to follow-up. The Commission emphasized the importance of integrating and analyzing data sources to study disease pattern and to examine how it changes over time in a population, to define areas of unmet needs for focused intervention2. Registry and administrative data are also useful to evaluate the effects of new drugs and technology in real-world settings, and to identify sub-populations most likely to benefit.
This review summarizes the epidemiology of diabetes in Asia, referencing studies in Hong Kong, previously a British crown colony later returned to the Chinese sovereignty to become a special administrative region of the People's Republic of China. Hong Kong has a dual-track healthcare system comprising private and public sectors, serving its population of 7.5 million people. Over 90% of medical services are provided by the Hong Kong Hospital Authority (HA), a statutory body that governs all the public hospitals and most of the public out-patient clinics. Since 2000, the HA has developed an electronic medical record system which was deployed territory-wide across all healthcare facilities within the HA, capturing clinical information of its attendees along their life course3. The HA clinical database is therefore representative of the profile of people living in Hong Kong, and analysis of the HA database offered the opportunity to understand the disease landscape in this population. Given the similarities in demographic, socioeconomic status, and people's culture between Hong Kong and other cosmopolitan cities in China, observations in Hong Kong can largely be applied to these settings. The HA database encompassed a wide range of clinical variables including demographic, in-patient and out-patient disease codes, procedures, laboratory results, and prescription records, allowing for the analysis of disease patterns with high granularity.
TRENDS IN INCIDENCE OF TYPE 1 AND TYPE 2 DIABETES
The time trends in the incidence of type 1 and type 2 diabetes vary. In a multi-country analysis of 24 population-based data sources including four countries or jurisdiction from Asia, approximately 80% of data sources reported a decline in the incidence of type 2 diabetes from 2010 onward4. In Hong Kong, the incidence rates of type 2 diabetes among older adults aged 40 years and above has remained largely static for the past 10 years between 2005 and 20155. Public health efforts to create a health-enabling living environment including campaigns to promote healthy eating and active lifestyle have helped to slow down the rising prevalence of adult overweight and obesity in Hong Kong. It is noteworthy that the incidence rates of type 2 diabetes remain higher in Hong Kong Chinese and in other East Asian populations compared with European White. The age- and sex-adjusted incidence rates were 949 to 1,099 per 100,000 person-year (py) in Hong Kong5, 830 per 100,000 py in Korea6, and 800 per 100,000 py in Taiwan7, but were 370 per 100,000 py in United Kingdom8 and 398 per 100,000 py in Sweden9 over comparable reporting periods. The higher rates among the East Asian population despite their leaner body habitus indicates that factors beyond general obesity contribute to the development of type 2 diabetes. The tendency for visceral fat accumulation, early insulin resistance, and defective beta-cell function are key biological processes underlying type 2 diabetes in Asians10.
In contrast to trends in older adults, increases in the incidence rate of type 2 diabetes in Hong Kong Chinese youth and young adults were observed with annual growths of 4.8–5.9% in people aged below 20 years and 3.3–4.2% in those aged between 20 and 39 years5. Type 2 diabetes accounted for more than half of the diabetes presentation in children and adolescents in Hong Kong and in other East Asian populations. In a study modeling the global incidence of type 2 diabetes in youth, China had the highest burden contributing 7,300 out of 41,600 new cases of youth-onset type 2 diabetes in 202111. In ranking the incidence rates of type 2 diabetes in youth by ethnicity and regions, the highest rates were reported from indigenous populations in Australia, Canada, and the United States (USA), followed closely by Hong Kong, Taiwan, and South Korea12. Therefore, the higher incidence rates of type 2 diabetes in East Asian adults are generalized to the youth population, calling for a more effective strategy to reduce the risk factors for type 2 diabetes from a young age and revisiting the clinical threshold to screen for abnormal glucose tolerance in this group. Maternal obesity and hyperglycemia are strongly linked to increased risks of youth-onset type 2 diabetes, contributing to 47% of type 2 diabetes in this age group13. A multi-pronged life-course approach to optimize maternal health and to reduce perinatal adversity are needed to tackle the rising rates in intergenerational transmission of diabetes.
Type 1 diabetes is more prevalent in European Whites than in East Asians14. However, recent studies showed that incidence rates of type 1 diabetes have been rising in East Asian youths15, whereas the rates in Nordic countries and the USA have stabilized in the past decade16, 17. In Hong Kong, the incidence rates of type 1 diabetes increased by 3.6–4.4% per annum in children and adolescents between 2005 and 20155. The reasons underlying the increasing trend is not immediately obvious, although environmental factors including childhood obesity, climate change, and infection have been implicated. The incidence rates of type 1 diabetes were unchanged in adults aged 20 years and above, but it is worth noting that adults comprised more than two-thirds of the type 1 diabetes population in Hong Kong. A recent study that modeled the global incidence of type 1 diabetes identified twin peaks in incidence rates with the first peak occurring in the age group 10–14 years and the second peak in people aged above 75 years18.
TRENDS IN INCIDENCE OF DIABETES-RELATED COMPLICATIONS
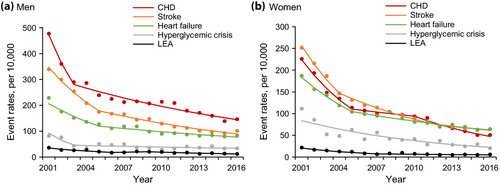
The past three decades have witnessed a major transformation in the management of people with diabetes. The first issue of Standards of Medical Care of people with diabetes released by the American Diabetes Association (ADA) in 1989 was a 4 page document without any mention of a recommended glycemic target19. The 2024 ADA guideline suggested a glycated hemoglobin (HbA1C) goal of 7% or below for most adults and 70% more time-in-range in the ambulatory glucose profile20. The recent guideline has strong emphasis on multi-disciplinary care including diabetes self-management education and support, medical nutrition therapy, physical activity, and psychosocial care. The use of statin therapy and renin-angiotensin system (RAS) inhibitors have become the standard of care since the publication of landmark trials confirming cardiovascular and kidney protection of these two drug classes20. Not surprisingly, the incidence rates of most diabetes-related complications have decreased in many parts of the world21. In a national surveillance in the USA from 1990 to 2010, age-standardized incidence rates of acute myocardial infarction, stroke, lower extremity amputation, and death from hyperglycemic crisis declined by 51–68%, whereas a smaller decline of 28% was observed for end-stage kidney disease22. A population-based study in Korea reported reduction in age- and sex-standardized incidence rates of acute myocardial infarction by 37%, ischemic stroke by 37%, and hemorrhagic stroke by 30%, from 2006 to 201323. In Hong Kong, age-standardized incidence rates of coronary heart disease, heart failure, stroke, lower extremity amputation, and hospitalization for hyperglycemic crisis declined by 59–70% in men and 66–82% in women from 2001 to 2016 (Figure 1)24. Similar to observations in the USA, however, the decrease in incidence rates of kidney failure were less pronounced compared with other diabetes-related complications. Annualized incidence rates of kidney failure, defined as the estimated glomerular filtration rate below 15 mL/min/1.73 m2 measured at least 3 months apart, decreased by 41%, whereas the rates of kidney replacement therapy have not changed during the past 16 years in Hong Kong25.
Notably, the declines in event rates were sharper in the initial one-third of the surveillance period then slowed down after mid-2000. Likewise, in the USA, improvements have plateaued with evidence of a resurgence of some events during the following 5 year period from 201026. One explanation is that the age structure and clinical profile of people with diabetes have changed over time. Improvements in survival resulted in more people with diabetes living to older ages who were more likely to accumulate multi-morbidities and at a higher risk of developing complications, especially kidney failure and heart failure. In recent years, in Hong Kong, elderly people aged above 75 years contributed two-thirds of cardiovascular diseases and over 80% of hospitalizations for heart failure24. At the same time, a decrease in age at diabetes onset with a corresponding rise in the incidence rate of young-onset type 2 diabetes led to an accumulation of individuals who were exposed to a high glycemic burden from early life with an increased life-time risk of diabetes-related complications. The expansion of diabetes pharmacotherapeutics has resulted in more options of glucose-lowering drugs including glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose co-transporter-2 (SGLT-2) inhibitors20. Although these drugs have been shown to prevent atherosclerotic cardiovascular disease, heart failure, and end-stage kidney disease in clinical trials, the impact in real-world populations with diabetes is yet to be examined.
MORTALITY TRENDS IN PEOPLE WITH DIABETES
Retrospective analysis of 16 data sources reported a decline in all-cause mortality rates in almost all regions, with regions in East Asia including Hong Kong, South Korea, Singapore and Taiwan having the largest decreases in mortality, recording annual percentage changes between −3.5% and −4.2%27. This is accompanied by decreases in standardized mortality ratios, signifying that mortality differentials between people with and without diabetes have narrowed over time in most regions, with the largest decline recorded in Hong Kong and Singapore27. The reasons for more significant improvements in regions in East Asia compared with other parts of the world are not clear but it is possible that initiatives to enhance care delivery for people with diabetes and policy changes to reduce behavioral risk factors have been more effective in this locality. In Hong Kong, at the turn of the millennium, a comprehensive diabetes assessment programme was implemented in major public hospitals to facilitate the early detection and treatment of diabetes-related complications28. In 2007, the programme, designated as the Risk Assessment and Management Programme (RAMP), was extended from secondary care to primary care setting and approximately 60% of people with diabetes attending Hong Kong HA have since participated in the RAMP. This structured care model has been shown to effectively reduce the incidence of cardiovascular disease, heart failure, end-stage kidney disease, and all-cause mortality by 57–66% in Hong Kong Chinese with diabetes29. In recent surveillance, declines were observed in mortality due to cardiovascular disease and cancer, but not pneumonia, resulting in a shift in the leading cause of death from cardiovascular disease to pneumonia, the latter contributing to one-third of all deaths in people with diabetes in 201630.
YOUNG-ONSET DIABETES IN ASIA
The incidence of young-onset type 2 diabetes is higher in Asians than in European Whites12. In a multi-national study of 41,030 people with type 2 diabetes in Asia, one in five presented before the age of 40 years31. Type 2 diabetes is also the major form of diabetes arising in Asian children and adolescents. People with young-onset type 2 diabetes have a higher lifetime risk of developing diabetes-related complications than those with a later-onset type 2 diabetes32, 33, due to a combination of longer disease exposure, poor control of blood glucose, and other metabolic risk factors in particular obesity. In a modeling analysis of HbA1c trajectories by age at diabetes diagnosis, a younger age predicted higher HbA1c values at diagnosis and a more rapid increase in HbA1c values over time34. Glycemic response to most glucose-lowering drug classes, including metformin, thiazolidinediones, sulphonylureas, and dipeptidyl-peptidase-4 inhibitors, was attenuated in younger people35. Among 5,170 Hong Kong Chinese with type 2 diabetes, indices of pancreatic beta-cell function including homeostasis model assessment of beta-cell function (HOMA2-%B) and fasting C-peptide levels were significantly lower in the group with young-onset diabetes, adjusted for sex, diabetes duration, HbA1c values, and body mass index36. Moreover, the slope of decline in HOMA2-%B across diabetes duration was steeper in the younger group, especially among those with a normal weight36. These observations alongside others indicate an accelerated loss of beta-cell function in young-onset compared with later-onset type 2 diabetes, contributing to the more adverse glycemic trajectory detected in young people36, 37.
HEALTH BURDEN OF YOUNG-ONSET TYPE 2 DIABETES
Several studies in Asia have examined the progression to diabetes-related complications in young-onset type 2 diabetes, and compared the rates of progression against later-onset type 2 diabetes. Among 111,621 Japanese men of working age followed for 4 years, diabetes conferred a 17-fold increase in the risk of coronary artery disease in the group aged 31–40 years, and the excess risk was lowered to 2.5-fold in those aged 51–60 years38. In a cross-sectional analysis of 222,773 Chinese with type 2 diabetes, a young age at diabetes onset was associated with a 91% increase in age-adjusted odds of non-fatal cardiovascular disease versus later-onset age, and the effect size attenuated when adjusted for diabetes duration39. In a prospective study of 9,506 Chinese with type 2 diabetes in Hong Kong, at the same attained age, people with young-onset disease had 48% and 35% higher risks of developing cardiovascular and kidney disease, respectively, than those with late-onset type 2 diabetes33. In this study, there was no significant difference in the rates of development of complications by age of onset when diabetes duration was accounted for. However, given the impact of aging on various biological functions including the vascular system, the observation that people with young- and later-onset type 2 diabetes have similar risks of cardiovascular and kidney disease despite a large age difference is concerning. While the incidence of diabetes-related complications increases with diabetes duration, it has been shown that younger age at diabetes onset amplified the effect of disease duration on the risk of chronic kidney disease, suggesting that young-onset diabetes accelerates kidney injury independent of disease duration40.
People with young-onset type 2 diabetes, especially those who are overweight or obese, have a worse prognosis compared with age-matched counterparts with type 1 diabetes. In a prospective study of 2,323 Chinese with diabetes diagnosed at an age below 40 years from the Hong Kong Diabetes Register followed for 9 years, the highest incidence rates of cardiovascular disease and end-stage kidney disease were observed in the overweight group with type 2 diabetes and lowest in those with type 1 diabetes41. The risk differences for clinical events between type 2 and type 1 diabetes were rendered non-significant after adjustment for metabolic risk factors, suggesting that obesity and other metabolic aberrations associated with insulin resistance are key drivers for complications41. Similarly, in another population-based cohort of 2,487 Hong Kong Chinese youth with diabetes, type 2 diabetes was associated with 1.7- and 2.0-fold excess risks of cardiovascular disease and end-stage kidney disease compared with type 1 diabetes, and the risk differential was eliminated upon correction for differences in metabolic profile42.
Up to 30% of young Asians with type 2 diabetes are not obese41. A small subset may have latent autoimmune diabetes but the majority do not an alternative etiology for dysglycemia. It has been postulated that the lean group have diminished beta-cell function but improved insulin sensitivity compared with the overweight counterparts43. Using real-world data from the Hong Kong HA, Chinese with type 2 diabetes and a BMI below 25 kg/m2 had a reduced glucose-lowering response to thiazolidinediones, an insulin sensitizer, than those with a higher BMI, although there was no differential in the treatment response to metformin by body weight35. Despite a normal weight, young people with type 2 diabetes had higher blood pressure and lipid levels than those with type 1 diabetes, accompanied by a higher incidence of cardiovascular and kidney diseases41. Hence, the lean group with young-onset type 2 diabetes appears to be intermediate between type 1 diabetes and obese type 2 diabetes with respect to metabolic profile and risk of diabetes-related complications.
Young-onset type 2 diabetes incurs a considerable burden on healthcare resources. In a study comparing 1.5 million Hong Kong Chinese with and without type 2 diabetes, people with diabetes diagnosed at age 18–39 years had a 3.5- to 4.3-fold increase in hospital bed-days, whereas the relative excess was only 1.4-fold in the oldest age group, compared with age-matched control44. Importantly, excess hospitalization associated with type 2 diabetes was not limited to traditional morbidities such as cardiovascular diseases and genitourinary diseases, but extended to hospitalization for cancer, respiratory tract diseases, digestive diseases, and mental health disorders. Mental health disorders including schizophrenia, bipolar affective disorder, and depression accounted for 38% of hospital bed-days in the youngest age group44. Co-occurrence of young-onset type 2 diabetes and mental health disorders has been reported previously45, and reflects a shared lifestyle and other environmental factors, effects of psychotropic drugs on metabolic health, and challenges in coping with diabetes self-management from an early age contributing to distress and other negative emotions.
LACK OF IMPROVEMENT IN CLINICAL OUTCOME OF YOUNG-ONSET TYPE 2 DIABETES
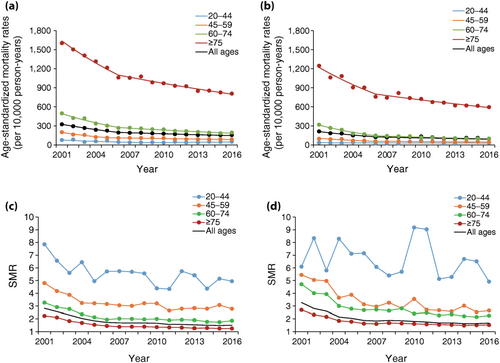
In stark contrast to the decreasing trends in incidence rates of diabetes-related complications and mortality in older population, improvements were not observed in the younger group. In Hong Kong, although the absolute mortality rates were lower in people aged 20–44 years than in older age groups, the mortality rates did not decline in young people in the recent surveillance from 2001 to 2016 (Figure 2)30. Importantly, standardized mortality ratios have also remained static, with diabetes conferring a 5-fold higher risk of mortality, which translated to approximately 8 years loss of life expectancy in the younger age group (Figure 2)30. This is accompanied by a lack of gains in the control of blood glucose and other risk factors, and a slower uptake in the prescription of organ protective drugs including statins and RAS inhibitors among young people24, 30. Current management guidelines are based on evidence generated from an older population with diabetes, as young people have been largely under-represented in most clinical trials46. It remains undetermined whether evidence from older people can be extrapolated to younger counterparts given the known differences in pathophysiology, response to treatment, and the rate of progression to diabetes-related complications between the two groups. In a multi-ethnic type 2 diabetes cohort in Asia, people with young-onset diabetes were less likely to receive pharmacotherapy for hypertension, dyslipidemia, and albuminuria than those with later-onset diabetes, and the treatment gaps were larger in women than in men31. In a study of 1,260 Hong Kong Chinese youths with type 2 diabetes followed for 9 years, the values of risk factors associated with the lowest risks of composite clinical outcomes comprising cardiovascular disease, end-stage kidney disease or all-cause mortality, were 6.5% (48 mmol/mol) for HbA1c, 117 mmHg for systolic blood pressure, and 2.2 mmol/L (85 mg/dL) for LDL-cholesterol42. These levels were lower than most recommended glycemic and metabolic targets for adults with type 2 diabetes, indicating that more stringent goals may be appropriate for a younger population. In another Hong Kong study assessing the population attributable fractions of risk factors for all-cause mortality by age groups, risk factors including high blood glucose, hypertension, high LDL-cholesterol, suboptimal body weight, smoking, pre-existing chronic kidney disease, cardiovascular disease and cancer, accounted for 52% of all deaths in the youngest group aged 18–54 years, but only 35% in people aged over 75 years47. The contribution of individual risk factors also varied by age such that hypertension was the leading risk factor in the youngest group, whilst chronic kidney disease had the largest effect size in older people. Given the greater excess mortality in the presence of risk factors in younger than in older age groups, more aggressive risk factor management especially the optimization of blood pressure from a young age could be effective in reducing premature mortality in this group.
CONCLUSIONS
In high-income regions in Asia such as Hong Kong, where there is universal health coverage, the incidence rates of diabetes-related complications and mortality have largely decreased in the past 15 years. The reduction in competing risk of mortality resulted in population aging and more people with multi-morbidities and high consumption of healthcare resources. The increasing incidence of young-onset type 2 diabetes contributed to a growing number of people who are likely to develop major complications at an age when they are most economically productive. Despite improvements in care standards, the monitoring of population-based data has revealed unmet needs in these subpopulations, where strategies tailored to their multifactorial needs are required to reduce morbidity and disability.
ACKNOWLEDGMENT
The author acknowledges the Chinese University of Hong Kong – Prince of Wales Hospital Diabetes Care and Research Team including doctors, nurses, research assistants, and administrative staff for establishment of the Hong Kong Diabetes Register, and Asia Diabetes Foundation for setting up and maintaining the Joint Asia Diabetes Evaluation database. The author also acknowledges the Hong Kong Hospital Authority for providing anonymized territory-wide data for research and publication. The current work received no funding support. A.O.Y.L. has served as a member of advisory panel for Amgen, AstraZeneca, Boehringer Ingelheim, and Sanofi and received research support from Amgen, Asia Diabetes Foundation, Bayer, Biogen, Boehringer Ingelheim, Lee's Pharmaceutical, MSD, Novo Nordisk, Roche, Sanofi, Sugardown Ltd, Takeda, outside the submitted work.
DISCLOSURE
The author declares no conflict of interest.
Approval of the research protocol: N/A.
Informed consent: N/A.
Approval date of registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.




