Correlation between hepatic venous pressure gradient and portal pressure gradient in patients with autoimmune cirrhotic portal hypertension and collateral branches of the hepatic vein
Abstract
Aim
To assess the correlation and agreement between hepatic venous pressure gradient (HVPG) and portal pressure gradient (PPG) in patients with autoimmune liver diseases (ALD) and portal hypertension, and to investigate the extent to which hepatic vein collateralization affects the accuracy of this assessment.
Methods
Ninety-eight patients with ALD between 2017 and 2021 who underwent transjugular intrahepatic portosystemic shunt with conventional and innovative 15 mL pressurized contrast were selected to measure wedged hepatic venous pressure (WHVP) and portal venous pressure and to calculate the HVPG and PPG. Pearson's correlation was used for correlation analysis between the two groups. Bland–Altman plots were plotted to estimate the agreement between paired pressures.
Results
The r values of PPG and HVPG in the early, middle, late, and portal venous visualization were 0.404, 0.789, 0.807, and 0.830, respectively, and the R2 values were 0.163, 0.622, 0.651, and 0.690, respectively. The p value for the r and R2 values in the early group was 0.015, and the p values in the remaining groups were less than 0.001. Bland–Altman plots showed that patients in the portal venous visualization group had the narrowest 95% limits of agreement. The mean value of the difference was close to the zero-scale line.
Conclusions
In patients with ALD, the correlation between the HVPG and PPG was good, and the later the collateral development, the better the correlation. Hepatic vein collateral was an essential factor in underestimating WHVP and HVPG, and the earlier the collateral appeared, the more obvious the underestimation.
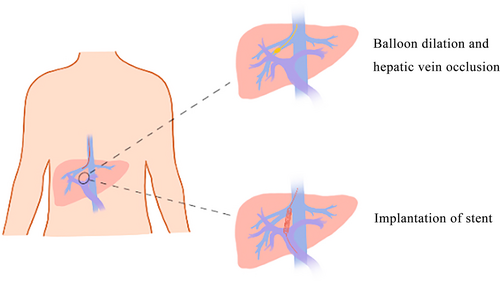
Graphical Abstract
Our study confirmed that the correlation between the wedged hepatic venous pressure (WHVP) and portal venous pressure groups and between the hepatic venous pressure gradient (HVPG) and portal pressure gradient groups was better in both triphasic shunting and portal vein visualization by innovative angiography, with the best agreement in the portal vein visualization group. Hepatic vein collateral branches were an important factor in underestimating WHVP and HVPG; the earlier the appearance of collateral branches, the more pronounced the underestimation. The absence of hepatic vein collateral veins is a crucial factor in the overestimation of the WHVP and HVPG.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interest for this article.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.