World traumatic dental injury prevalence and incidence, a meta-analysis—One billion living people have had traumatic dental injuries
Abstract
Traumatic dental injuries (TDIs) account for a considerable proportion of bodily injuries. Nevertheless, global TDI frequency is unknown, probably because TDI diagnosis is not standardized. This study estimated world TDI frequency. A literature search (publication years 1996-2016) was aimed at covering as many countries, communities, ethnic groups as possible, thus achieving high generalizability. In particular, non-specific keywords, no language restrictions, and large databanks were used. Observational studies reporting proportions of individuals with at least one TDI (prevalence) and who developed TDI (incidence rate) were considered. Prevalence rates to permanent dentition, primary dentition and in 12-year-olds, incidence rate to any tooth for any age, male-to-female prevalence ratio (PR) in 12-year-olds, with 95% confidence intervals (95 CIs), were extracted/calculated. Study quality, Z-score distribution, funnel plot symmetry analysis, between-study heterogeneity, sensitivity, and subgroup analyses were performed. Selected primary studies were 102 (permanent dentition; 268 755 individuals; median age, 13.8 years), 46 (primary dentition; 59 436 individuals; median age, 3.4 years), 42 (12-year-olds; 33 829 individuals), 11 (incidence rate; 233 480 person-years; median age, 7.8 years), and 31 (PR; 16 003 males, 16 006 females). World TDI frequency resulted as follows: permanent dentition prevalence 15.2% (95 CI, 13.0%-17.4%); primary dentition prevalence 22.7% (95 CI, 17.3%-28.7%); 12-year-olds prevalence 18.1% (95 CI, 15.3%-21.0%); incidence rate, 2.82 (95 CI, 2.28%-3.42%) per 100 person-years; PR, 1.43 (95 CI, 1.34%-1.52%). Differences between WHO Regions were found. This study shows that more than one billion living people have had TDI. TDI is a neglected condition which could rank fifth if it was included in the list of the world's most frequent acute/chronic diseases and injuries.
1 INTRODUCTION
Traumatic dental injuries (TDI) are very frequent in the society and comprise 85% of patients presenting with injuries to the oral region,1 although the oral region comprises as small an area as 1% of the total body area, oral injuries account for 5% of all bodily injuries in all ages, and in pre-school children the proportion is as high as 17%.2 For example, according to a national US survey, one in four individuals aged 6-50 years had evidence of TDI.3 In the UK, one in five children have experienced TDI to their permanent anterior teeth before leaving school.4 In a literature review, Glendor concluded that in the primary dentition one-third of all children sustained a TDI, while in the permanent dentition one-fourth of all schoolchildren and one-third of all adults sustained TDI.5 Prospective studies also report high incidence rates. Namely, a Danish study, where all dental injuries occurring from birth to the age of 14 years were carefully registered, demonstrated that 30% of children had sustained injuries to the primary dentition and 22% to the permanent dentition. Altogether, every child had sustained a TDI by the age of 14 years.6 An Australian study found an incidence rate of 20 TDI per 1000 individuals per year in children aged 6-12 years.7 Two large Swedish studies extended over several years reported incidence rates of 19 to 29 events per 1000 individuals per year,8 and an annual incidence rate of 28%,9 respectively.
Thus, although TDI prevalence and incidence are generally high worldwide, they may vary considerably. Such a variation reflects not only socioeconomic, behavioral, and cultural diversity,5 but also the lack of standardized TDI registration and classification systems observed in the literature.10 It is probably for this reason that world TDI frequency is unknown and TDI was not included in the list of the 300 most important acute and chronic diseases and injuries provided by the Global Burden of Disease (GBD) Study.11
To close this important gap in knowledge between TDI and all other acute and chronic diseases and injuries, this study was aimed at providing reliable global estimates of TDI prevalence and incidence rates for primary and permanent teeth, through a systematic literature review and a meta-analysis of observational studies.
2 MATERIALS AND METHODS
The assumption underlying the meta-analysis methodology is that there is a population of studies investigating a given issue, some published and some unpublished, and the meta-analysis works on an accurate sample of studies extracted from this population.
Unlike conventional meta-analyses that investigate effect sizes and involve two variables, meta-analyses of disease frequency involve just one variable. One of the main problems of conventional meta-analyses is the control of small-study effect (ie, small studies reporting nonsignificant effect sizes are not published or are published by local journals) and the consequent publication and selection biases. Thus, study search is crucial and keyword selection and matching are important aspects of this process.12, 13 These issues are relatively simpler in meta-analyses of disease frequency, because there are just two terms to match, namely, the disease and the measure of disease frequency. However, these meta-analyses yield other important problems. Namely, there are different sources of disease frequency, such as epidemiologic studies, as in conventional meta-analyses, disease registries, and population surveys, that provide different frequencies for the same underlying population. In addition, epidemiologic study search provides totally or partially duplicated papers and the choice of the most accurate version is often difficult.14 Another problem is that while the effect size in conventional meta-analyses is normally distributed, disease frequency is binomially distributed (ie, disease present/absent), and studies reporting prevalence close to 0 or 1 yield artificially higher meta-analysis weights than studies reporting prevalence close to 0.5. This problem requires the transformation of binomially distributed variables into normally distributed variables.15
Another problem, common in meta-analyses, is whether there is a single true underlying disease frequency or a population of frequencies, which vary among different countries, due to different TDI risk factor distributions across the world.16-18 In the latter case, the global TDI frequency equals to the mean of the underlying TDI frequencies among different communities and its assessment requires that primary studies are collected from as many countries, communities, and social contexts, as possible. A prerequisite which makes these global estimates feasible is therefore to gather as many primary studies as possible carefully excluding studies with partially or totally overlapping results. If this condition is satisfied, the impact of missing studies and publication/selection bias on meta-analysis reliability would be low.16, 18
According to the GBD methodology, the data sources for the assessment of incidence and prevalence are disease registries (new cases reported by physicians and laboratories), population surveys (nation-based surveys which provide self-reported information), healthcare facility data (diagnosed cases reported on consultation), and not merely epidemiologic studies as in conventional meta-analyses.19
As for TDI registries and population surveys, data were searched by two authors (AL, GU) through the websites of the scientific societies of disciplines such as dental traumatology, pediatric dentistry, endodontics, oral-maxillofacial surgery. GOOGLE and Yahoo! were considered as web services providers. Two groups of keywords were matched, namely “Association,” “Society,” “Organization” AND “Dental Traumatology,” “Paediatric Dentistry,” “Endodontics,” “Oral-maxillofacial Surgery.” In addition, the websites of important public health organizations, namely the World Health Organization and the US Centres for Disease Control and Prevention, were considered.
According to the GBD methodology, healthcare facility data are unreliable and were not considered.
As for epidemiologic studies, a literature search was undertaken trying to locate the highest possible number of primary studies from different countries and to minimize publication and selection biases. The search was limited to the years 1996-2016. Although this option led to the exclusion of classic studies published before 1996, it was justified by the fact that the improvement of TDI surveillance systems, the dissemination of public awareness campaigns in some countries, the implementation of prevention policies in high-risk settings, such as during sports playing or at school, could have drastically changed TDI frequency in many countries. In addition, the improvement of databases during the last decade made available the gray literature, that is, informally published material, such as studies published by local scientific journals or in languages different from English, theses, congress proceedings, etc., published after the nineties.
There was no language restriction and at least one broad data bank that could help locate congress proceedings and doctoral theses was considered. The databanks used were PubMed, Scopus, Web of Science, and GOOGLE Scholar. Non-specific keywords were chosen (Unpublished Material 1—available upon request to the correspondig author). As for GOOGLE Scholar, papers were sorted in order of relevance and only the 500 most relevant titles were considered. “GOOGLE Translate” was used to handle articles published in languages other than English.
Data search was performed by one author (PS), an expert in meta-analysis of observational studies, who also screened titles and abstracts of the identified studies. Full texts of the studies that could fall into the inclusion criteria were searched. Eligibility, a key issue in meta-analyses of disease frequency, was assessed by the three authors together.14 Studies reporting overlapping results and studies which did not fall into the inclusion criteria were excluded. More specifically, duplication was suspected when the studies had at least one author in common and were performed in the same country and setting, and when age and gender distributions were similar. If necessary, the corresponding authors were contacted to ask whether study samples overlapped.
Corresponding authors of eligible studies that reported incomplete information were also contacted to seek missing data, particularly when studies were from under-represented countries. Reference lists from full texts were also checked.
Study inclusion/exclusion criteria were the following:
- Data sources: As for disease registries and population surveys, only national data and data covering at least 10 000 people at risk that were provided by important scientific societies were eligible. As for the epidemiologic studies, only observational studies that did not artificially over-estimate TDI prevalence or incidence were considered, that is, population-based studies, cross-sectional studies, and cohort studies, while case-control studies and case series were not considered. Non-original studies, such as systematic reviews, editorials, and commentaries, were excluded. Also excluded were studies which reported results that were already, totally or partly, reported by other studies. Analytical cross-sectional studies and baseline examinations of cohort studies were considered to assess the differences between males and females, while cohort studies were used for the assessment of both incidence and prevalence (baseline examination data).
- Setting: Any setting was eligible. Hospital-based studies also were considered, but those performed in emergency and traumatology services, where TDI frequency could be artificially higher, were not considered.
- Sampling method: Any method was considered acceptable, such as randomized, stratified, consecutive, and convenience samples.
- Participation rate: Studies with rates lower than 60% were not considered.
- TDI diagnosis: The outcome of this study was the frequency of individuals with at least one TDI, irrespective of injury severity, and the number of injured teeth. For this reason, all the TDI classification criteria reviewed by Feliciano et al10 were considered. The diagnostic criteria had to be clearly provided and examiners had to be trained and/or calibrated to ensure the highest possible level of diagnostic reliability.
The outcomes considered in this study were as follows:
- TDI prevalence and 95% confidence interval (95 CI) to permanent dentition.
- TDI prevalence and 95 CI to primary dentition.
- TDI prevalence and 95 CI among 12-year-old subjects (tolerance ±1 year).
- TDI incidence rate and 95 CI to any tooth and for any age.
- TDI prevalence ratio and 95 CI among males and females aged 12±2 years.
Prevalence was expressed as percent of individuals with at least one TDI, incidence rate as number of new TDI per 100 persons per year, prevalence ratio as ratio between prevalence in males and prevalence in females with females considered the unexposed group.
If prevalence, incidence rate, and prevalence ratio were not directly provided, they were calculated. If information was incomplete, the corresponding authors were contacted, and if they did not reply/provide the requested information, the study was excluded.
Data were extracted or calculated by one author (PS) and checked by the remaining authors (AL, GU). Disagreements between authors were reconciled through discussions.14
As anticipated, for every investigated TDI frequency measure the null hypothesis was that there was a single global TDI frequency and the observed differences across studies were due to sampling error. The alternative hypothesis was that there was a population of TDI frequencies and the global estimate was the mean of the underlying frequencies. The choice between the two hypotheses was pivotal in the present meta-analysis and was therefore accurately investigated.
For each outcome measure, the Z scores were calculated from all primary studies and frequency distribution was plotted. Ideally, the null hypothesis was acceptable if frequency distribution was normal, with mean 0.0 and standard deviation 1.0. If mean and/or standard deviation were far from these values, the distribution was considered not normal and the null hypothesis was rejected.18
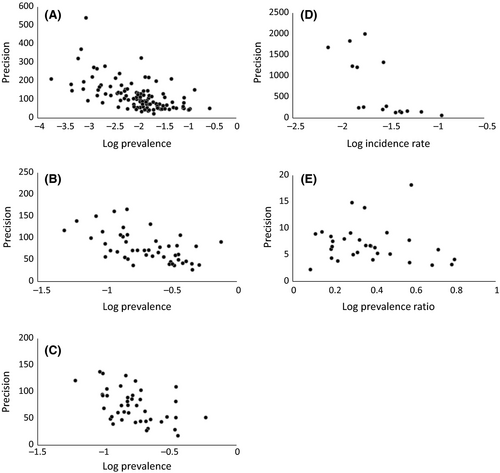
The analysis of funnel plots also was considered to investigate the underlying hypothesis. Indeed, funnel plot asymmetry is not only a symptom of publication bias, but could be due to true differences in TDI frequency between studies in accordance with the alternative hypothesis. Thus, in the present meta-analysis, funnel plot symmetry was considered supporting the null hypothesis.12, 20 For each outcome measure, a funnel plot was drawn with the logarithm of TDI frequency in the x-axis and precision, that is, the inverse of the standard error of the frequency estimate in the y-axis. Funnel plot asymmetry was investigated through formal tests, namely the tests of Begg and Mazumdar21 and Eggeret al.20
Finally, the I2 test, with formula I2 = 100 × {[Q-(k-1)]/Q}, where Q was the Cochran's Q, a χ2 test with (k−1) degrees of freedom and k the number of included studies, was also performed. The I2 test describes the percentage of total variation across studies that is due to heterogeneity rather than chance.17
For each TDI frequency outcome measure, the meta-analytic model was chosen on the basis of the cumulative analysis of Z-score distribution, funnel plot symmetry, and I2 test. If the majority of these analyses suggested that primary studies were homogeneous enough, the null hypothesis was accepted, the global TDI frequency was assumed to be the same across different studies, and the fixed-effects model was used to estimate the pooled TDI frequency. If primary studies were regarded as heterogeneous, the null hypothesis was rejected, the global TDI frequency was assumed to be the mean of the TDI frequencies, and the random-effects model was used.
As anticipated, prevalence and incidence rate were binomially distributed. Consequently, the pooled confidence intervals could include implausible values lower than 0 or higher than 1. In addition, when proportions are close to 0 or 1, the variances of these studies are squeezed toward 0 and the weights toward infinity. Thus, these studies yield artificially higher impact on the meta-analysis results than the remaining studies. To overcome these problems, the double arcsine transformation of prevalence and incidence rate values was adopted following the GBD protocol.15
The summary measures chosen in this study were TDI prevalence to permanent teeth, prevalence to primary teeth, prevalence among 12-year-old children, incidence rate, and male-to-female prevalence ratio.
To investigate the reliability of the world estimates and to check whether a single country had an excessive impact on the estimates, a different approach to meta-analysis was also adopted. Namely, the pooled TDI frequency estimates for each single WHO region were considered as units and were meta-analyzed with the inverse-variance weighting method.
An uncertainty analysis was also performed. Estimates of disease frequency, which extrapolate from specific epidemiologic studies to population-level measures, are subject to a broad range of uncertainty.14 Uncertainty around the world TDI frequency estimates could arise from several sources. The first is incomplete information, as the estimates are necessarily based on observations from samples that yield random error. The assessment of the confidence intervals for the pooled prevalences and incidence rates accounts for this kind of uncertainty.22
Uncertainty is also due to systematic error that, in turn, could be due to biases of primary studies regarding TDI assessment (diagnostic bias) and representativeness of the selected sample (selection bias). In addition, the problem of representativeness may affect the global estimates, as some countries could be under- or over-represented.22
Formally assessing susceptibility to bias of observational studies is not easy, as there are almost one hundred quality assessment tools, but none of them are rigorously developed, evidence-based, valid, reliable, and easy to use at the same time. In particular, none of these tools were designed to assess the quality of prevalence/incidence studies.23 To overcome this problem, only studies with moderate-to-high quality were included in the study set. More specifically, studies had to acknowledge items 1, 2, 4, and 5 of the abovementioned inclusion criteria. For this purpose, the Newcastle-Ottawa scale (NOS), previously adapted for cross-sectional studies,24 was further adapted to disease frequency studies.25 Namely, scores could range between 0 and 5, based on the following items:
- Case definition (score 1, use of an acknowledged TDI classification system).
- Sample selection (score 1, randomized or randomized-cluster samples).
- Sample size (score 1, size large enough to minimize the standard error, ie, 265 subjects assuming 20% prevalence and 10% 95 CI at 95% level of significance).
- Reliability of diagnosis (trained and/or calibrated examiners).
- Response rate (60% or higher).
Study quality was considered fair-to-good for scores ≥3. Common methods for incorporating risk of bias assessments into the synthesis process include sensitivity analysis, narrative assessment, and restriction of the analysis to studies at lower risk of bias.26 In this study, the third option was chosen and poor quality studies with scores 0-2 were excluded from the analysis.
The problem of over- and under-represented countries and communities was difficult to overcome, as the number of reliable data sources for injuries is extremely poor. Indeed, the GBD study globally identified nearly 6600 data sources for communicable, maternal, perinatal, and nutritional conditions (group I diseases), 1500 sources for non-communicable diseases (group II diseases), and only 18 sources for injuries (group III diseases).19, 22, 27
To assess the overall quality of this meta-analysis, the uncertainty level of at least one of the global estimates assessed in this study was compared to a global estimate assessed using the GBD data.14 According to the GBD injury group, the mortality rate due to injury was considered the most reliable information regarding group III diseases for obvious reasons. In addition, the death-to-incidence ratio was assessed using specific studies and was considered reasonably consistent. Using these data, the group estimated the incidence rates and the 95% uncertainty intervals for the various injuries.27, 28 The GBD injury study group considered the bodily injuries (ie, Chapter XIX Sections S00-T98 and Chapter XX Sections V01-Y98 of the International Classification of Diseases 10) that warrant healthcare assistance and did not consider TDI.28 Therefore, in the present uncertainty analysis, a procedure was used to adapt the uncertainty analysis of the GBD injury group to TDI. First, the global number of incident bodily injuries that warrant healthcare assistance reported for the year 2013 by the GBD injury study with the 95% uncertainty interval was extracted summing up the number of incident injuries warranting inpatient admission and the number of those warranting other types of healthcare.28 Second, the study of Petersson and colleagues, the most reliable and well-designed study on any injury, bodily and dental, that warrant healthcare assistance performed in Västmanland (Sweden) during one year,2 was used to assess the number of bodily injuries that occur for every TDI with 95 CI, as the ratio between the proportion of bodily injuries and the proportion of TDI. Third, the global number of incident TDI that warrant healthcare assistance accounting for uncertainty was estimated as the ratio between the global number of incident bodily injuries with 95% uncertainty interval and the number of bodily injuries occurring for every TDI with 95 CI.
This number was compared to the global number of incident TDI estimated using the results of the present meta-analysis. According to the aforementioned study of Petersson and colleagues, TDI incidence is stable from birth to 20 years of age and 90% of all TDI occur before this age.2 Therefore, the global number of incident TDI occurred before the age of 20 years was assessed multiplying the world population count aged 0-19 years in the year 2013 with the pooled incidence rate assessed using only studies regarding TDI that warrant healthcare assistance with 95 CI and referring to subjects aged 1-19 years. The global number of all incident TDI occurred in 2013 at any age was assessed multiplying this value by 10/9.
These two estimates were compared using 95% uncertainty/confidence intervals. If the two intervals partly overlapped, then the levels of uncertainty of the two estimates were non-significantly different. If they did not, the present estimate yielded a higher degree of uncertainty than the GBD injury study.
Sensitivity analysis to study inclusion was performed to investigate whether the pooled frequency estimates were influenced by a single study. For every meta-analysis, the contribution of each study to the overall weight was measured as percent of the total weight. Studies which yielded weights ≥10% could excessively influence the pooled estimates and were excluded in turn. The pooled TDI frequency was re-estimated and compared with the overall estimate. If the two 95 CIs overlapped, the pooled estimate was regarded as robust enough.18
Sensitivity analysis to low-quality study inclusion was also performed excluding low-quality studies that were necessarily included to cover under-represented areas and countries.
Subgroup analysis was one of the aims of this study. The primary studies were split according to countries into six subsets corresponding to the World Health Organization (WHO) Regions, namely European Region, Region of the Americas, West-Pacific Region, South-East Asia Region, Eastern Mediterranean Region, and African Region. For every Region, the pooled TDI frequencies were estimated.
The statistical analyses were performed using StatView 5.0.1 (SAS Institute Inc., NC, USA) and MedCalc 14.8.1 (MedCalc Software BVBA, Ostend, Belgium). The level of significance was α = 0.05.
The PRISMA statement for reporting meta-analyses was acknowledged.29
3 RESULTS
The study search was completed on December 29, 2016.
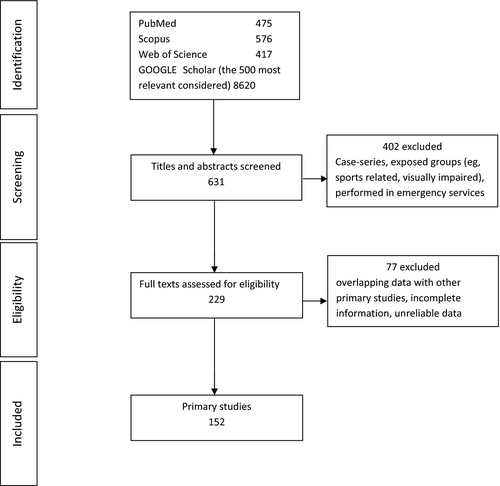
No disease registers and population surveys covering at least 10 000 people were detected. As for epidemiologic studies, among the 631 titles and abstracts screened, 229 full texts were potentially eligible and 77 of them were excluded for various reasons, thus leaving 152 primary studies (Figure 1). Of these, 102 studies were considered for TDI prevalence to permanent teeth1, 7, 9, 30-128 (Unpublished Material 2), 46 for TDI prevalence to primary teeth9, 36, 45, 129-171 (Unpublished Material 3), 42 for TDI prevalence among 12-year-old children31-34, 48-53, 55, 56, 61, 63, 64, 72, 77-79, 81, 83-85, 89, 91, 93-95, 99, 106, 107, 109, 111, 112, 116, 118, 121-123, 125, 126 (Unpublished Material 4), 11 for TDI incidence rate9, 45, 134, 172-179 (Unpublished Material 5), and 31 for male-to-female TDI prevalence ratio31-34, 43, 49-53, 55, 61, 63, 75, 77-79, 81, 85, 89, 94, 95, 105, 113, 116, 118, 121-123, 125, 126 (Unpublished Material 6). Many studies were considered for more than one purpose. The study set covered all the WHO Regions and 39 countries globally (Albania, Australia, Belgium, Brazil, Canada, China, Cuba, Egypt, Finland, Georgia, India, Iran, Iraq, Ireland, Israel, Italy, Jordan, Kuwait, Lesotho, Malaysia, Nigeria, Palestine, Peru, Poland, Romania, Russia, Saudi Arabia, South Africa, Spain, Sudan, Sweden, Switzerland, Syria, Taiwan, Thailand, Turkey, UAE, UK, US). Brazil was the most represented country followed by India and Turkey.
All the included studies yielded modified NOS ranging between 3 and 5. Indeed, the items “Case definition,” “Reliability of diagnosis,” and “Response rate” were always satisfied; the item “Sample size” was satisfied by all studies excluding seven;47, 64, 117, 120, 122, 134, 160 some studies also satisfied the item “Sample selection” (Unpublished Material 2-6). Several diagnostic classification systems were adopted (Table 1), and the most frequent was Andreasen's/WHO classification (49.3%) followed by O'Brien's classification (24.3%).
| Classification system | Number of studies | Frequency distribution (%) |
|---|---|---|
| Andreasen | 75 | 49.3 |
| Ellis | 7 | 4.6 |
| Garcia-Godoy | 5 | 3.3 |
| O'Brien | 37 | 24.3 |
| Sgan-Cohen | 3 | 2.0 |
| Others | 25 | 16.4 |
Overall, the Z scores of the primary studies were not normally distributed (Unpublished Material 7). Although the means of all the investigated parameters, excluding male-to-female prevalence ratio, were close to zero, the standard deviations were far from the value one. Funnel plots (Figure 2) were only partly symmetrical. In particular, those regarding TDI prevalence to permanent teeth and TDI incidence rate were skewed to the right (Figure 2). The funnel plot symmetry tests were not concordant. Indeed, according to the test of Begg and Mazumdar, there was significant asymmetry regarding prevalence in 12-year-old children, incidence rate, and prevalence ratio, while according to the test of Egger et al, there was significant asymmetry regarding prevalence to permanent teeth, prevalence to primary teeth, and prevalence in 12-year-old children (Unpublished Material 8). Finally, the I2 tests showed that between-study inconsistency was 97.9%-99.6% among TDI prevalence and incidence studies, while it was 40.7% among male-to-female prevalence ratio studies (Tables 2-6). Although these results were not concordant, the majority of them suggested to reject the null hypothesis of a single TDI frequency for all the five investigated parameters. This led to the use of the random-effects model.
| WHO Region | Number of subjects | I2 test (%) | Prevalence (%) | 95% Confidence interval |
|---|---|---|---|---|
| World | 268 755 | 99.6 | 15.2 | 13.0-17.4 |
| European Region | 62 389 | 99.6 | 14.0 | 9.8-18.9 |
| Region of the Americas | 53 080 | 98.4 | 19.1 | 16.4-21.9 |
| Western Pacific Region | 79 177 | 99.9 | 9.9 | 1.9-23.2 |
| South-East Asia Region | 41 922 | 98.8 | 12.2 | 9.4-15.4 |
| Eastern Mediterranean Region | 17 392 | 98.9 | 16.0 | 11.1-21.7 |
| African Region | 14 795 | 97.3 | 11.1 | 7.9-14.8 |
- Age (mean of medians). World, 13.80; European Region, 13.17; Region of the Americas, 14.58; Western Pacific Region, 12.13; South-East Asia Region, 14.86; Eastern Mediterranean Region, 12.42; African Region, 12.17.
- Sensitivity analysis: World pooled estimate excluding the low-quality studies which did not fully meet the inclusion criteria (Eyuboglu et al57; Locker1; Quaranta et al102; Stockwell7): Number of subjects 183 562; I2 test = 99.1%; Prevalence, 15.4% (95% confidence interval, 13.7%-17.3%). World pooled estimate excluding the study with relative weight>10% (Stockwell7; relative weight 64%): Number of subjects 202 255; I2 test = 99.2%; Prevalence, 15.3% (95% confidence interval, 13.6%-17.1%).
| WHO Region | Number of subjects | I2 test (%) | Prevalence (%) | 95% Confidence interval |
|---|---|---|---|---|
| World | 59 436 | 99.6 | 22.7 | 17.3-28.7 |
| European Region | 21 869 | 99.7 | 14.2 | 6.0-25.0 |
| Region of the Americas | 28 736 | 99.0 | 26.5 | 21.5-31.8 |
| Western Pacific Region | – | – | – | – |
| South-East Asia Region | 3312 | 99.9 | 27.0 | 0.0-79.3 |
| Eastern Mediterranean Region | 2052 | 97.3 | 22.7 | 12.0-35.6 |
| African Region | 3467 | 98.1 | 22.7 | 13.3-33.7 |
- Age (mean of medians). World, 3.40; European Region, 3.63; Region of the Americas, 3.07; South-East Asia Region, 4.33; Eastern Mediterranean Region, 4.67; African Region, 3.17.
- Sensitivity analysis: World pooled estimate excluding the low-quality study which did not fully meet the inclusion criteria (Al-Majed et al36): Number of subjects 59 082; I2 test = 99.6%; Prevalence, 22.5% (95% confidence interval, 17.0%-25.6%). World pooled estimate excluding the study with relative weight > 10% (Rhouma et al162, relative weight 92%): Number of subjects 47 436; I2 test = 99.2%; Prevalence, 23.5% (95% confidence interval, 19.4%-27.9%).
| WHO Region | Number of subjects | I2 test (%) | Prevalence | 95% Confidence interval |
|---|---|---|---|---|
| World | 33 829 | 97.9 | 18.1 | 15.3-21.0 |
| European Region | 1693 | 0.0a | 13.5 | 11.9-15.1 |
| Region of the Americas | 14 968 | 98.0 | 22.1 | 17.4-27.1 |
| Western Pacific Region | 1630 | 91.3 | 13.3 | 7.6-20.2 |
| South-East Asia Region | 8133 | 99.0 | 15.8 | 8.6-24.8 |
| Eastern Mediterranean Region | 2269 | 65.3 | 14.9 | 12.3-17.8 |
| African Region | 5136 | 94.3 | 13.2 | 9.4-17.4 |
- Sensitivity analysis: World pooled estimate excluding the study which included 14-year-olds (Chen et al50). Number of subjects 32 629; I2 test = 98.0%; Prevalence, 18.1% (95% confidence interval, 15.2%-21.2%). None of the studies yielded relative weights higher than 10%.
- a Fixed-effects model due to nonsignificant Q test at 95% level.
| Person-years | I2 test (%) | Incidence ratea | 95% Confidence interval | |
|---|---|---|---|---|
| Overall | 233 480 | 98.2 | 2.82 | 2.28-3.42 |
| Permanent teeth | 140 416 | 97.5 | 2.75 | 2.09-3.49 |
| Primary teeth | 43 968 | 97.7 | 2.72 | 1.65-4.04 |
| Follow-up examinations | 4046 | 92.6 | 5.19 | 2.75-8.33 |
| Public Dental Healthcare Reports | 208 658 | 98.4 | 2.51 | 1.99-3.09 |
- Sensitivity analysis: World pooled estimates excluding the studies with relative weights > 10%. Skaare and Jacobsen176; relative weight 26%: Number of subjects 162 680; I2 test = 98.3%; Incidence rate, 3.0% (95% confidence interval, 2.3%-3.7%). Skeie et al178; relative weight 18%: Number of subjects 21 2704; I2 test = 97.7%; Incidence rate, 3.0% (95% confidence interval, 2.5%-3.6%). Borssén and Holm45; relative weight 11%: Number of subjects 185 368; I2 test = 97.3%; Incidence rate, 2.8% (95% confidence interval, 2.3%-3.4%). Glendor et al174; relative weight 22%: Number of subjects 192 022; I2 test = 98.1%; Incidence rate, 3.0% (95% confidence interval, 2.4%-3.7%).
- a Events per 100 persons per year.
| WHO Region | Males | Females | I2 test (%) | PR | 95% Confidence interval |
|---|---|---|---|---|---|
| World | 3434/16003 | 2401/16006 | 40.7 | 1.43 | 1.34-1.52 |
| European Region | 184/1294 | 127/1330 | 0.0a | 1.48 | 1.20-1.83 |
| Region of the Americas | 1958/8339 | 1461/8686 | 36.5a | 1.41 | 1.33-1.49 |
| Western Pacific Region | 147/888 | 94/742 | 48.9a | 1.32 | 1.04-1.68 |
| South-East Asia Region | 751/3022 | 457/2999 | 63.3 | 1.53 | 1.17-2.01 |
| Eastern Mediterranean Region | 205/1041 | 132/940 | 0.0a | 1.43 | 1.17-1.74 |
| African Region | 189/1419 | 130/1309 | 0.0a | 1.31 | 1.06-1.62 |
- Sensitivity analysis: World pooled estimate excluding the study with relative weight > 10% (Marcenes et al81, relative weight 11%): Number of subjects M 3217/15 680, F 2236/15 677; I2 test = 40.8%; PR, 1.43 (95% confidence interval, 1.34-1.54). World pooled estimate excluding the study with relative weight > 10% (Dame-Teixeira et al53, 2013, relative weight 10%): Number of subjects M 3120/15 233, F 2184/15 284; I2 test = 42.6%; PR, 1.46 (95% confidence interval, 1.39-1.53). World pooled estimate excluding the study with relative weight > 10% (Malikaew et al77, relative weight 17%): Number of subjects M 2834/14 679, F 2047/14 605; I2 test = 10.9%; PR, 1.39 (95% confidence interval, 1.32-1.47).
- a Fixed-effects model due to nonsignificant I2 test at 95% level.
Globally, 268 755 individuals were included in the analysis regarding the assessment of the pooled TDI prevalence to permanent teeth. Age ranged between 7 and 98 years (Unpublished Material 2), and the mean of the medians was 13.8 years. Global prevalence was 15.2% (95 CI, 13.0%-17.4%; Table 2). No statistically significant difference was found between WHO Regions. However, the highest prevalence was reported in the Region of the Americas (19.1%) and the lowest in the Western Pacific Region (9.9%). Although the study of Stockwell7 was published in 1988, it was considered in the Western Pacific Region because primary studies published between 1996 and 2016 were not enough to get a reliable pooled estimate. TDI was self-reported in the studies of Quaranta102 and Locker,76 while the study of Eyuboglu57 was performed in a dental clinic. These studies were not excluded from the set because they were based on samples exceeding 10 000 individuals and yielded modified NOS of 3. In any case, the sensitivity analysis performed excluding these three studies and the study of Stockwell7 had minimal impact on the pooled prevalence estimate.
The analysis of TDI prevalence to primary teeth was assessed on 59 436 individuals globally. The mean of the median ages was 3.4 years (Unpublished Material 3). Overall prevalence was 22.7% (95 CI, 17.3%-28.7%; Table 3). There were not enough data for the prevalence in the Western Pacific Region. The highest rate was found in the South-East Asia Region (27.0%) and the lowest in the European Region (14.2%). The study of Al-Majed36 was performed on male subjects only, but yielded NOS 4 and its exclusion did not significantly change the results of the meta-analysis. Similarly, the exclusion of the study of Rhouma162 that yielded a relative weight higher than 10% did not affect the pooled prevalence estimate significantly.
The pooled TDI prevalence in children aged 12±1 years was based on 33 829 individuals. Overall prevalence was 18.1% with a narrow confidence interval (95 CI, 15.3%-21.0%; Table 4). The highest rate was reported in the Region of the Americas (22.1%), while the lowest was in the African Region (13.2%). The study of Chen50 also included 14-year-old children, but its exclusion did not produce significant changes in the pooled prevalence estimate.
There were 233 480 individuals considered to assess the pooled TDI incidence rate. Ages varied between 0 and 19 years (Unpublished Material 5) with a mean of median ages of 7.8 years. The global incidence rate was 2.82 events per 100 persons per year (95 CI, 2.28%-3.42%; Table 5). There was no difference between rates to permanent and primary teeth. An important difference was reported between rates assessed through cohort studies, based on follow-up examinations of cohorts, and through population-based studies, which reported the records collected at public dental healthcare centers. Indeed, incidence rates were 5.19 (95 CI, 2.75%-8.33%) and 2.51 (95 CI, 1.99%-3.09%), respectively. Although this difference was not statistically significant, it suggested that roughly one half of incident TDI are not reported. Sensitivity analysis showed that the pooled incidence rate was not significantly affected by the four studies45, 174, 176, 178 with relative weights higher than 10%.
The assessment of the pooled male-to-female TDI prevalence ratio was performed on 16 003 males and 16 006 females. The global prevalence ratio was 1.43 (95 CI, 1.34-1.52), suggesting that males were 34%-52% more likely to develop TDI than females (Table 6). The prevalence ratio estimates were similar among the WHO Regions, with the lowest ratio reported in the African Region (prevalence ratio, 1.31) and the highest in the South-East Asia Region (prevalence ratio, 1.53). Three studies53, 77, 80 yielded relative weights higher than 10%, but their effect on the pooled odds ratio was nonsignificant.
The meta-analyses performed using the pooled estimates assessed for the WHO Regions as units corroborated the reported results (Unpublished Material 9). Indeed, TDI prevalence to permanent teeth was 14.8%, TDI prevalence to primary teeth was 23.8%, and TDI prevalence among 12-year-old children was 14.3%, while male-to-female prevalence ratio was 1.41.
Regarding the uncertainty analysis, according to GBD the global number of incident bodily injuries that warranted healthcare assistance for the year 2013 was 972 200 000 (95% uncertainty interval, 950 600 000-1 008 300 000).28 According to the Västmanland study, 5% (95 CI, 4.73%-5.29%) of the injuries reported by the local public health facilities were TDIs, while 95% (95 CI, 94.71%-95.27%) were bodily injuries.2 Thus, there were 19 (95 CI, 17.90-20.14) bodily injuries for every TDI and, therefore, the estimated global number of incident TDI that warranted health assistance in the year 2013 was 51 168 000 (95% uncertainty interval, 47 200 000-56 330 000; data not in Table).
The estimated world population aged 0-19 years in 2013 was 2 498 762 000 individuals. Thus, using the pooled incidence rate assessed using only public health facility reports (Table 5), the global number of incident TDI that warranted healthcare assistance occurred before the age of 20 years was 62 719 000 (95 CI, 49 725 000-77 212 000) and the global number of all incident TDI occurred in 2013 was 69 688 000 (95 CI, 55 250 000-85 791 000; data not in Table).
Although the point estimate of the number of incident TDI gathered from the present meta-analysis was higher, the two estimates partly overlapped, thus suggesting that the present pooled incidence estimates yielded an uncertainty level similar to the level yielded by the GBD injury study. Indeed, the ratio between the two estimates was 0.98-1.82.
4 DISCUSSION
The main problems of disease frequency meta-analyses are not only related to the quality of primary studies, and to publication and selection biases, but also to the world representativeness of the study set and to the problem of merging data provided by different sources.19 The latter problem was automatically resolved because of the lack of disease registries, large population surveys, and the choice to exclude studies performed in emergency services and dental healthcare settings.
As for the quality of epidemiologic studies, the main forms of bias in disease frequency studies are selection and diagnostic bias. The TDI paradox is that the diagnosis of the majority of lesions is relatively easy, while their classification is complex, as there are more than fifty distinct diagnostic systems,10 and many injuries are seen in combination.180-182 Diagnostic bias is relatively low in TDI prevalence studies, due to regression toward the mean; namely, the proportion of false positives is counterbalanced by a similar proportion of false negatives,183 while it could be more serious in incidence studies. Indeed, reversals could occur at the follow-up examinations; that is, individuals diagnosed with TDI at baseline and without TDI at the follow-up examination. In caries incidence studies, diagnostic bias is adjusted using the net incidence (incident cases minus reversals) instead of the crude incidence.184 Such an adjustment was not considered in TDI incidence studies, and the pooled incidence rate reported in the present study likely over-estimated the true incidence rate.
At meta-analysis level, the degree of diagnostic bias was reduced excluding studies that did not use acknowledged TDI diagnostic systems and where examiners were not trained and/or calibrated. The choice to limit the diagnostic bias, thus getting more reliable data, was the reason why the pooled TDI frequency was not categorized for disease severity. Indeed, the assessment of disease severity required severity-based calibration of examiners and the use of the same TDI classification system. These requisites were not met by the included studies. Therefore, the global TDI frequency estimates categorized for severity would be unpredictable and unfeasible at the same time. Thus, although this choice prevented further analyses regarding, for example, social and individual costs of TDI at the global level, such a limit was compensated by the gain in terms of reliability of the pooled estimates.
As disease frequency epidemiologic studies must cope with the problem of sample representativeness, three items of the modified NOS, namely sample selection, sample size, and response rate, were dedicated to this issue. As for the sample size, all the studies excluding seven were large enough for the purpose of the present study, while low response rate was one of the exclusion criteria. The problem of sample selection procedures was acknowledged by only some studies that adopted random, cluster-random sampling selection procedures or were population-based studies (Unpublished Material 2-6). It is difficult to say what is the effect of this bias on each single study. At meta-analysis level, the choice to pool as many studies as possible could help overcome the limitation of including studies with non-representative samples18, 25.
At meta-analysis level, this study was designed to decrease selection bias, which refers to incomplete study retrieval, including more than 150 moderate-to-high quality studies and excluding low-quality studies. Therefore, even if some studies could be missing their effect on the pooled estimates must be minimal. The analysis of publication bias, however, suggested that there could be an excess of studies reporting high TDI prevalence to permanent teeth and incidence rate. Therefore, the present results could reasonably over-estimate the true disease prevalence and incidence rate.
The conservative approach adopted in this study to control the aforementioned limits resulted in wide confidence intervals of the pooled estimates, with consequent relatively high uncertainty. Nevertheless, the estimated global number of incident TDI that warrant assistance was not significantly different from the estimate resulting from the uncertainty analysis performed using the data from the GBD injury28 and the Västmanland2 studies, thus suggesting that the pooled estimates were reliable enough. However, this analysis also showed that there was a tendency to over-estimate the true world prevalence/incidence rate.
The pooled TDI incidence rate was probably less reliable than the pooled prevalences, for the abovementioned problems of diagnostic bias in incidence studies, the relatively low number of primary studies (Unpublished Material 5), and the heterogeneity between studies due to different data sources. Indeed, the incidence rate estimated using cohort studies was more than double the rate estimated using population-based studies, that is, 5.2 vs. 2.5 per 100 person-years (Table 5). This result was explained by the fact that all the individuals included in the cohorts were periodically examined, while in population studies, only data from individuals who seek dental healthcare are reported. Therefore, subjects with mild forms of TDI who do not seek dental healthcare and have low awareness toward TDI does not induce parents to seek care for their children.185 Further inconsistency is due to the TDI incidence not being the same throughout life, as it is roughly constant from birth to 10-12 years of age, declines constantly up to the age of 20 years, is close to nil up to the age of 40-45 years, and is approximately nil since that age. Overall, ninety percent of TDI occur before the age of 20.2 The problem of low reliability of incidence rates is acknowledged in disease frequency studies and even the GBD study group reported an increase in uncertainty when prevalence data were transformed into incidence rates.19
Accounting for the aforementioned limits and according to previously validated methodology,186 the reported results were used to estimate the global burden of TDI. As for TDI to permanent teeth, prevalence is rather stable starting from the age of 20 years until periodontal disease and/or dental caries result in the loss of injured teeth. At that point, reversals due to missing teeth occur and age-stratified prevalence rate decreases progressively. Using US population data on dental caries and periodontal disease provided by the National Institute of Dental and Craniofacial Research (NIDCR) during the National survey performed in 2011-2012 (see https://www.nidcr.nih.gov/DataStatistics/ByPopulation/Adults/, last accessed December 17, 2016), it was conjectured that TDI prevalence decreased appreciably after the age of 65 years. Thus, accounting for the chance that the pooled prevalence could be over-estimated, it was conservatively assumed that prevalence in individuals younger than 7 and older than 65 years was nil and that the pooled prevalence reported in Table 2 was valid only in individuals aged 7 to 65 years. The world population aged 7-65 years was 5 870 758 000 individuals in 2016. Therefore, there were approximately 900 million individuals who had had at least one TDI of any kind to permanent teeth (Table 7). The assessment of the burden of TDI to primary teeth refers to children aged between 1 and 6 years, a similar age range as that reported in Table 3. The world population aged 1-6 years was 791 115 600 children; thus, roughly 180 million children had had at least one TDI to primary teeth. Globally, overall, there are more than one billion subjects who have had TDI.
| Tooth type | Age | Individuals with TDI | 95% Confidence interval |
|---|---|---|---|
| Permanent teeth | 7-65 years | 892 355 216 | 763 198 540-1 021 511 892 |
| Primary teeth | 1-6 years | 179 583 241 | 136 862 999-227 050 177 |
| Any tooth | 1-65 years | 1 071 938 457 | 900 061 539-1 248 562 069 |
- Individuals older than 65 years and younger than 1 year are assumed to have no TDI.
This condition would rank fifth if it were included in the list of the main chronic diseases and injuries by the GBD study 2015, after caries, headache, anemia, hearing loss, and before migraine, with an uncertainty interval ranging between fourth and seventh.11 Considering TDI to permanent teeth and to primary teeth separately, the two conditions would rank sixth (95% uncertainty interval 5th-10th) and thirty-seventh (95% uncertainty interval, 33rd-44th), respectively. After dental caries, TDI is the second most frequent oral disease preceding periodontal disease and severe tooth loss.
These results demonstrate that TDI is very frequent worldwide and is still a neglected and unknown condition, probably because there are no universally acknowledged diagnostic, classification, and registration systems.187 This limited knowledge and awareness at public health level and among healthcare policymakers makes it difficult to allocate adequate resources, implement preventive programs, organize proper emergency services and first aid, and design acceptable awareness campaigns at the population level.188-190
CONFLICT OF INTEREST
The authors confirm that they have no conflict of interest.