Semi-circumferential endoscopic submucosal dissection for laterally spreading tumors on the ileo-ascending colon anastomosis
Abstract
Watch a video of this article
Brief Explanation
A 72-year-old woman with a past history of hysterectomy 30 years previously had received an ileo-ascending colon anastomosis graft for a subsequent ileus. The colonoscopy revealed two non-granular laterally spreading tumors (LSTs) on the anastomosis (Fig. 1a), both were classified as JNET type 2A (Fig. 1b). We performed endoscopic submucosal dissection (ESD) instead of endoscopic mucosal resection (EMR) because the lesions were located on the anastomosis (Video S1).1
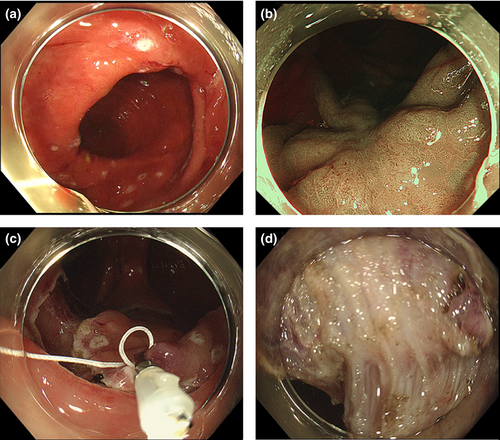
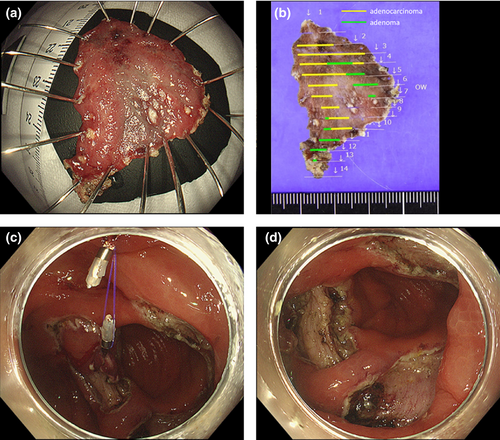
First, we performed marking using magnifying narrow band imaging (NBI) because some part of the margins were not clear with white light imaging. Then, we performed traction-assisted colonic ESD using a clip-and-line for the large LST.2-4 After injecting hyaluronic acid (ksmart, concentration of 4 mg/mL without dilution; Olympus Co, Tokyo, Japan), a mucosal incision was made per anum. A mucosal flap was created using a FlushKnife BT (DK2618JB15; Fujifilm Medical, Tokyo, Japan). We then grasped the mucosal flap with a clip-and-line; pulling the line with appropriate tension enabled better submucosal layer visibility (Fig. 1c). Severe fibrosis was observed immediately above the anastomosis (Fig. 1d). Despite the risk of injury or perforation, the lesion was resected en bloc in 89 min (Fig. 1d). Subsequently, ESD was performed for the small LST. Because the aforementioned traction-assisted methods require a scope reinsertion, we used a clip-and-ring for traction (Fig. 2a).5 Good visibility was obtained by traction, and the lesion was resected en bloc in 58 min (Fig. 2b). We closed ESD scars with clips. After cutting the ring using scissors forceps, the lesion was retrieved per anum using a retrieval net together with the first lesion. Pathologically, the LSTs were intramucosal adenocarcinoma with adenoma and tubular adenoma with negative margins, respectively. Clip-and-line method is useful because we can adjust tension by pulling and loosing line, while clip-and-ring method doesn’t demand reinsertion of scope.
Authors declare no conflicts of interest for this article.
Acknowledgment
We would like to thank Masanori Kitamura (Department of Diagnostic Pathology and Cytology, Osaka International Cancer Institute) for making histological figures, and Editage (www.editage.com) for English language editing.