Predicting depth of invasion for JNET Type 2B colorectal lesions: Is there a role for magnifying chromoendoscopy?
Given the underlying pathophysiology of colorectal cancer and adenoma to carcinoma sequence, efforts to improve modalities related to the detection and diagnosis of lesions prior to progression of disease, as well as proper assessment to estimate the depth of invasion, are crucial to improving patient outcomes. Recent advances and strategies aimed to improve the optical diagnosis of colorectal neoplasm have resulted in a paradigm shift in diagnosis of these lesions. However, challenges remain in endoscopists’ ability to accurately predict histologic features based upon virtual chromoendoscopy alone.
At present, magnifying narrow banding imaging (NBI) during colonoscopy to assess colonic lesions using the Japan NBI Expert Team (JNET) classification has been established as a reliable and sensible method to predict depth of invasion and guide treatment. This JNET classification1 is based upon vessel and surface pattern findings and was designed and validated2 to overcome the limitations of the NBI International Colorectal Endoscopy (NICE) classification system.3 The JNET classification includes Type 1, 2A, 2B, and 3 which correlate with the pathological diagnoses of hyperplastic polyp or sessile serrated polyp, low-grade intramucosal neoplasms, high-grade intramucosal neoplasms or superficial submucosal cancer (T1a; <1000 μm), and deep submucosal invasive cancer (T1b; ≥1000 μm), respectively.1, 2 This ability of the JNET classification to differentiate or subdivide Type 2 lesions into Type 2A and 2B has shown an improved ability to predict superficial from deep invasion and determine patient candidacy for appropriate en bloc endoscopic resection – thus avoiding unnecessary colorectal surgery for lesions with low risk of lymph node metastasis.4
However, despite this stratification of Type 2 lesions, JNET Type 2B lesions include a wide variety of colorectal neoplasms ranging from low-grade dysplasia to deep submucosal lesions – making therapeutic decisions challenging. In fact, in the JNET validation study by Iwatate and colleagues, over half of the colorectal lesions classified as Type 2B were determined histologically to have deep submucosal invasion.2 However, given concerns regarding depth of invasion for Type 2B lesions, alternative strategies to classify these lesions have been devised in effort to better predict the depth of invasion. One strategy, proposed by Sumimoto and colleagues, aimed to determine if the polyp morphology was a predictor of JNET Type 2B lesion accuracy.5 This study examined non-polypoid versus polypoid lesions, using the Paris classification (polypoid: pedunculated, Ip and sessile, Is; and nonpolypoid: slightly elevated, IIa, flat, IIb and slightly depressed, IIc) though found no difference based upon morphology.
The most updated European Society of Gastrointestinal Endoscopy guidelines from 2019 on advanced imaging for detection and differentiation of colorectal neoplasia suggest that direct observation of the Kudo pit pattern with crystal violet should be performed for JNET 2B lesions.6 With magnifying dye-based chromoendoscopy, Kudo has proposed a gross classification of pit patterns stratified into seven distinct types: non-neoplastic patterns identified as type I (roundish pits) or type II (stellar or papillary pits); non-invasive patterns as type IIIS (small roundish pits), IIIL (roundish and tubular pits), IV (branch-like or gyrus-like pits), or superficial VI (irregular and distorted pits); or invasive patterns which include type VN (non-structural and absence of pits) and deep VI (highly irregular and distorted). Multiple studies have validated the Kudo pit pattern classification for colorectal lesions by magnifying chromoendoscopy in comparison with the histological findings.7
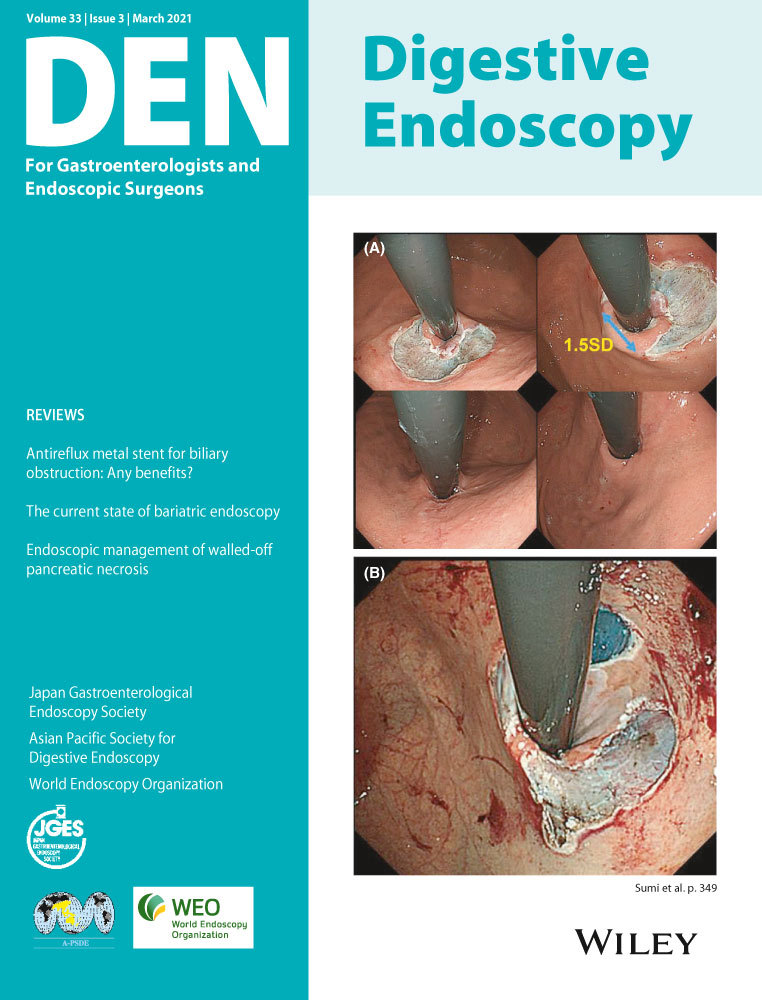
In this issue of Digestive Endoscopy, Hosotani and colleagues retrospectively analyzed the efficacy of magnifying chromoendoscopy to further evaluate JNET type 2B colorectal lesions. In this large, single-center study including 1229 patients and 1573 colorectal lesions (all ≥ 10 mm), 69.7% of lesions were classified on magnifying NBI as JNET Type 2A, 22.8% as Type 2B, and 7.5% as Type 3. Using magnifying NBI, the risk of deep invasion for Type 2A and Type 3 lesions was shown to be 1.8% and 96.6%, while for Type 2B lesions, the risk of invasive malignancy was sub-optimal at 30.1%. However, when magnifying chromoendoscopy was performed in combination with magnifying NBI to better stratify Type 2B lesions, the associated pit pattern significantly improved this ability to predict the depth of invasion. Among Type 2B lesions, non-V pit pattern was associated with an invasive risk of 4.3%, VI-low grade pit pattern invasive risk of 6.6%, and VI-high grade pit pattern invasive risk of 76.0%. The authors further performed multivariable logistic regression analyses which further demonstrated a V pit pattern, along with protruded morphology and increased lesion size, were a significant predictor associated with deeply invasive cancer.
The results of this study provide much needed literature to support the current ESGE guideline recommending assessment of the pit pattern for Type 2B lesions. Based upon these results, the addition of magnifying dye-based chromoendoscopy for JNET Type 2B colorectal lesions may better predict risk of deep invasion and stratify which lesions are amenable for endoscopic resection. Although this manuscript was retrospective in nature, this study included over 350 Type 2B lesions and showed the combination of two modalities (magnifying NBI and magnifying chromoendoscopy) did significantly improve diagnostic accuracy for T1 colorectal cancer. These data validate preconceived diagnostic strategies and may serve as an ideal algorithm for the optical diagnosis of JNET Type 2B lesions. This combination method to perform “optical biopsy” may be critical in avoiding ill-advised endoscopic resection (i.e., either endoscopic mucosal resection [EMR] or endoscopic submucosal dissection8) for invasive cancers or unnecessary surgery for low-risk lesions.
This notion of reducing unnecessary procedures and surgeries is pivotal as the number of surgeries for benign colorectal polyps has significantly increased in the United States and in several other countries with associated high morbidity and mortality over the last two decades.9, 10 Despite this, broad adoption of optical magnification continues to be an issue for Western countries given the fact that the magnifying colonoscope is not widely utilized in clinical practice and crystal violet is not commercial available in the United States. Additionally, it should be noted that despite magnifying chromoendoscopy having a good predictive value for guiding management of colorectal lesions, adoption of routine use, even for use specifically with JNET Type 2B lesions, may be challenging given the fact that dye-based chromoendoscopy is time-consuming, requires the use of staining solutions and spraying catheters, and may be limited by mucus on the lesion surface. Also, familiarity with newer devices and techniques is important given the learning curve or clinical expertise needed to perform an effective procedure. In an effort to increase adoption of virtual and dye-based chromoendoscopy in Western countries, online training systems for optical biopsy or use of artificial intelligence (AI) may be necessary.
In summary, estimation of the depth of invasion for colorectal neoplasms is an incredibly important step to determine appropriate management. While magnifying NBI endoscopy to determine JNET classification is the most useful and practical method for histologic prediction and assessing invasion depth, magnifying chromoendoscopy for JNET type 2B lesions is still necessary to reach a satisfactory diagnostic accuracy. Despite this study demonstrating presence of a V pit pattern to greatly enhance ability to determine deep invasion, additional studies are needed to further elucidate how much diagnostic accuracy can be improved by additional magnifying chromoendoscopy.
Conflict of Interest
Thomas R. McCarty has no conflicts to disclose. Hiroyuki Aihara is a consultant for Olympus America, Boston Scientific, Fujifilm Medical Systems, Medtronic, ConMed, Auris Health, Lumendi, and 3-D Matrix.
Funding Information
None.