Case Report—Cytopathological Diagnosis of Metastatic Squamous Cell Carcinoma in Vitreous Fluid
Funding: The authors received no specific funding for this work.
Abstract
This report describes a rare case of HPV-associated oropharyngeal squamous cell carcinoma metastasising to the vitreous fluid, presenting initially with nonspecific visual symptoms. It emphasises the critical importance of maintaining a high clinical suspicion and utilising cytological diagnosis to improve patient management and outcomes.
1 Introduction
Squamous cell carcinoma (SqCC) in the vitreous fluid is exceedingly rare and usually caused by metastasis from primary sites such as lung, breast, and cervix [1-3]. Metastases to the vitreous from other primary sites are even rarer; when they do occur, they are most commonly from cutaneous melanoma in patients previously treated with immune checkpoint inhibitors [4]. Most patients present with vision changes at advanced stages of malignancy with non-specific ocular symptoms, making diagnosis challenging [2]. Given the scarcity of literature on this entity, there are no consensus therapy guidelines for these patients. Reporting individual cases is crucial for expanding the knowledge base, guiding clinical suspicion, and improving management strategies, especially because timely and accurate diagnosis could potentially impact the quality of life of affected patients. Herein, we present a case of oropharyngeal SqCC with metastasis to the vitreous humour.
2 Case Presentation
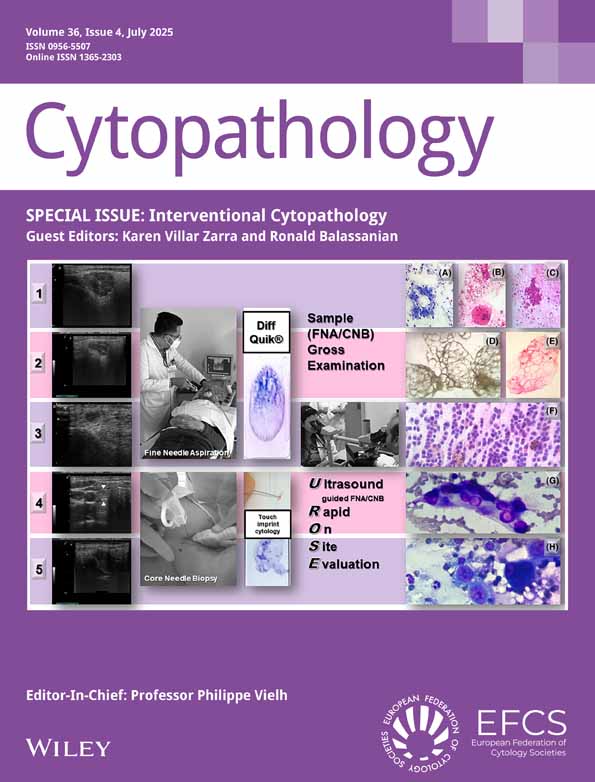
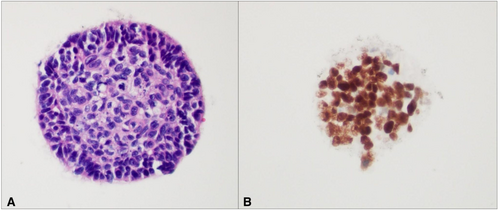
Our patient is a 57-year-old male with HPV-associated squamous cell carcinoma of the oropharynx initially diagnosed in 2015. He had multiple local recurrences and metastases to the bone, retroperitoneum, and lung throughout the course of chemoradiotherapy. While on therapy with capecitabine, he developed a sudden decrease in vision and floaters in the left eye and was referred for ophthalmic evaluation. The examination was significant for intraretinal lesions, raising suspicion for panuveitis and posterior cyclitis. A pars plana vitrectomy was performed and sent for cytologic examination wherein the cell block showed a cluster of cells with nuclear enlargement, nuclear membrane irregularities, coarse chromatin, prominent nucleoli, and atypical mitoses (Figure 1A). These cells were strongly and diffusely positive for pancytokeratin and p40 immunohistochemistry (IHC, Figure 1B), raising the suspicion for involvement by the patient's known squamous cell carcinoma. Since ocular adverse effects are common in patients taking anti-metabolite chemotherapeutic drugs such as capecitabine, as was the case in this patient, the clinical suspicion for metastatic disease was low [5]. Consequently, a membrane peel was obtained for corroboration of the cytologic findings. Surgical pathology examination of the epiretinal membrane confirmed the diagnosis of non-keratinising squamous cell carcinoma (Figure 2A) which stained strongly and diffusely with pancytokeratin (Figure 2B) and p16, serving as a surrogate marker for HPV (Figure 2C). The patient was counselled, and he elected to receive intravitreal Melphalan instead of local radiotherapy due to the marginally worse adverse effect profile of radiotherapy.
3 Discussion
Non lymphatic distant metastases to the orbital soft tissue and vitreous humour have been documented to arise predominantly from breast and lung primaries, followed by a few articles reporting cervical SqCC as the primary tumor [1-3], occasional case reports of melanoma and even fewer involving cancer patients treated with immune checkpoint inhibitors4. Notably, case reports of SqCC spreading to the vitreous in a non-contiguous manner are few and far between [2, 6-8]. The challenges associated with diagnosing ocular metastasis are compounded by their nonspecific and vague presentation. Most patients with metastatic involvement of the vitreous present with vision changes and sudden onset of floaters usually at advanced stages of malignancy with poor prognosis and adverse clinical outlook2. Previous reports mentioned an average survival of 7 months following the diagnosis of ocular metastases in patients with head and neck carcinoma [2, 7, 8]. A similar dismal prognosis has also been demonstrated with other primaries including renal cell carcinoma, where ocular metastasis may serve as the initial sign of systemic dissemination of disease [9]. A recent analysis highlighted the importance of comprehensive evaluation when ocular symptoms are present in patients with an established malignancy, emphasising the importance of addressing both the local and systemic disease burden [4].
Due to the rarity of these cases, the true incidence of such distant non-lymphatic metastases remains unclear. Consequently, ophthalmologists often maintain a low index of suspicion for this diagnosis when evaluating SqCC patients with vision changes. The only method of establishing a definite diagnosis is vitreous fluid sampling, which is an invasive procedure that many patients with advanced cancer may not consent to, leading to missed diagnoses in a large proportion of cases. The subsequent dearth of documented cases prevents the formulation of consensus therapy guidelines or establishment of clinical trials. A prior study conducted postmortem examination on patients with breast cancer and found that more than one third of cases had ocular metastasis, which was significantly higher than previously reported [10].
This case highlights that a high index of suspicion should be maintained with ocular cytologic specimens in patients with a history of squamous cell carcinoma. Current literature highlights that timely diagnosis is essential in determining appropriate interventions. Current gaps in the literature include the estimated prognosis following metastasis in the ocular region and analysis of whether initiating radiation/chemotherapeutic interventions increase survival in these types of cases. Further expansion of these studies could include quality of life metrics to inform decision making with regards to risk benefit ratios in the treatment of vitreous metastasis. However, the rarity of these cases hampers the formulation of consensus therapy guidelines. Our case is not only unusual, but is one of the first reports of SqCC of the oropharynx metastasizing to vitreous fluid. Our patient demonstrated significantly worse survival following diagnosis of ocular metastasis compared to the average of 7 months previously reported [2]. The true extent of survival, possible interventions, and improved quality of life measures with poor prognosis all remain to be elucidated with these types of cases. Our case highlights the importance of early diagnosis as patients are typically at later stages of cancer by this point and could benefit from improved therapeutic management to increase quality of life.
Author Contributions
Poorva Singh: contributed to the conception of the case report, clinical case selection, and primary drafting of the manuscript. Katlin T. Wilson: conducted literature review, contributed to manuscript writing and revisions, and assisted in formatting and figure preparation. Linda Varghese: provided cytopathologic interpretation, supervised manuscript development, and critically revised the manuscript for intellectual content. Jimmie Stewart: provided cytopathologic interpretation, contributed to case interpretation, and offered critical review and approval of the final manuscript. All authors meet the ICMJE criteria for authorship, have reviewed and approved the final version of the manuscript, and agree to be accountable for its contents.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.