Semi-quantitative HPV viral load in patients with ASC-US cytology: viral load correlates strongly with the presence of CIN but only weakly with its severity
Abstract
Objectives
This study was performed to evaluate the prognostic significance of human papillomavirus (HPV) viral load, expressed in relative light units (RLUs), in patients with atypical squamous cells of undetermined significance (ASC-US) cytology.
Methods
A total of 349 ASC-US cases with HPV infection, detected using Hybrid Capture 2, were diagnosed histologically. A colposcopically directed punch biopsy was performed on acetowhite areas. Endocervical curettage biopsy and random cervical punch biopsy in four quadrants were performed in unsatisfactory colposcopy cases. In negative colposcopy cases, random cervical punch biopsy in four quadrants was performed.
Results
Case with no cervical intraepithelial neoplasia (CIN), CIN1 and CIN2+ (CIN2/CIN3) accounted for 162, 135 and 52 cases, respectively. The mean age showed no difference among the three groups (P = 0.510). There was a significant correlation between RLU values and the presence of CIN (P < 0.001), but less so with its severity: the median RLU values for negative, CIN1 and CIN2+ cases were 42.68, 146.45 and 156.43, respectively, with widely overlapping confidence intervals. The cut-off values of RLU to detect CIN1+ and CIN2+ were 6.73 and 45.64, respectively.
Conclusions
The HPV viral load in ASC-US cases showed a significant correlation with the presence of CIN and less so with its severity, and showed large overlap of viral loads between grades of CIN. In ASC-US cases, RLU was not an accurate predictor of immediate high-grade CIN.
Introduction
Approximately 5% of Papanicolaou (Pap) tests performed each year in the USA are interpreted as atypical squamous cells of undetermined significance (ASC-US), which is the most common abnormal cytological result within cervical cancer screening.1, 2 Although repeat cytological testing, colposcopy or DNA testing for high-risk (HR) types of human papillomavirus (HPV) are all acceptable methods for the management of women with ASC-US in the USA,3 the American Society for Colposcopy and Cervical Pathology (ASCCP) recommends HPV DNA-based triage as the most effective strategy for the management of women with ASC-US cytology.4 HPV DNA-based triage is recommended for the management of women with borderline and low-grade cytology in the NHS Cervical Screening Programme in England: http://www.cancerscreening.nhs.uk/cervical/hpv-triage-test-of-cure.html
The sensitivity of cytology for the prediction of cervical intraepithelial neoplasia (CIN) grade 2/CIN3 varies between 40 and 80%, with a specificity of 83–92%.5-7 Meanwhile, HPV DNA testing for the detection of CIN2/CIN3 in the triage of ASC-US cytology is reported to have low specificity (63%) and a low positive predictive value (PPV), despite the high sensitivity (83–100%).2 Thus, HPV DNA testing causes high referral rates to second-level colposcopy and biopsy. To improve the test specificity, several studies have implemented a higher cut-off for the positivity of HPV DNA testing.8 However, these trials caused a decrease in sensitivity and negative predictive value (NPV), and no cut-off level could exclude patients with underlying CIN2/CIN3 lesions or cancer.9
The Hybrid Capture 2 (HC2®; Digene Co., Silver Spring, MD, USA) assay, a Food and Drug Administration (FDA)-approved, commercially available test, is currently one of the most frequently applied methods of detection of HR-HPV. The test detects the presence of any of 13 HR-HPV types and provides a quantification of the viral DNA load. Positive specimens are those with relative light units (RLUs) equal to or greater than the mean RLU values of positive controls containing 1.0 pg/ml viral DNA. High viral load levels and the severity of high-grade CIN have been shown to be closely correlated.5, 9, 10, 8 However, the use of viral load as a predictor of high-grade cervical lesions in women with ASC-US cytology is doubtful, because of the large overlap of diagnosis.2, 5, 11
Our institute manages women over the age of 21 years with ASC-US by HPV DNA testing, repeat cervical cytology testing or immediate colposcopy, as recommended.4 All HPV DNA-positive cases are diagnosed histologically by colposcopically directed punch biopsy and/or endocervical curettage (ECC). Even for negative colposcopy cases, random cervical punch biopsy in four quadrants is conducted routinely. This study was performed to determine the correlation between the semi-quantitative measurement of HPV viral load, expressed in RLUs, and the grade of cervical pre-neoplastic lesions in ASC-US cases. We further evaluated the usefulness of RLU cut-offs by comparison with histologically proven cases.
Materials and methods
Study population
Our hospital has been a referral centre for patients with cancer since August 2005. All patients who were diagnosed as having ASC-US12 at Konkuk University Hospital, Seoul, South Korea, from August 2005 to December 2012, were managed by repeat cervical cytology testing, immediate colposcopy or HPV DNA testing, according to consensus guidelines.1
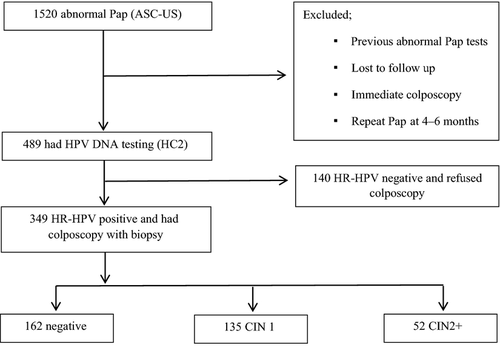
Patients were excluded from the analysis if any of the following criteria were present: (1) previous abnormal Pap tests; (2) loss to follow-up; (3) immediate colposcopy; or (4) repeat Pap tests at 4–6 months. Among the 1520 women diagnosed as having ASC-US in cervical cancer screening, 489 underwent HPV DNA testing using the HC2 assay following the manufacturer's instructions (Figure 1). In total, 349 HR-HPV DNA-positive cases underwent colposcopy. A colposcopically directed punch biopsy was performed on acetowhite areas. ECC biopsy and random cervical punch biopsy in four quadrants were performed in unsatisfactory colposcopy cases. In negative colposcopy cases, random cervical punch biopsy in four quadrants was performed. We examined all 349 cases histologically and analysed all clinical and histological data from the patients. Two experienced gynaecological pathologists reviewed all of the histological data of the cases. Discrepancies between their results were settled through discussion. The data were analysed on the basis of a two-tiered system with low-grade lesions that are likely to be self-limited (CIN1) and high-grade lesions that have the potential to progress to invasive carcinoma (CIN2/CIN3).13 This study was approved by the institutional review board at Konkuk University Hospital.
Semi-quantitative HPV viral load
The HC2 assay uses chemiluminescence to detect the presence of HPV, which is measured in RLUs, and includes a probe designed to detect 13 types of HR-HPV (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68).14 Test results were scored as positive when the RLU/cut-off (RLU/CO) ratio (RLUs of the specimen/mean RLUs of two positive controls) was 1 pg/ml or greater.14 The sensitivity of the test was 1 pg of viral DNA/100 μl.14 At our hospital, exact RLU values are routinely reported for reference, although the test is used in a qualitative fashion (positive versus negative).2 RLU/CO values of one or higher are defined as positive. However, 0.80 ≤ RLU/CO ≤ 1.90 is described as an equivocal range because of the possible non-specific responses.
Statistical analysis
The correlation between pathological diagnosis and RLU/CO was evaluated statistically with a Kruskal–Wallis one-way analysis of variance using IBM® SPSS® statistics 20.0 (IBM SPSS Statistics, Chicago, IL, USA); P values of less than 0.05 were considered to be significant. The receiver operating characteristic (ROC) curves and cut-offs for positive final diagnoses were calculated with MedCalc version 9.3.9.0 (MedCalc Software, Ostend, Belgium). The sensitivity and specificity of the cut-offs were determined.
Results
The mean age of the studied patients was 40.4 ± 12.3 years. Of the 349 patients, 162 (46.4%) had no CIN lesion (negative), 135 (38.7%) were diagnosed as CIN1 and 52 (14.9%) as CIN2 or CIN3 (CIN2+) (Figure 1). The ages of patients, intervals between HC2 test and biopsy and RLU values in the three groups are shown in Table 1. There was no significant difference in age groups (p = 0.510).
| Characteristic | Negative | CIN1 | CIN2+ | P value |
|---|---|---|---|---|
| Number of patients | 162 | 135 | 52 | |
| Age (years) | 41.4 ± 12.9 | 40.1 ± 12.1 | 39.5 ± 11.5 | 0.510 |
| Interval between HC2 test and biopsy (days) | 8.0 (1.0–113.0) | |||
| RLU value | 42.68 (0.84–2368.30) | 146.45 (0.92–2701.47) | 156.43 (2.20–1563.62) | <0.001 |
- CIN, cervical intraepithelial neoplasia; HC2, Hybrid Capture 2 test; RLU, relative light unit.
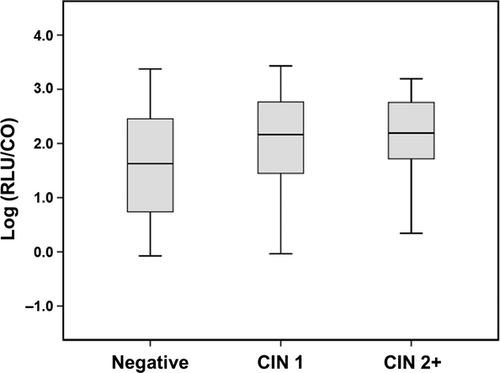
Increasing RLU values showed a statistically significant correlation with worsening outcomes (P < 0.001) (Table 1, Figure 2).
To assess viral load as a predictor of histological outcome, we determined the cut-off points for the RLU values. A cut-off point of 6.73 predicts CIN1+ (Figure 3a). At this point, we estimated a sensitivity of 95.4%, specificity of 29.3% and a PPV of 59.8%. To improve the specificity to 90.5%, the cut-off was adjusted to 981.21. However, the sensitivity decreased markedly to 18.5% (Table 2). At an RLU value of 2368.30, the specificity was 100%.
| RLU | Sensitivity | Specificity | PLR | NLR | PPV | NPV | |
|---|---|---|---|---|---|---|---|
| No CIN lesion versus CIN1+ | 6.73 (cut-off) | 95.4 | 29.3 | 1.35 | 0.16 | 59.8 | 85.2 |
| 981.21 | 18.5 | 90.5 | 1.94 | 0.90 | 68.1 | 50.2 | |
| 2368.30 | 2.3 | 100.0 | 3.63 | 0.98 | 100.0 | 48.2 | |
| ≤CIN1 versus CIN2+ | 45.64 (cut-off) | 80.0 | 43.5 | 1.42 | 0.46 | 18.3 | 93.2 |
| 10.76 | 91.1 | 21.8 | 1.16 | 0.41 | 15.5 | 93.9 | |
| 1333.13 | 6.7 | 91.6 | 0.79 | 1.02 | 11.1 | 86.1 |
- CIN, cervical intraepithelial neoplasia; NLR, negative likelihood ratio; NPV, negative predictive value; PLR, positive likelihood ratio; PPV, positive predictive value; RLU, relative light unit; ROC, receiver operating characteristic.
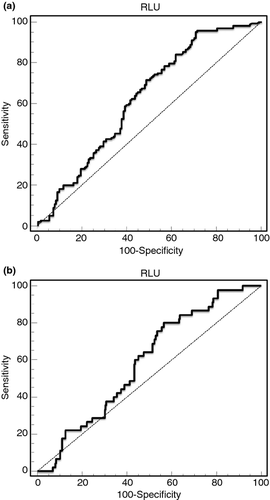
A cut-off value of 45.64 predicted CIN2+ (Figure 3b). However, the sensitivity and specificity were relatively low (80.0% and 43.5%, respectively). At this point, the NPV was 93.2 (Table 2). Reducing the cut-off to 10.76 improved the sensitivity to 91.1%, but the specificity worsened to 21.8%. To achieve a specificity of 91.6%, we adjusted the cut-off to 1333.13 (sensitivity 6.7%).
Nevertheless, of the 60 cases with RLU values of less than 6.73, seven (11.7%) had CIN1+. Of the 48 cases with RLU values higher than 981.21 (specificity of 90.5%), 16 (33.3%) showed no CIN. In total, 17 of 52 CIN2+ cases (32.7%) had RLU values of less than 45.64. RLU values higher than 1333.13 (specificity of 91.6%) were detected as CIN2+ in three (10.7%) of 28 cases.
Discussion
The viral load detected by the HC2 assay has been reported to be associated with CIN2/CIN3 frequency in several earlier studies.2, 15-18 Similar to previous studies on HPV viral load in cases of ASC-US cytology,2, 11 our study indicates that an increasing HPV viral load in ASC-US cases correlates with the severity of the cervical lesions, although the difference was greater between no CIN and CIN1+ than between CIN1 and CIN2+. This study was performed in patients diagnosed as having ASC-US at one institute. All of the patients positive for HPV DNA underwent histological diagnosis based on acetowhite lesions and/or ECC or random biopsies. The values of the cumulative prevalence of CIN1 and CIN2+ diagnosed as ASC-US at our institute during the study period were 27.6% and 10.6%, respectively (data not shown). This value is similar to the real prevalence of pre-cancerous lesions with borderline cervical cytology detected in a screening setting.1 However, the prevalence increased to 38.7% and 14.9%, respectively, in the HPV DNA-positive testing group in the present study.
In the current study, we wanted to determine the cut-off points of RLU values for predicting CIN1+ (6.73) and CIN2+ (45.64). As expected, the cut-off values for the detection of CIN1+ and CIN2+ showed low specificity (29.3% and 43.5%, respectively) and a low PPV (59.8% and 18.3%, respectively), despite the high sensitivity (95.4% and 80.0%, respectively). Our study demonstrated a marked association between viral load and the underlying CIN, especially in CIN2+ cases. Several earlier studies have shown a strong relationship between viral load determined semi-quantitatively and high-grade CIN.2, 5, 19, 20 Nevertheless, as a predictive method for CIN, viral load expressed in RLUs is not reliable in ASC-US cases, because our current study showed large overlap of viral loads between the grades of cervical lesions. Origoni et al.2 subclassified the HC2 results into five classes of increasing RLU/CO values to determine the correlation with the probability of CIN2/CIN3 in ASC-US cases. Although this study showed a significant correlation with increasing CIN2/CIN3 prevalence, two (4%) of 52 CIN2/CIN3 cases had a very low RLU/CO value of class 1 (0 < RLU/CO ≤ 1). Therefore, ‘significant correlation’ did not mean that the RLU/CO classes were definite diagnoses, but that the PPV of HPV DNA positivity increased consistently with increasing RLU/CO values. However, Bae et al.14 showed a difference in the negative conversion rate between groups with high and low RLU/CO values. Thus, the researchers demonstrated that RLU/CO may be used to select women at higher risk of the discovery or development of CIN, and could therefore be used as a follow-up test in women with negative cytology but who are positive for HR-HPV DNA.14
Castle et al.21 reported that a positive HR-HPV test (with negative cytology or ASC-US+) at one time point predicts cervical cancer risk for more than 15 years, identifying not only women who have prevalent CIN3+, but also women whose HPV infections will persist and develop into disease in the future. In contrast, cytological abnormalities are a specific diagnostic marker for immediate, microscopic and visible disease, but do not forecast clinically important disease beyond 1 or 2 years; thus, it is necessary to repeat cytological testing at much shorter intervals.21, 22 We believe that, in ASC-US cases, as in cases detected by a screening test, HPV infections may persist and develop into cervical lesions in the future. In this study, we have not recommended HPV DNA testing as a screening tool, but rather as the most effective strategy for the management of women with ASC-US cytology. That is, HPV-infected ASC-US cases were histologically assessed to detect immediate microscopic disease. Abnormal histology cases with a low RLU/CO were included in the present analyses. The RLU/CO of these cases might decrease after the development of cervical lesions. ‘Negative’ histology cases with high RLU/CO values were excluded from the calculation of cut-offs. However, according to previous studies, these patients could develop cervical diseases in the future. This concept could explain the large overlap of viral loads between the grades of CIN, despite the statistically significant correlation between RLU values and cervical lesions in the present study (Figure 2). We have decided to extend our study to a longer term follow-up to determine more accurate values for cut-offs. We expect that the inclusion of newly diagnosed cervical lesion cases during the study period may also help to determine more accurate cut-offs.
Given the limitations of both cytology and HPV DNA-based approaches as stand-alone tests, new disease-specific biomarkers of HPV-associated transformation have been developed and validated.23 In a result from the ATHENA HPV study, co-testing with genotyping triage and an ASC-US threshold detected the most CIN2+ and CIN3+, with the highest sensitivity (67.5% and 76.2%, respectively) and the highest false-positive rate for CIN3+ (18.5%).24 The ASCCP recommends genotyping assays for the presence of HPV 16/18 for women aged 30 years and older who are HR-HPV DNA positive with normal cytology.25, 26
Several biomarkers (i.e. p16, Ki-67, mRNA, methylation of tumour suppressor genes) have been evaluated for cytology triage, although none has yet been incorporated into screening algorithms.26 Darragh et al. 13 concluded that only p16 immunohistochemical staining could be recommended for differential diagnosis between pre-cancer (CIN2 or CIN3) and its mimics (e.g. immature squamous metaplasia, atrophy, reparative epithelial changes, tangential cutting). In a recent meta-analysis of eight studies, the pooled sensitivity and specificity of APTIMA-mRNA, which identifies mRNA of 14 HR-HPV types to triage ASC-US to detect underlying CIN3+, were 96.2% and 54.9%, respectively.27 Schmidt et al.28 reported that p16/Ki-67 dual-stain cytology as a triage for the detection of CIN2+ lesions had sensitivities of 92.2% (ASC-US) and 94.2% (low-grade squamous intraepithelial lesion, LSIL) and specificities of 80.6% (ASC-US) and 68.0% (LSIL). Several studies have reported that the detection of HPV viral methylation may distinguish women with CIN2+ from those with HR-HPV infections that do not show evidence of CIN2+.29 A positive association between methylation of CpG sites in the L1 gene and CIN2+ has been reported.29 However, candidate HPV viral methylation needs to be thoroughly validated for clinical use.
This study contained several limitations. First, the study was performed retrospectively with a relatively small number of patients at a single institution. Second, although we managed the cases with ASC-US according to the guidelines, we did not have accurate criteria to select patients for HPV DNA testing, repeat cervical cytological testing or colposcopy. In general, we prefer HPV DNA testing because of its higher sensitivity compared with other methods. For postmenopausal women, we recommend a repeat Pap smear more frequently. This protocol might have caused selection bias in the current study. Third, we did not distinguish between CIN2 and CIN3 because of the relatively small number of patients in these groups and the frequency of both lesions being present. Lastly, we could not analyse HPV 16 and HPV 18 risk stratification separately because we do not routinely recommend HPV 16 and HPV 18 detection in HPV DNA-positive cases.
In summary, the HPV viral load in ASC-US cases showed a significant correlation with the severity of cervical lesions. Although the cut-offs of RLUs of 6.73 for the detection of CIN1+ and 45.64 for the detection of CIN2+ may have prognostic value, this study showed large overlap of viral loads between the grades of CIN. In ASC-US cases, RLUs were not an accurate predictor of immediate cervical lesions, possibly because HPV infections with a high RLU/CO could persist and develop cervical lesions in the future. To achieve more accurate cut-offs, a longer term follow-up, including newly detected cervical disease cases, is needed.
Acknowledgments
This work was supported by Konkuk University Medical Center Research Grant 2011.