FOXA1 expression affects the proliferation activity of luminal breast cancer stem cell populations
Funding Information:
Ministry of Education, Culture, Sports, Science and Technology of Japan.
Abstract
The expression of estrogen receptor is the key in most breast cancers (BC) and binding of estrogen receptor to the genome correlates to Forkhead protein (FOXA1) expression. We herein assessed the correlation between the cancer stem cell (CSC) population and FOXA1 expression in luminal BC. We established luminal BC cells derived from metastatic pleural effusion and analyzed the potency of CSC and related factors with established luminal BC cell lines. We also confirmed that mammosphere cultures have an increased aldehyde dehydrogenase-positive population, which is one of the CSC markers, compared with adherent culture cells. Using a quantitative PCR analysis, we found that mammosphere forming cells showed a higher expression of FOXA1 and stemness-related genes compared with adherent culture cells. Furthermore, the growth activity and colony-forming activity of 4-hydroxytamoxifen-treated BC cells were inhibited in a mammosphere assay. Interestingly, 4-hydroxytamoxifen-resistant cells had significantly increased FOXA1 gene expression levels. Finally, we established short hairpin RNA of FOXA1 (shFOXA1) MCF-7 cells and investigated the relationship between self-renewal potential and FOXA1 expression. As a result, we found no significant difference in the number of mammospheres but decreased colony formation in shFOXA1 MCF-7 cells compared with control. These results suggest that the expression of FOXA1 appears to be involved in the proliferation of immature BC cells rather than the induction of stemness-related genes and self-renewal potency of CSCs.
Breast cancer (BC) treatment has progressed in recent decades. Many previous clinical studies clarified that pathological characteristics, such as estrogen receptor (ER), progesterone receptor (PgR), human epidermal growth factor receptor 2 (HER2), and Ki-67 expression, correlate with the gene expression profile, such as PAM50,1, 2 prognosis, and treatment effects. Therefore, we can clinically divide BC into five types according to these pathological characteristics in consideration of the therapeutic plan: luminal A, luminal B, luminal-HER2, HER2-enrich, and triple negative type.3 For luminal A and B, which are categorized as ER-positive BC, endocrine therapy can be used with chemotherapy treatment.
It is known that ER-positive BC constitute approximately 70% of all BC, and it shows a good prognosis.4-6 However, it has been reported that ER-positive and HER2-negative BC patients with low Ki-67 proliferation, so-called luminal A type, can lead to late recurrence compared to other BC subtypes, possibly due to the presence of dormant tumor cells.7 The BC markers of late recurrence8-10 or commercialized prognostic prediction systems such as Oncotype DX11 and MammaPrint12 have been established. However, the BC cell mechanism of late recurrence is still poorly understood.
Cancer stem cells (CSCs) have been isolated and characterized to have high potential for tumor growth, self-renewal, multidifferentiation, high metastatic ability, and drug resistance.13-18 Interestingly, there are many similar biological characteristics between dormant cells and CSCs, especially in terms of therapy resistance and cell signals that regulate self-renewal and the quiescent state of CSCs.19-21 Therefore, it is speculated that CSCs might contribute to late recurrence with dormant cells,22 and we hypothesized that some part of CSCs would be involved in the late recurrence of luminal type A in this study.
Al-Hajj et al.13 reported that the CD44+/CD24−/low population of BC cells showed higher tumor initiating potential than other populations. In addition, Ginestier et al.23 reported that aldehyde dehydrogenase (ALDH) 1 is a good marker for both stem cells of normal mammary cells and BC cells. Moreover, it has been reported that the expression of these CSC markers correlate with a clinically poor outcome.23-26 These markers were positively expressed in triple negative BC cells as well as in normal mammary stem/progenitor cells. Additionally, most of the previous reports showed that they were ER-negative.27 Regarding CSCs of the luminal type of BC, Sun et al.28 reported that estrogen promotes stemness and invasiveness through Gli1 activation, however, the mechanisms that maintain CSCs in luminal BC remains obscure.
Forkhead protein (FOXA1) is the downstream target of GATA binding protein 3 and maintains ER sensitivity.29 FOXA1 directly binds to the estrogen receptor 1 promoter and activates ER mRNA expression.30 Moreover, it is known that FOXA1 binds to chromatin DNA and modulates ER activity.31, 32 Conversely, it has been reported that FOXA1 activates p27 transcription and works as a growth repressor.33 Until now, the correlation between FOXA1 and CSCs through ER has not yet been determined. According to tissue samples, Horimoto et al.34 clarified that those metastatic breast cancer patients whose tissue highly expressed FOXA1 took a long time to relapse compared to low FOXA1 patients, indicating that FOXA1 might be related to late recurrence. Taken together, the tendency for luminal A type BC and FOXA1-enriched BC to cause late recurrence, and the similarity between CSCs and dormant cells, it may be hypothesized that FOXA1 expression, especially in CSCs, causes late recurrence and provides a poor prognosis for patients.
In this study, we investigated the mechanisms of initiation of luminal breast CSCs to understand how those CSCs influence BC late recurrence. First, we analyzed the potency of CSCs and related factors by a mammosphere assay compared to adherent culture BC cells. Under mammosphere culture, we found that CSC populations of luminal BC have increased FOXA1 expression compared with the control population. The FOXA1 knockdown study showed that FOXA1 is involved in the proliferation of immature BC cells rather than the induction of stemness-related genes and self-renewal potency of CSCs. Our findings may therefore help to establish a novel strategy to treat luminal BC and its late recurrence.
Materials and Methods
Cell lines
The MCF-7 and MDA-MB-231 human breast cancer cell lines were purchased from RIKEN BioResource Center (Ibaraki, Japan). HCC1500 human breast cancer cells were purchased from ATCC (Manassas, VA, USA). All cells were cultured in DMEM high glucose medium (Gibco; Thermo Fisher Scientific, Waltham, MA, USA) supplemented with 10% FBS (Thermo Fisher Scientific), l-glutamine, MEM–non-essential amino acid solution, and penicillin/streptomycin. Cells were maintained in a humidified incubator at 37°C at an atmospheric pressure of 5% (v/v) CO2/air.
Patient sample and established cell lines
A surgical breast cancer tissue sample and metastatic pleural effusion from a breast cancer patient (79 years of age, ER [+], PgR [+], HER2 [0]), under aromatase inhibitor treatment, were harvested following the approval of the ethics committee at University of Tsukuba (Tsukuba, Japan). The pleural effusion was treated with RosetteSep Human CD45 Depletion Cocktail (Stemcell Technologies, Vancouver, BC, Canada) according to the manufacturer's instructions. The cells were then laid onto a density gradient buffer (HISTOPAQUE-1083; Sigma-Aldrich, St. Louis, MO, USA) and centrifuged at 460g for 20 min at room temperature. The mononuclear cells were collected and plated at the density of 2 × 105–2 × 106 cells/mL in a 25-cm2 culture flask (Sumitomo Bakelite, Osaka, Japan) and maintained at 37°C in 5% CO2.
Establishment of shFOXA1 cells
We purchased OmicsLink shRNA Expression Clone targeted to FOXA1 and scrambled control gene (GeneCopoeia, Rockville, MD, USA). The shRNA clones were transfected into HEK293T cells using the Lenti-Pac HIV Expression Packaging Kit (GeneCopoeia) and pseudo-viral particles were harvested.
These particles were then transduced into target cells and selected with puromycin. The effect of shRNA of FOXA1 was assessed by an immunoblot analysis.
Flow cytometry
To characterize and analyze BC cells, flow cytometry was used (MoFlo XDP; Beckman Coulter, Tokyo, Japan) with CD44-FITC antibody (BD Biosciences, San Jose, CA, USA) and CD24-PE antibody (BioLegend, San Diego, CA, USA) as previously reported.31 For ALDH activity, an ALDEFLUOR kit (Stemcell Technologies) was used according to the manufacturer's instructions.
Mammosphere formation assay
Mammosphere culture was carried out using MammoCult medium (Stemcell Technologies), hydrocortisone, penicillin/streptomycin, and heparin according to the manufacturer's instructions. Approximately 1 × 104 cells were plated onto 35-mm petri dishes (Sumitomo Bakelite), and the number of mammospheres over 100-μm diameter was counted under a microscope. To analyze the effects of 4-hydroxytamoxifen (4-OHT; Sigma-Aldrich, Tokyo, Japan) on the mammospheres derived from BC cells, a concentration of 1 μM 4-OHT/dish was used.
Colony formation assay
The cells were seeded in triplicate at 100 cells/6-well plate (Sumitomo Bakelite) in complete medium. After 2 weeks, the cells were fixed and stained with 0.5% w/v crystal violet in methanol. Visible colonies were scored by macroscopic observation.
Quantitative RT-PCR
Total RNA was prepared from samples using extraction reagent (Sepasol-RNA I Super G; Nacalai Tesque, Kyoto, Japan), and cDNA was synthesized by reverse transcription using the ReverTra Plus kit (Toyobo, Osaka, Japan). The expression levels of target genes were analyzed using a 7500 Fast Real-Time PCR machine (Applied Biosystems, Foster City, CA, USA) with Thunderbird SYBR qPCR Mix (Toyobo). Experiments were carried out in triplicate and data were calculated using the ΔCt method. The sequences of the primers used for quantitative RT-PCR are shown in Table 1.
| Human Oct4 | Sense: | 5′-CTGGGGGTTCTATTTGGGAAGGTA-3′ |
| Antisense: | 5′-CTGCAGGAACAGATTCTCCAGGTT-3′ | |
| Human Nanog | Sense: | 5′-ACAGAAATACCTCAGCCTCCAGCA-3′ |
| Antisense: | 5′-CTCCAGGTTGAATTGTTCCAGGTC-3′ | |
| Human Sox2 | Sense: | 5′- GAGTGGAAACTTTTGTCGGAGACG-3′ |
| Antisense: | 5′-CCGGTATTTATAATCCGGGTGCTC-3′ | |
| Human ESR1 | Sense: | 5′-ATGTGTAGAGGGCATGGTGGAGAT-3′ |
| Antisense: | 5′-GACTTCAGGGTGCTGGACAGAAAT-3′ | |
| Human FOXA1 | Sense: | 5′-ACTCGTACATCTCGCTCATCACCA-3′ |
| Antisense: | 5′-CAAGTAGCAGCCGTTCTCGAACAT-3′ | |
| Human β-actin | Sense: | 5′-CTGGCACCACACCTTCTACAATGA-3′ |
| Antisense: | 5′-TAGCACAGCCTGGATAGCAACGTA-3′ |
Western blot analysis
Whole cell extract was prepared using RIPA buffer (50 mM Tris, 150 mM NaCl, 0.5% sodium deoxycholate, 1% NP-40, and 0.1% SDS). Samples were electrophoresed on a 7.5% SDS–polyacrylamide gel and transferred onto PVDF membranes (Merck Millipore, Darmstadt, Germany). After blocking with 5% skim milk/TBST buffer, the membranes were incubated with anti-FOXA1 antibody (clone2F83, dilution 1:1000; Abcam, Tokyo, Japan) or anti-actin antibody as control (clone C-11, dilution 1:2000; Santa Cruz Biotechnology, Santa Cruz, CA, USA). After washing, the membranes were incubated with HRP-conjugated secondary antibodies, and positive signals were analyzed by a luminescence imager (Image Quant LAS4000; GE Healthcare, Little Chalfont, UK) using chemiluminescence reagents (Merck Millipore).
Immunohistochemical staining
The cell pellets were fixed in 10% formalin and 70% ethanol. After fixation, samples were embedded in paraffin blocks.
Immunohistochemical staining was carried out by the Translational Research and Resource Core at the University of Tsukuba. Nearly all staining methods, except for HER2, were based on the autostainer BenchMark ULTRA (Roche, Tokyo, Japan) protocols; HER2 was stained as recommended by the supplier. The following antibodies were used: mouse anti-FOXA1 antibody (clone2F83, dilution 1:2000; Abcam); Ventana ultraView confirm ER (clone SP1; Roche); Ventana ultraView confirm PgR (clone 1E2; Roche); Histofine HER2 kit (Nichirei, Tokyo, Japan); cytokeratin (CK) 5/6 (clone D5/16 B4; Dako, Tokyo, Japan); and CK 8 (clone 35H11; Dako).
Growth inhibition curve analysis
To investigate the effects of 4-OHT on cell growth, we modified the method reported previously.35 Both MCF-7 and BC#1 cells were incubated at various concentrations of 4-OHT for 72 h. Cells were harvested and viable cells were counted using the Trypan blue exclusion method.
Statistical analysis
All results are expressed as the means ± SD from three or more independent experiments. A statistical evaluation of the data was carried out using Student's t-test. P-values <0.05 were considered to be significantly different.
We used the GraphPad Prism 6 software program (GraphPad Software, San Diego, CA, USA) for all analyses.
Results
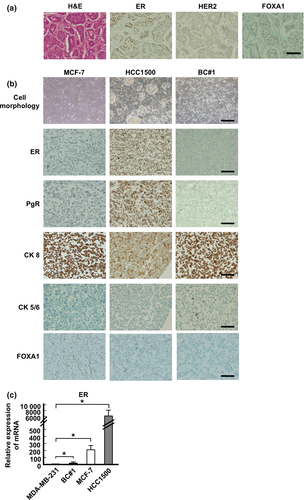
Characteristics of BC-derived cells
To clarify the stemness of luminal BC, we first isolated BC cells from metastatic breast cancer pleural effusion and characterized them. Immunohistochemical staining of the surgical tissue is shown in Figure 1(a): ER-positive, HER2-negative, and FOXA1-positive staining was evident in approximately 80–90% of cells. NANOG, OCT4, and SOX2 were not stained in the tissue sample (data not shown). In newly isolated cells, named BC#1 cells, ER was not expressed, whereas PgR was expressed in nearly 80% by immunohistochemical staining (Fig. 1b, Table 2). As the PgR expression in the tumor has been determined to be an indication of functional ER,36, 37 we analyzed the expression of ER in BC#1 cells. BC#1 cells were negative for ER according to immunohistochemical staining, whereas ER mRNA expression was higher in BC#1 than in MDA-MB-231 cells (Fig. 1c). The reason behind the decreased ER expression of BC#1 was surmised as follows. It has been reported that the hormone receptor discordance between primary and recurrent BC has occurred at the frequency of 10–40%, because of the change in tumor characteristics after treatment.38 In addition, it is known that long-term estrogen deprivation in culture causes the instability of ER expression in vitro.39 These factors might cause the discrepancy of the ER expression in BC#1 cells isolated from the pleural effusion. According to epithelial markers, approximately 100% of BC#1 cells were strongly positive for CK 8 and partially positive for CK 5/6. Therefore, we confirmed that there is little contamination of the non-epithelial population in BC#1 cells. MCF-7 and HCC1500 cells were positive for CK 8 (Fig. 1b, Table 2). We next examined FOXA1 expression by immunohistochemical staining. FOXA1 was positively expressed in MCF-7 and HCC1500 cells, but not in BC#1 cells (Fig. 1b).
| Cell line (ATCC name) | ER | PgR | HER2 | CK 8 | CK 5/6 |
|---|---|---|---|---|---|
| MCF7 (HTB-22) | + | + | − | + | − |
| HCC1500 (CRL-2329) | + | + | − | + | − |
| BC#1 | − | + | − | + | + |
- +, Positively expressed; −, no expression. CK, cytokeratin; ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; PgR, progesterone receptor.
According to these findings, the newly isolated BC#1 cells were categorized into the luminal type of BC cells and were found to express different characteristics from commercially available BC cell lines.
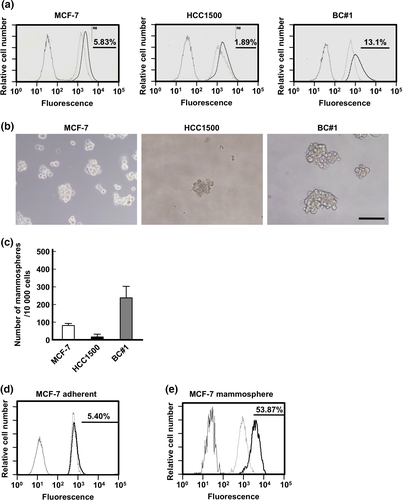
Expression of stemness markers and mammosphere forming capacity of different luminal BC cells
We evaluated the ALDH activity and frequency of CD44+/24− cells in our luminal BC cell lines (Figs 2a, S1). We found that BC#1 contains CSC populations at the highest frequency among the three BC cell lines investigated. The number of mammospheres was the highest in BC#1 compared to the other two BC cell lines (Fig. 2b and 2c). It has been previously reported that the changing of culture conditions from regular adherent culture to mammosphere culture led to the elevated expression of genes related to stemness.17 As shown in Figure 2(d,e), under a mammosphere culture, ALDH-positive MCF-7 cells increased compared to MCF-7 cells cultured under adherent conditions.
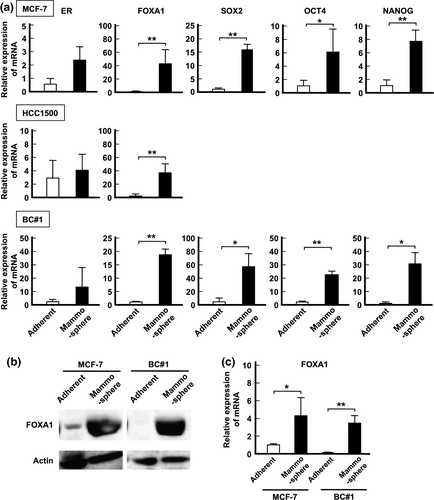
Mammosphere culture causes ectopic expression of FOXA1 and stemness-related genes
First, the mRNA expression of ER, FOXA1, and stemness-related genes NANOG, SOX2, and OCT4 were analyzed by quantitative PCR analyses.28, 40-42 There was no significant difference in the expression of ER between mammosphere and adhesion cultured cells. In contrast, the expression of FOXA1 under mammosphere culture was significantly higher than that under adherent culture (Fig. 3a). Similar to FOXA1 expression, stemness-related genes were highly expressed in MCF-7 and BC#1 cell lines under mammosphere culture compared to those under an adherent culture. Because lower mammosphere formation was observed in HCC1500 compared to that of MCF-7 and BC#1 cell lines, we could not harvest sufficient samples for the analysis of gene expression. A Western blot analysis clearly indicated that FOXA1 protein expression was highly upregulated in both MCF-7 and BC#1 cell lines under mammosphere culture compared to adherent culture (Fig. 3b).
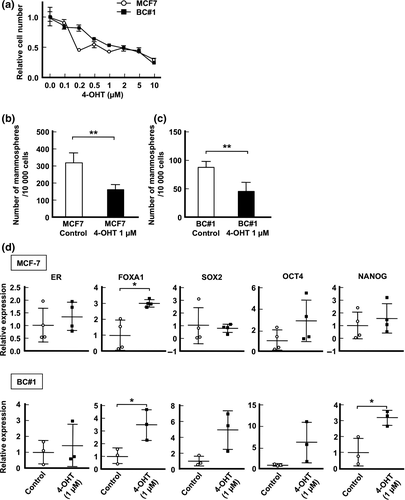
Ectopic FOXA1 expression in mammospheres is correlated to 4-OHT resistance
The correlation between drug therapy resistance and FOXA1 has also been reported previously.34, 43, 44 To determine the concentration of 4-OHT for BC cell resistance, we examined the proliferative activity of MCF-7 and BC#1 cell lines in the presence of various concentrations of 4-OHT. As shown in Figure 4(a), both MCF-7 and BC#1 cells tended to maintain growth activity over 50% when 4-OHT was added at a concentration less than 1 μM. No significant morphologic changes were observed in MCF-7 or BC#1 cell lines (data not shown). Therefore, we used 4-OHT at the concentration of 1 μM in this study. Next, we examined the effect of 4-OHT on mammosphere culture. The number of mammospheres in MCF-7 and BC#1 cell lines drastically decreased in the presence of 4-OHT (Fig. 4b,c). The expression of ER mRNA and stemness-related genes in mammospheres from MCF-7 and BC#1 cells did not differ according to the presence or absence of 4-OHT. In contrast, FOXA1 mRNA expression of 4-OHT-treated mammospheres was significantly higher than that of the control (MCF-7, P = 0.0210; BC#1, P = 0.0353; Fig. 4d).
Knockdown expression of FOXA1 does not correlate with expression of stemness-related genes
To investigate the effect of FOXA1 on the expression of stemness-related genes or mammosphere forming cells, we established FOXA1 knockdown MCF-7 cells (shFOXA1 MCF-7 cells, Fig. 5a). These cells showed downregulated ER and AGR2 expression, which have been reported to be downstream of FOXA1.45 However, the expression of stemness-related genes, NANOG and OCT4, was maintained at a high level compared to the control (Fig. 5b). No significant difference in the number of mammospheres between shFOXA1 and control cells was observed (Fig. 5c), suggesting that FOXA1 may not affect the generation of CSCs. The colony formation assay is widely used to evaluate the proliferative ability of immature cells.28, 46 As shown in Figure 5(d,e), the number of colonies derived from shFOXA1 MCF-7 cells significantly decreased compared to control cells.
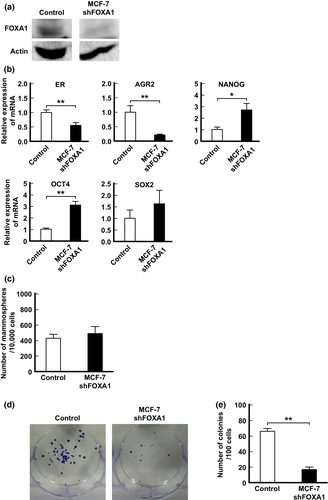
Taken together, these findings indicate that FOXA1 appears to work as a factor in the proliferation rather than maintenance of stemness-related genes or the activation of CSCs.
Discussion
Understanding the characteristics and properties of CSCs is crucial for clinical application. Metastases and recurrence are known to correlate with CSCs, and chemotherapeutic resistance and endocrine therapy-resistance of BC are generally known to correlate with CSC populations.47-50 Therefore, CSCs are the major challenge in BC treatment difficulties.
One of the methods to assess the potency of CSCs is the mammosphere assay. Mammosphere culture was first reported by Dontu et al.17 to evaluate the potency of progenitor/stem cells. A correlation has also been shown between mammospheres and epithelial–mesenchymal transition51-53 and drug resistance.53 Thus, we speculated that analyses of BC colonies formed under the mammosphere assay would elucidate the mechanism by which CSCs in luminal BC arise. In order to enrich BC cells for CSC populations, mammosphere culture was used and investigated in this study. Harrison et al.54 previously showed that the CD44+/CD24− population generates more mammospheres than other cell populations. Furthermore, it has been reported that an assessment of mammospheres could be useful to predict prognosis.55 In this study, we determined that both established BC cell lines and commercially established BC cell lines had CSC marker positive populations and could form mammospheres. Each mammosphere showed high expression of stemness-related genes, such as NANOG, SOX2, and OCT4. Interestingly, mammosphere-forming cells showed high expression of FOXA1 mRNA and protein compared to adherent culture samples. By contrast, BC#1 cells in adherent culture did not express FOXA1 according to immunohistochemical staining and Western blotting analyses. These findings suggest that CSCs cultured under specific culture atmospheres increase the CSC population and induce stemness-related genes as well as FOXA1 expression.
Because BC is composed of various subtypes, the FOXA1 expression determined by immunohistochemical staining was observed in the majority of the luminal subtype. Therefore, we hypothesized that the prognosis of the luminal subtype regarding FOXA1 expression would be superior to other types. Indeed, a tissue analysis by immunohistochemical staining showed that FOXA1 is a good prognosis marker of formalin-fixed paraffin-embedded tissue staining.33, 44, 56 It has also been reported that late recurrence also tends to occur in luminal BC,7 not in other subtypes. Some studies also show that FOXA1 expression correlates with metastatic lesions of luminal BC.34, 57 Furthermore, Ross-Innes et al.57 showed that there are specific and reoccurring cis-regulatory elements that are occupied by ER in BC; however, these vary according to good and poor outcome samples, and FOXA1 mediates ER reprogramming. The ectopic expression of FOXA1 observed in our study may correlate with this mechanism.
Drug resistance is a significant problem that influences the CSC ability. Raffo et al.47 compared the mammosphere formation capacity and in vivo tumorigenicity between parental MCF-7 and 4-OHT-resistant MCF-7 cells and showed that 4-OHT-resistant MCF-7 cells had an increased mammosphere number and tumorigenicity compared to parent MCF-7 cells. Moreover, Calcagno et al.48 reported that doxorubicin-resistant MCF-7 cells showed high stemness potential using a mammosphere assay, CSC markers, and tumorigenicity. Lin et al.58 described that tamoxifen-resistant BC cells possibly emerge from CSC populations by validating the DNA methylation and SOX2 gene expression. In our study, the colony-forming activity of 4-OHT-treated BC cells was inhibited in the mammosphere assay. Interestingly, 4-OHT-resistant cells had significantly increased FOXA1. Moreover, we established shFOXA1 MCF-7 cells and investigated the relationship between their self-renewal potential and FOXA1 expression. As a result, the number of mammospheres was not significantly different between shFOXA1 MCF-7 cells and control cells. We also observed decreased colony formation in shFOXA1 MCF-7 cells than control cells, indicating the contribution of specific culture conditions in the mammosphere assay to activate CSCs formation.
In conclusion, our findings showed for the first time that the CSC population in luminal BC induces ectopic expression of FOXA1. The expression of FOXA1 appears to be involved in the proliferation of immature BC cells rather than the induction of stemness-related genes and self-renewal potency of CSCs.
Further studies are necessary to investigate the process of ectopic FOXA1 expression in BC development and its biological influence. These findings are thus expected to help establish a novel strategy to treat luminal BC and its late recurrence.
Acknowledgments
This work was supported by a Grant-in Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Disclosure Statement
The authors have no conflict of interest.