Neurofilament light chain: A potential biomarker for cerebrovascular disease in children with sickle cell anaemia
Corresponding Author
Nancy S. Green
Department of Pediatrics, Columbia University Irving Medical Center, New York, New York, USA
Correspondence
Nancy S. Green, Department of Pediatrics, Columbia University Medical Center, New York, NY, USA.
Email: [email protected]
Search for more papers by this authorCaterina Rosano
Department of Epidemiology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
Search for more papers by this authorPaul Bangirana
Department of Psychiatry, Makerere University College of Health Sciences, Kampala, Uganda
Global Health Uganda, Kampala, Uganda
Search for more papers by this authorRobert Opoka
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorDeogratias Munube
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorPhilip Kasirye
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorMichael Kawooya
Department of Radiology, Makerere University College of Health Sciences, Kampala, Uganda
Ernest Cook Ultrasound Research and Education Institute (ECUREI), Mengo Hospital, Kampala, Uganda
Search for more papers by this authorSamson K. Lubowa
Department of Radiology, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorEzekiel Mupere
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorAndrea Conroy
Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana, USA
Search for more papers by this authorFrank J. Minja
Department of Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, Georgia, USA
Search for more papers by this authorAmelia K. Boehme
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorMin Suk Kang
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorLawrence S. Honig
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorRichard Idro
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorCorresponding Author
Nancy S. Green
Department of Pediatrics, Columbia University Irving Medical Center, New York, New York, USA
Correspondence
Nancy S. Green, Department of Pediatrics, Columbia University Medical Center, New York, NY, USA.
Email: [email protected]
Search for more papers by this authorCaterina Rosano
Department of Epidemiology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
Search for more papers by this authorPaul Bangirana
Department of Psychiatry, Makerere University College of Health Sciences, Kampala, Uganda
Global Health Uganda, Kampala, Uganda
Search for more papers by this authorRobert Opoka
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorDeogratias Munube
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorPhilip Kasirye
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorMichael Kawooya
Department of Radiology, Makerere University College of Health Sciences, Kampala, Uganda
Ernest Cook Ultrasound Research and Education Institute (ECUREI), Mengo Hospital, Kampala, Uganda
Search for more papers by this authorSamson K. Lubowa
Department of Radiology, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorEzekiel Mupere
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorAndrea Conroy
Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana, USA
Search for more papers by this authorFrank J. Minja
Department of Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, Georgia, USA
Search for more papers by this authorAmelia K. Boehme
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorMin Suk Kang
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorLawrence S. Honig
Department of Neurology, Columbia University Irving Medical Center, New York, New York, USA
Search for more papers by this authorRichard Idro
Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Kampala, Uganda
Search for more papers by this authorSummary
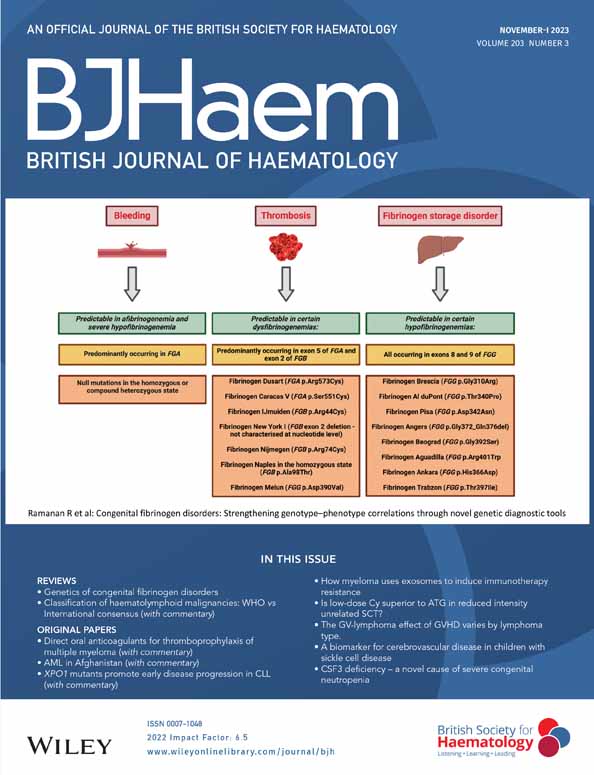
Cerebrovascular injury frequently occurs in children with sickle cell anaemia (SCA). Limited access to magnetic resonance imaging and angiography (MRI-MRA) in sub-Saharan Africa impedes detection of clinically unapparent cerebrovascular injury. Blood-based brain biomarkers of cerebral infarcts have been identified in non-SCA adults. Using plasma samples from a well-characterized cross-sectional sample of Ugandan children with SCA, we explored relationships between biomarker levels and MRI-detected cerebral infarcts and transcranial Doppler (TCD) arterial velocity. Testing was performed using a 4-plex panel of brain injury biomarkers, including neurofilament light chain (NfL), a central nervous system neuron-specific protein. Mean biomarker levels from the SCA group (n = 81) were similar to those from non-SCA sibling controls (n = 54). Within the SCA group, NfL levels were significantly higher in those with MRI-detected infarcts compared to no infarcts, and higher with elevated TCD velocity versus normal velocity. Elevated NfL remained strongly associated with MRI-detected infarcts after adjusting for sex and age. All non-SCA controls and SCA participants lacking MRI-detected infarcts had low NfL levels. These data suggest potential utility of plasma-based NfL levels to identify children with SCA cerebrovascular injury. Replication and prospective studies are needed to confirm these novel findings and the clinical utility of NfL versus MRI imaging.
Graphical Abstract
CONFLICT OF INTEREST STATEMENT
The authors have no relevant conflicts to disclose.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is available upon request to the corresponding author, except where data access is restricted for protection of the privacy of research participants.
Supporting Information
| Filename | Description |
|---|---|
| bjh19036-sup-0001-TableS1.docxWord 2007 document , 16.9 KB |
Table S1. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Ohene-Frempong K, Weiner SJ, Sleeper LA, Miller ST, Embury S, Moohr JW, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998; 91(1): 288–294.
- 2Kirkham FJ, Lagunju IA. Epidemiology of stroke in sickle cell disease. J Clin Med. 2021; 10(18):4232.
- 3Ali SB, Moosang M, King L, Knight-Madden J, Reid M. Stroke recurrence in children with sickle cell disease treated with hydroxyurea following first clinical stroke. Am J Hematol. 2011; 86(10): 846–850.
- 4Nichols FT, Jones AM, Adams RJ. Stroke prevention in sickle cell disease (STOP) study guidelines for transcranial Doppler testing. J Neuroimaging. 2001; 11(4): 354–362.
- 5Ambrose EE, Latham TS, Songoro P, Charles M, Lane AC, Stuber SE, et al. Hydroxyurea with dose escalation for primary stroke risk reduction in children with sickle cell anaemia in Tanzania (SPHERE): an open-label, phase 2 trial. Lancet Haematol. 2023; 10: e261–e271.
- 6Abdullahi SU, Jibir BW, Bello-Manga H, Gambo S, Inuwa H, Tijjani AG, et al. Hydroxyurea for primary stroke prevention in children with sickle cell anaemia in Nigeria (SPRING): a double-blind, multicentre, randomised, phase 3 trial. Lancet Haematol. 2022; 9(1): e26–e37.
- 7Lagunju I, Brown BJ, Oyinlade AO, Asinobi A, Ibeh J, Esione A, et al. Annual stroke incidence in Nigerian children with sickle cell disease and elevated TCD velocities treated with hydroxyurea. Pediatr Blood Cancer. 2019; 66(3):e27252.
- 8Opoka RO, Hume HA, Latham TS, Lane A, Williams O, Tymon J, et al. Hydroxyurea to lower transcranial Doppler velocities and prevent primary stroke: the Uganda NOHARM sickle cell anemia cohort. Haematologica. 2020; 105(6): e272–e275.
- 9Brousse V, Kossorotoff M, de Montalembert M. How I manage cerebral vasculopathy in children with sickle cell disease. Br J Haematol. 2015; 170(5): 615–625.
- 10Houwing ME, Grohssteiner RL, Dremmen MHG, Atiq F, Bramer WM, de Pagter APJ, et al. Silent cerebral infarcts in patients with sickle cell disease: a systematic review and meta-analysis. BMC Med. 2020; 18(1): 393.
- 11DeBaun MR, Kirkham FJ. Central nervous system complications and management in sickle cell disease. Blood. 2016; 127(7): 829–838.
- 12DeBaun MR, Armstrong FD, McKinstry RC, Ware RE, Vichinsky E, Kirkham FJ. Silent cerebral infarcts: a review on a prevalent and progressive cause of neurologic injury in sickle cell anemia. Blood. 2012; 119(20): 4587–4596.
- 13Pegelow CH, Macklin EA, Moser FG, Wang WC, Bello JA, Miller ST, et al. Longitudinal changes in brain magnetic resonance imaging findings in children with sickle cell disease. Blood. 2002; 99(8): 3014–3018.
- 14Kija EN, Saunders DE, Munubhi E, Darekar A, Barker S, Cox TCS, et al. Transcranial Doppler and magnetic resonance in Tanzanian children with sickle cell disease. Stroke. 2019; 50(7): 1719–1726.
- 15Jacob M, Stotesbury H, Kija E, Saunders D, Mtei RJ, Tutuba H, et al. Effect of age, cerebral infarcts, vasculopathy and haemoglobin on cognitive function, in Tanzanian children with sickle cell anaemia. Eur J Paediatr Neurol. 2022; 37: 105–113.
- 16Choi S, O'Neil SH, Joshi AA, Li J, Bush AM, Coates TD, et al. Anemia predicts lower white matter volume and cognitive performance in sickle and non-sickle cell anemia syndrome. Am J Hematol. 2019; 94(10): 1055–1065.
- 17Choudhury NA, DeBaun MR, Ponisio MR, Jordan LC, Rodeghier M, Pruthi S, et al. Intracranial vasculopathy and infarct recurrence in children with sickle cell anaemia, silent cerebral infarcts and normal transcranial Doppler velocities. Br J Haematol. 2018; 183(2): 324–326.
- 18Wang WC, Gallagher DM, Pegelow CH, Wright EC, Vichinsky EP, Abboud MR, et al. Multicenter comparison of magnetic resonance imaging and transcranial Doppler ultrasonography in the evaluation of the central nervous system in children with sickle cell disease. J Pediatr Hematol Oncol. 2000; 22(4): 335–339.
- 19Green NS, Munube D, Bangirana P, Buluma LR, Kebirungi B, Opoka R, et al. Burden of neurological and neurocognitive impairment in pediatric sickle cell anemia in Uganda (BRAIN SAFE): a cross-sectional study. BMC Pediatr. 2019; 19(1): 381.
- 20Idro R, Boehme AK, Kawooya M, Lubowa SK, Munube D, Bangirana P, et al. Brain magnetic resonance imaging and angiography in children with sickle cell Anaemia in Uganda in a cross-sectional sample. J Stroke Cerebrovasc Dis. 2022; 31(4):106343.
- 21Jacob M, Stotesbury H, Kawadler JM, Lapadaire W, Saunders DE, Sangeda RZ, et al. White matter integrity in Tanzanian children with sickle cell anemia: a diffusion tensor imaging study. Stroke. 2020; 51(4): 1166–1173.
- 22Dhana A, DeCarli C, Aggarwal NT, Dhana K, Desai P, Evans DA, et al. Serum neurofilament light chain, brain infarcts, and the risk of stroke: a prospective population-based cohort study. Eur J Epidemiol. 2023; 38: 427–434.
- 23Heshmatollah A, Fani L, Koudstaal PJ, Ghanbari M, Ikram MA, Ikram MK. Plasma beta-amyloid, Total-tau, and neurofilament light chain levels and the risk of stroke: a prospective population-based study. Neurology. 2022; 98(17): e1729–e1737.
- 24Cabezas JA, Bustamante A, Giannini N, Pecharroman E, Katsanos AH, Tsivgoulis G, et al. Discriminative value of glial fibrillar acidic protein (GFAP) as a diagnostic tool in acute stroke. Individual patient data meta-analysis. J Investig Med. 2020; 68(8): 1379–1385.
- 25Liu D, Chen J, Wang X, Xin J, Cao R, Liu Z. Serum neurofilament light chain as a predictive biomarker for ischemic stroke outcome: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2020; 29(6):104813.
- 26Benkert P, Meier S, Schaedelin S, Manouchehrinia A, Yaldizli O, Maceski A, et al. Serum neurofilament light chain for individual prognostication of disease activity in people with multiple sclerosis: a retrospective modelling and validation study. Lancet Neurol. 2022; 21(3): 246–257.
- 27Teunissen CE, Verberk IMW, Thijssen EH, Vermunt L, Hansson O, Zetterberg H, et al. Blood-based biomarkers for Alzheimer's disease: towards clinical implementation. Lancet Neurol. 2022; 21(1): 66–77.
- 28Fink EL, Kochanek PM, Panigrahy A, Beers SR, Berger RP, Bayir H, et al. Association of blood-based brain injury biomarker concentrations with outcomes after pediatric cardiac arrest. JAMA Netw Open. 2022; 5(9):e2230518.
- 29Savage WJ, Barron-Casella E, Fu Z, Dulloor P, Williams L, Crain BJ, et al. Plasma glial fibrillary acidic protein levels in children with sickle cell disease. Am J Hematol. 2011; 86(5): 427–429.
- 30Shabani E, Ouma BJ, Idro R, Bangirana P, Opoka RO, Park GS, et al. Elevated cerebrospinal fluid tumour necrosis factor is associated with acute and long-term neurocognitive impairment in cerebral malaria. Parasite Immunol. 2017; 39(7): e12438.
- 31Helton KJ, Adams RJ, Kesler KL, Lockhart A, Aygun B, Driscoll C, et al. Magnetic resonance imaging/angiography and transcranial Doppler velocities in sickle cell anemia: results from the SWiTCH trial. Blood. 2014; 124(6): 891–898.
- 32Anderson AM, Easley KA, Kasher N, Franklin D, Heaton RK, Zetterberg H, et al. Neurofilament light chain in blood is negatively associated with neuropsychological performance in HIV-infected adults and declines with initiation of antiretroviral therapy. J Neurovirol. 2018; 24(6): 695–701.
- 33Brickman AM, Manly JJ, Honig LS, Sanchez D, Reyes-Dumeyer D, Lantigua RA, et al. Plasma p-tau181, p-tau217, and other blood-based Alzheimer's disease biomarkers in a multi-ethnic, community study. Alzheimers Dement. 2021; 17(8): 1353–1364.
- 34Correia M, Silva I, Gabriel D, Simren J, Carneiro A, Ribeiro S, et al. Early plasma biomarker dynamic profiles are associated with acute ischemic stroke outcomes. Eur J Neurol. 2022; 29(6): 1630–1642.
- 35Gattringer T, Pinter D, Enzinger C, Seifert-Held T, Kneihsl M, Fandler S, et al. Serum neurofilament light is sensitive to active cerebral small vessel disease. Neurology. 2017; 89(20): 2108–2114.
- 36Sanchez JD, Martirosian RA, Mun KT, Chong DS, Llorente IL, Uphaus T, et al. Temporal patterning of neurofilament light as a blood-based biomarker for stroke: a systematic review and meta-analysis. Front Neurol. 2022; 13:841898.
- 37Abdelhak A, Foschi M, Abu-Rumeileh S, Yue JK, D'Anna L, Huss A, et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat Rev Neurol. 2022; 18(3): 158–172.
- 38Datta D, Bangirana P, Opoka RO, Conroy AL, Co K, Bond C, et al. Association of plasma tau with mortality and long-term neurocognitive impairment in survivors of pediatric cerebral malaria and severe malarial anemia. JAMA Netw Open. 2021; 4(12):e2138515.
- 39Medana IM, Idro R, Newton CR. Axonal and astrocyte injury markers in the cerebrospinal fluid of Kenyan children with severe malaria. J Neurol Sci. 2007; 258(1–2): 93–98.
- 40Liu H, Povysheva N, Rose ME, Mi Z, Banton JS, Li W, et al. Role of UCHL1 in axonal injury and functional recovery after cerebral ischemia. Proc Natl Acad Sci U S A. 2019; 116(10): 4643–4650.
- 41Sherwani RAK, Shakeel H, Awan WB, Faheem M, Aslam M. Analysis of COVID-19 data using neutrosophic Kruskal Wallis H test. BMC Med Res Methodol. 2021; 21(1): 215.
- 42Berry KJ, Mielke PW. Exact and Monte Carlo resampling procedures for the Wilcoxon-Mann-Whitney and Kruskal-Wallis tests. Percept Mot Skills. 2000; 91(3 Pt 1): 749–754.
- 43Ludbrook J. Multiple comparison procedures updated. Clin Exp Pharmacol Physiol. 1998; 25(12): 1032–1037.
- 44He WC, Zhang XJ, Zhang YQ, Zhang WJ. Elevated serum neurofilament light chain in children autism spectrum disorder: a case control study. Neurotoxicology. 2020; 80: 87–92.
- 45Simone M, De Giacomo A, Palumbi R, Palazzo C, Lucisano G, Pompamea F, et al. Serum neurofilament light chain and glial fibrillary acidic protein as potential diagnostic biomarkers in autism spectrum disorders: a preliminary study. Int J Mol Sci. 2023; 24(3):3057.
- 46Wu J, Wu D, Liang Y, Zhang Z, Zhuang L, Wang Z. Plasma neurofilament light chain: a biomarker predicting severity in patients with acute ischemic stroke. Medicine (Baltimore). 2022; 101(26):e29692.
- 47Lance EI, Casella JF, Everett AD, Barron-Casella E. Proteomic and biomarker studies and neurological complications of pediatric sickle cell disease. Proteomics Clin Appl. 2014; 8(11–12): 813–827.
- 48Chambliss C, Richardson T, Onyekaba J, Cespedes J, Nti A, Harp KO, et al. Elevated neuregulin-1beta levels correlate with plasma biomarkers of cerebral injury and high stroke risk in children with sickle cell anemia. Endocr Metab sci. 2021; 3: 3.
10.1016/j.endmts.2021.100088 Google Scholar
- 49Mahmoud AA, Abd El Naby SA, Abdelgawad AS, Rizq MS, Abd El Hady NMS. Brain-derived neurotrophic factor and neuroimaging in pediatric patients with sickle cell disease. Pediatr Res. 2023; 93: 1922–1926.
- 50Gao W, Zhang Z, Lv X, Wu Q, Yan J, Mao G, et al. Neurofilament light chain level in traumatic brain injury: a system review and meta-analysis. Medicine (Baltimore). 2020; 99(38):e22363.
- 51Galadanci AA, Galadanci NA, Jibir BW, Abdullahi SU, Idris N, Gambo S, et al. Approximately 40 000 children with sickle cell anemia require screening with TCD and treating with hydroxyurea for stroke prevention in three states in northern Nigeria. Am J Hematol. 2019; 94(11): E305–E307.
- 52Pafiti A, Krashias G, Tzartos J, Tzartos S, Stergiou C, Gaglia E, et al. A comparison of two analytical approaches for the quantification of neurofilament light chain, a biomarker of axonal damage in multiple sclerosis. Int J Mol Sci. 2023; 24(13):10787.