A comparison of the International Consensus and 5th WHO classifications of T-cell lymphomas and histiocytic/dendritic cell tumours
Summary
Since the publication in 2017 of the revised 4th Edition of the World Health Organization (WHO) classification of haematolymphoid tumours, here referred to as WHO-HAEM4, significant clinicopathological, immunophenotypic and molecular advances have been made in the field of lymphomas, contributing to refining the diagnostic criteria of several diseases, upgrading entities previously defined as provisional and identifying new entities. This process has resulted in two recent classification proposals of lymphoid neoplasms: the International Consensus Classification (ICC) and the 5th edition of the WHO classification (WHO-HAEM5). In this paper, we review and compare the two classifications in terms of diagnostic criteria and entity definition, focusing on T-cell lymphomas and histiocytic/dendritic cell tumours. Moreover, we update the genetic data of the various pathological entities. The main goal is to provide a tool to facilitate the work of the pathologists, haematologists and researchers involved in the diagnosis and treatment of these haematological malignancies.
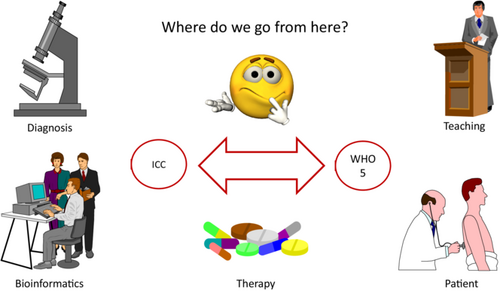
Graphical Abstract
INTRODUCTION
The revised 4th Edition of the World Health Organization (WHO) classification of haematolymphoid neoplasms, here referred to as WHO-HAEM4, was published in 2017 and served as the international standard for diagnosis and research.1 In 2022, two classifications of haematolymphoid tumours were proposed, named as the International Consensus Classification (ICC) and 5th edition of the WHO classification (WHO-HAEM5).2-7 The ICC has been published in its definitive format, whilst there has only been a preview of the WHO-HAEM5 Blue Book, which is already online as an Internet-based homepage.
As compared to WHO-HAEM4, there have been several changes to the ICC2 and WHO-HAEM5 that include differences in terminology and the addition/upgrading of entities, mainly based on progress in molecular studies.2-7 Moreover, criteria and recommended ancillary studies were refined in both classifications.
Recently, we compared the ICC and WHO-HAEM5 classifications of mature B-cell neoplasms.5 Here, we review and compare the two classifications in terms of diagnostic criteria and entity definition (Table 1), focusing on T-cell lymphomas and histiocytic/dendritic cell neoplasms. Moreover, we update the genetic data of the various pathological entities. The main aim is to provide a tool to pathologists, haematologists and researchers involved in the diagnosis and therapy of these tumours.
| WHO-HAEM4 | ICC 2022 | WHO-HAEM5 |
|---|---|---|
| Precursor lymphoid neoplasms | Precursor T-cell neoplasms | Precursor T-cell neoplasms |
| T-lymphoblastic leukemia/lymphoma | T-lymphoblastic leukemia/lymphoma, NOS | T-lymphoblastic leukemia/lymphoma, NOS |
| Early T-cellprecursor-lymphoblastic leukemia/lymphoma | Early T-cell precursor-lymphoblastic leukemia/lymphoma, NOS | Early T precursor-lymphoblastic leukemia/lymphoma |
| Not considered | Early T-cell precursor-lymphoblastic leukemia/lymphoma with BCL11B rearrangement | Not considered |
| NK-lymphoblastic leukemia /lymphoma (provisional entity) | NK-lymphoblastic leukemia /lymphoma (provisional entity) | Entity deleted |
| Mature T and NK-cell neoplasms | Mature T and NK-cell neoplasms | Mature T-cell and NK-cell neoplasms |
| Not considered | Not considered | Mature T-cell and NK-cell leukemia |
| T-cell prolymphocytic leukemia | T-cell prolymphocytic leukemia | T-prolymphocytic leukemia |
| T-cell large granular lymphocytic leukemia | T.cell large granular lymphocytic leukemia | T-large granular lymphocytic leukemia |
| Aggressive NK leukemia | Aggressive NK leukemia | Aggressive NK-cell leukemia |
| Adult T-cell leukemia/lymphoma | Adult T-cell leukemia/lymphoma | Adult T-cell leukemia/lymphoma |
| Chronic lymphoproliferative disorder of NK cells (provisional) | Chronic lymphoproliferative disorder of NK cells (provisional) | NK-large granular lymphocytic leukemia |
| See later | See later | Sézary syndrome |
| EBV+T-cell and NK-cell LPD of childhood | EBV+ T/ NK-cell LPD of childhood | EBV+ T and NK-cell LP and lymphomas of childhood |
| Hydroa Vacciniforme-like LPD | Hydroa Vacciniforme LPD | Hydroa Vacciniforme LPD |
| Severe mosquito bite allergy | Severe mosquito bite allergy | Severe mosquito bite allergy |
| Chronic active EBV infection of T and NK-cell type, systemic form | Chronic active EBV disease, systemic(T and NK-cellphenotype) | Systemic chronic active EBV disease |
| Systemic EBV+T-cell lymphoma of childhood | Systemic EBV+T-cell lymphoma of childhood | Systemic EBV+ T-cell lymphoma of childhood |
| Not considered | Not considered | EBV positive NK/T-cell lymphomas |
| Primary EBV positive nodal T-cell or NK cell lymphoma (variant of PTCL, NOS) | Primary nodal EBV positive T-cell/NK cell lymphoma (provisional entity) | EBV-positive nodal T-and NK-cell lymphoma |
| Extranodal NK/T-cell lymphoma, nasal type | Extranodal NK/T-cell lymphoma, nasal type | Extranodal NK/T-cell lymphoma |
| Intestinal T-cell lymphoma | Intestinal T-cell lymphoma | Intestinal T-cell and NK-cell lymphoid proliferations and lymphomas |
| Enteropathy-associated T-cell lymphoma (EATL) | Enteropathy-associated T-cell lymphoma (EATL) | Enteropathy-associated T-cell lymphoma (EATL) |
| -Not reported | -Type II refractory coeliac disease (precursor of EATL) | -Not reported |
| Monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL) | Monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL) | Monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL) |
| Intestinal T-cell lymphoma, NOS | Intestinal T-cell lymphoma, NOS | Intestinal T-cell lymphoma, NOS |
| Indolent T-cell LPD of the gastrointestinal tract | Indolent clonal T-cell LPD of the gastrointestinal tract | Indolent T-cell lymphoma of the gastrointestinal tract |
| Not considered | Indolent NK-cell LPD of the gastrointestinal tract | Indolent NK-cell LPD of the gastrointestinal tract |
| Not considered | Not considered | Hepatosplenic T-cell lymphoma |
| Hepatosplenic T-cell lymphoma | Hepatosplenic T-cell lymphoma | Hepatosplenic T-cell lymphoma |
| Not considered | Not considered | Primary cutaneous T-cell lymphoma |
| Mycosis fungoides | Mycosis fungoides | Mycosis fungoides |
| Sézary syndrome | Sézary syndrome | Classified in mature T-cell and NK-cell leukemia (see above) |
| Subcutaneous panniculitis-like T-cell lymphoma | Subcutaneous panniculitis-like T-cell lymphoma | Subcutaneous panniculitis-like T-cell lymphoma |
| Primary cutaneous CD30+ T-cell LPD: | Primary cutaneous CD30+ T-cell LPD: | Primary cutaneous CD30+ T-cell LPD: |
| -Lymphomatoid papulosis | -Lymphomatoid papulosis | -Lymphomatoid papulosis |
| -Primary cutaneous ALCL | -Primary cutaneous ALCL | -Primary cutaneous ALCL |
| Primary cutaneous peripheral T-cell lymphomas, rare subtypes: | Not considered | Not considered |
| -Primary cutaneous gamma delta T-cell lymphoma | Primary cutaneous gamma-delta T-cell lymphoma | Primary cutaneous gamma/delta T-cell lymphoma |
| -Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma | Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma | Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma |
| -Primary cutaneous acral CD8+ lymphoma | Primary cutaneous acral CD8+ LPD | Primary cutaneous acral CD8+ LPD |
| -Primary cutaneous CD4+small/medium T-cell LPD | Primary cutaneous CD4+small/medium T-cell LPD | Primary cutaneous CD4+ small or medium T-cell LPD |
| Not considered | Not considered | Primary cutaneous peripheral T-cell lymphoma, NOS |
| Angioimmunoblastic T-cell lymphoma and other nodal lymphomas of T follicular helper (TFH) cell origin | Follicular helper T-cell lymphoma | Nodal T follicular helper (TFH) cell lymphoma |
| -AngioimmunoblasticT-cell lymphoma | -Angioimmunoblastic type | -Angioimmunoblastic type |
| -Follicular T-cell lymphoma | -Follicular type | -Follicular type |
| -Nodal peripheral T-cell lymphoma with T follicular helper phonotype | -Not otherwise specified (NOS) | -Not otherwise specified (NOS) |
| Not considered | Not considered | Anaplastic large cell lymphoma |
| Anaplastic large cell lymphoma, ALK positive | Anaplastic large cell lymphoma, ALK positive | ALK-positive anaplastic large cell lymphoma |
| Anaplastic large cell lymphoma ALK-negative | Anaplastic large cell lymphoma ALK-negative | ALK-negative anaplastic large cell lymphoma |
| Breast implant-associatedanaplastic large cell lymphoma (provisional entity) | Breast implant-associated anaplastic large cell lymphoma (definite entity) | Breast implant-associatedanaplastic large cell lymphoma (definite entity) |
| Not considered | Not considered | Other peripheral T-cell lymphoma |
| Peripheral T-cell lymphoma, NOS | Peripheral T-cell lymphoma, NOS | Peripheral T-cell lymphoma, NOS |
| Histiocytic and dendritic cell neoplasms | Histiocytic and dendritic cell neoplasms | (Myeloid) and histiocytic/dendritic neoplasms |
| Tumors derived from Langerhans cells: | Tumors derived from Langerhans cells: | Langerhans cell and other dendritic cell neoplasms: |
| -Langerhans cell histiocytosis | -Langerhans cell histiocytosis | -Langerhans cell histiocytosis |
| -Langerhans cell sarcoma | -Langerhans cell sarcoma | -Langerhans cell sarcoma |
| Indeterminate dendritic cell tumor | Indeterminate dendritic cell histiocytosis | -Indeterminate dendritic cell tumor |
| Interdigitating dendritic cell sarcoma | Interdigitating dendritic cell sarcoma | -Interdigitating dendritic cell sarcoma |
| Not considered | Not considered | Histiocytic neoplasms |
| Disseminated juvenile xanthogranuloma | Disseminated juvenile xanthogranuloma | Juvenile xanthogranuloma |
| Erdheim-Chester disease | Erdheim-Chester disease | Erdheim-Chester disease |
| Not considered | Rosai-Dorfman-Destombes disease | Rosai-Dorfman disease |
| Not considered | ALK positive histiocytosis | ALK positive histiocytosis |
| Histiocytic sarcoma | Histiocytic sarcoma | Histiocytic sarcoma |
| Not considered | Not considered | Mesenchymal dendritic cell neoplasms (in stroma-derived neoplasms of lymphoid tissue) |
| Follicular dendritic cell sarcoma | Follicular dendritic cell sarcoma | Follicular dendritic cell sarcoma |
| -Inflammatory pseudotumor like follicular/fibroblastic dendritic cell sarcoma | EBV+ inflammatory follicular dendritic cell/fibroblastic reticular cell tumor | EBV+ inflammatory follicular dendritic cell sarcoma |
| Fibroblastic reticular cell tumor | Fibroblastic reticular cell sarcoma | Fibroblastic reticular cell tumor |
| Not considered | Not considered | Myofibroblastic tumour |
| Intranodal palisaded myofibroblastoma | ||
| Not considered | Not considered | Spleen-specific vascular-stromal tumours |
| Littoral cell angioma | ||
| Splenic hamartoma | ||
| Sclerosing angiomatoid nodular transformation (SANT) of spleen |
- Note: Bold Underline means "Category"; Bold Italics means "Family/Class" of diseases.
PRECURSOR T-CELL NEOPLASMS
Early T-cell precursor (ETP) ALL
T-lymphoblastic leukaemia/lymphoma (T-ALL) is derived from precursor T-cells. The subdivision in early T-cell precursor ALL (ETP-ALL) and T-ALL, according to WHO-HAEM4, remains substantially unchanged in ICC and WHO-HAEM5. There are only minimal semantic differences occurring between the two classifications, i.e. Early T-precursor lymphoblastic leukaemia/lymphoma in WHO-HAEM5 versus Early T cell-precursor lymphoblastic leukaemia/lymphoma NOS in ICC.6, 7 ETP-ALL shows a gene expression signature similar to that of the earlier stages of normal precursor T-cells. ETP-ALL is diagnosed by the immunophenotype that often includes the expression of stem cell and/or myeloid markers.
As compared to WHO-HAEM4,8 the ICC includes a subtype of ETP-ALL (about 30% of cases), which is characterized by the activation of BCL11B encoding a T-lineage transcription factor present in haematopoietic stem cells.9-11 Activation of BCL11B can occur both via interchromosomal rearrangements (80% of cases) or focal amplifications that generate a neo-enhancer distal to BCL11B9, 10 (20% of cases). FLT3-ITD and WT1 co-mutations are common. All cases share a common gene expression profile.
The subset of T-ALL cases showing a phenotype similar to ETP-ALL but expressing CD5 on ≥75% of blasts is referred to as ‘near-ETP-ALL’.8 Near-ETP-ALL differs from ETP-ALL both genetically (enrichment in rearrangements of TLX3) and clinically.12, 13
T-acute lymphoblastic leukaemia
According to the ICC, the remainder of T-ALL (T-ALL, NOS) are subclassified into eight new provisional entities based on various genetic alterations, including T-cell receptor rearrangements, chimeric fusion oncoproteins and enhancer mutations (Table 2).13-16 T-ALLs harbouring rearrangements of TAL1 or TAL2 (referred as ‘TAL1/2-r’) account for 30%–40% of cases, with TAL1-r being more common than TAL2-r cases. TAL1/2-r T-ALL are characterized by an intermediate prognosis. STIL::TAL1 is the most common fusion and shows a late cortical thymocyte immunophenotype (CD4+ or CD8+).17
| Subtype | Frequency | Partner genes/other rearrangements | Common colesionsa |
|---|---|---|---|
| BCL11B-activated | 30% of ETP and T/myeloid MPAL, <5% of AML | BETA (BCL11B Enhancer Tandem Amplification at 14q32, ~700 kb distal of BCL11B); ARID1B, CCDC26/ MYC; CDK6; STAB1; ETV6; ZEB2; RUNX1. | FLT3-ITD; WT1 |
| TAL1/2-R | 30%–40% (TAL2 rare); poor prognosis | TCRA/D; TCRB (TAL2); 1p32 deletion (STIL); intergenic SNV generating a TAL1-deregulating superenhancer | CDKN2A, NOTCH1, PTEN, USP7 |
| TLX1-R | 5%–10% children; near 30% adult; good prognosis | TCR | PHF6, BNM2, BCL11, RB1, CDKN1B |
| TLX3-R | 20%–25% children <5% adult; good prognosis | TCR; BCL11B; CDK6 | CDKN2A, NOTCH1, FBXW7, PTEN |
| HOXA | 15%–25% | HOXA::TCRB/TCRG; KMT2A – R; PICALM::MLLT10; SET::NUP214 | |
| LMO1/2-R |
LMO1-R 5% LMO2-R 10% |
TCR; cryptic deletion; enhancer/ promoter mutations LMO complex with bHLH factors; Extremely high LMO1/2 expression | CDKN2A, NOTCH1, FBXW7, PTEN, LEF1 |
| NKX2-R | <5% children | NKX2.1/NKX2.2/NKX2.5::TCR; BCL11B; CDK6 | CDKN2A, NOTCH1, PHF6, LEF1, RPL10 |
|
SP11-R BHLH, other |
<5%, children with, very poor prognosis <2% |
STMN1; TCF7; BCL11B TCRB::LYL1 TCR::BHLHB1; high LMO expression |
NRAS, KRAS |
- a NOTCH1 and CDKN2A mutations are common throughout T ALL, except ETP-ALL.
T-ALLs carrying TLX1- and TXL3 rearrangements occur in about 30% of adults and 20%–25% of children, show a CD4+/CD8+/CD1a+ thymic phenotype and are characterized by good prognosis18 (Table 2). The BCL11B::TLX3 rearrangement results into TLX3 deregulation and should not be confused with the BCL11B-activated group of ETP-ALL either phenotypically or molecularly.18 The ‘HOXA dysregulated’ subtype (15%–25% of cases) is molecularly heterogeneous, including the HOXA::TRB/TRG, KMT2A-r, PICALM::MLLT10 and SET::NUP214 rearrangements18 (Table 2). These cases show an immature immunophenotype, recalling that of ETP. T-ALLs carrying rearrangements of LMO1 or LMO2 (‘LMO1/2-r’) accounts for about 15% of cases, show an immature immunophenotype and express high level of LMO1/2 proteins.18 Although not formally recognized in the ICC, rare cases of BCR::ABL1-positive T-ALL may occur.
NK lymphoblastic leukaemia/lymphoma
According to the WHO-HAEM4, NK lymphoblastic leukaemia/lymphoma should be considered when tumour cells express CD56 along with immature T-associated antigens such as CD2, CD3 and CD7, in the absence of B-cell and myeloid markers. The condition, regarded as a provisional entity in the WHO-HAEM4, is retained as such in the ICC whereas it is deleted in the WHO-HAEM5 because of lack of clear-cut and reliable diagnostic criteria, the absence of information on the expression on NK-cell-associated antigens such as CD94 and CD161, and the morphologic/immunophenotypic overlap with other entities, especially blastic plasmacytoid dendritic cell neoplasm (Table 1).
MATURE T-CELL AND NK-CELL NEOPLASMS
Mature T-cell and NK-cell leukaemia
Chronic lymphoproliferative disorder of NK-cells (CLPD-NK) manifests as a persistent increase (≥2 × 109/L, for >6 months) of mature NK cells in peripheral blood with an indolent clinical course. It presents many similarities with T-large granular lymphocytic leukemia (LGLL) and is regarded as a provisional entity in the WHO-HAEM4 and ICC. The WHO-HAEM5 classification considers it a well-defined entity by renaming it as an NK-LGLL, in the light of recent evidence of monoclonal or oligoclonal expansion of NK cells.
EBV-related mature T-cell and NK-cell neoplasms
The EBV-positive T-cell and NK-cell lymphoproliferative disorders (LPDs) of children are rare diseases that may also affect adults and occur more frequently in Asia and Latin America. In the WHO-HAEM4, two major groups were recognized, namely, chronic active EBV (CAEBV) infection of T and NK-cell type with a cutaneous indolent form (hydroa vacciniforme-like LPD and severe mosquito bite allergy) and a systemic form, and systemic EBV+ T-cell lymphoma of childhood. The WHO-HAEM5 and ICC now recognize four major disorders: hydroa vacciniforme (HV) LPD, severe mosquito bite allergy, chronic active EBV disease (CAEBVD), and systemic EBV+ T-cell lymphoma of childhood. The terminology, criteria and morphological features of severe mosquito bite allergy and systemic EBV+ T-cell lymphoma of childhood are unchanged.
In the WHO-HAEM5 and ICC, HVLPD replaces the previous term of hydroa vacciniforme-like LPD since ‘classic’ HV in Western countries is also EBV-related and, therefore, belongs to the same disease spectrum as cases from Asia and Latin America.19, 20 Thus, the term HVLPD introduced by both classifications now encompasses all manifestations of EBV-associated skin lesions. Two clinical forms are recognized: (i) the classic form that is more common in whites, presents more frequently in spring and summer with localized papulo-vesicular eruptions on sun-exposed skin and no systemic symptoms,21, 22 and shows an indolent/self-limited course19, 22; (ii) the systemic form that is more common in Asians23 and Latin Americans21, 24 and is characterized by an aggressive and protracted course with skin lesion in sun-exposed and non-exposed areas, fever, lymphadenopathy and frequent liver involvement21, 25 that may require treatment.26 The neoplastic cells are small to medium-sized with atypia, perivascular and periadnexal distribution in the dermis and occasionally in the subcutaneous; angiodestruction and necrosis are often present.27 Many cases are CD8+ and express a cytotoxic T cell phenotype (positivity for TIA-1, granzyme B and perforin). Occasional cases have an NK-cell phenotype and tend to be more panniculitic, mimicking subcutaneous panniculitis-like T-cell lymphoma. EBER is positive in a variable proportion of infiltrating cells whilst LMP1 is usually negative. EBV DNA in the blood is very elevated but the levels are not discriminatory between the two forms. Most cases have clonal TCR gene rearrangements.
CAEBV, previously referred to as an infection, is now termed ‘CAEBV disease’ (CAEBVD) because most adults are chronically infected with EBV (for 3 or more months) in the absence of known immunodeficiency. CAEBVD is characterized by a large clinical spectrum ranging from localized and/or indolent forms including severe mosquito bite allergy and HVLPD in the classical form, to systemic disease with fever, haepatosplenomegaly and lymphadenopathy with or without cutaneous manifestations (HVLPD systemic form and systemic CAEBVD). High blood levels of EBV DNA and organs infiltration by EBV-infected T-lymphocytes or NK-cells23, 28, 29 carrying DDX3X and KMT2D mutations similar to those found in T-cell and NK-cell lymphomas, suggest that this is a premalignant condition. EBV genome intragenic deletions that are not detected in reactive conditions (e.g., infectious mononucleosis), may also play a role in the pathogenesis of the disease.30
“Primary EBV-positive nodal T cell or NK-cell lymphoma”31 that was initially introduced in the 2017 WHO classification as a variant of PTCL, NOS,1 is now considered a provisional entity in the ICC, while is recognized as a distinct entity in the WHO-HAEM5, under the term of nodal EBV-positive T-cell and NK-cell lymphoma. This tumour mainly occurs in Asian patients, usually elderly and/or immunodeficient, and is characterized by lymphadenopathy with rare extranodal involvement but without nasal localization. It has a poor outcome, more common large cytotoxic T-cell rather than NK-cell derivation,32, 33 common TET2 gene mutation, distinct molecular signature,34 and immune pathway upregulation as well as lower genomic instability.35
Extranodal NK/T cell lymphoma,36 qualified as ‘nasal type’ in the WHO-HAEM4 and ICC is renamed extranodal NK/T cell lymphoma (ENKTL) in WHO-HAEM5 due to frequent localization in other extranodal sites at presentation. Intravascular NK/T-cell lymphoma considered a form of ENKTL in WHO-HAEM4, is now placed under aggressive NK-cell leukaemia in the WHO-HAEM5 as a provisional entity.
Extranodal T-cell and NK-cell neoplasms of the gastrointestinal tract
The WHO-HAEM4 subdivision of primary intestinal T-cell lymphomas into two major entities, that is, enteropathy-associated T-cell lymphoma (EATL), which are usually preceded by refractory coeliac disease, and monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL),8 remains unchanged in ICC and WHO-HAEM5. Type II refractory coeliac disease (RCD-II) is a precursor of EATL and has therefore been added to the ICC classification.
RCD-II occurs in about 1% of patients with coeliac disease and is defined by the presence of persistent gastrointestinal symptoms, usually chronic diarrhoea and hypoalbuminemia that may lead to malnutrition, and villous atrophy, despite a strict gluten-free diet for at least 6–12 months, once other conditions have been excluded.36 Infiltration by small T-lymphocytes in RCD-II is not restricted to the intestinal epithelium but may extend to the lamina propria.36 Abnormal intraepithelial lesions (IELs) in RCD-II are CD3+ (cytoplasmic), CD2+, CD5−, CD7+, CD8−/+, CD30−, CD56−, CD103+, and positive for cytotoxic molecules (TIA1+/− granzyme or perforin) and rarely for the NK receptor NKp46.37 The abnormal IELs in RCD-II exhibit clonal TRG or TRB gene rearrangements. Trisomy of 1q is the only known recurrent chromosome abnormality.38 Frequent gain-of-function mutations in JAK-STAT pathway genes have been identified.37 RCD-II has a high risk of progression to EATL that should be suspected when large lymphoid atypical cells expressing CD30 are present.36
The distinction between EATL and MEITL has been further refined by means of genomic studies39 (Table 3). In particular, the T-cell receptor (TCR) is silent in most EATL patients whilst it is expressed in the majority of MEITL cases that derive more frequently from gamma-delta T-cells than from alpha-beta T-cells.40-44 Moreover, MEITL carries frequent recurrent alterations in SETD2, which encodes a lysine methyltransferase (resulting in defective trimethylation of H3K36)43-45 and often harbours mutations of the STAT5B, JAK3, TP53 and GNAI2 genes.43, 44, 46, 47 Conversely, the mutational landscape of EATL overlaps that of RCD-II, being characterized by highly recurrent activating mutations in the JAK/STAT pathway, most commonly in JAK1 (at the p.c1097 hotspot) and STAT3, and rarely in JAK3, STAT5B, TYK2 or SOCS1.37, 44, 45, 48
| Feature | EATL | MEITL |
|---|---|---|
| Ethnicity (excess incidence) | Northern European | Asian, Hispanic |
| Risk factors | Coeliac disease, HLA-DQ2/DQ8 | None recognized |
| Localization | Small intestine | Small intestine |
| Morphology | Polymorphic, inflammatory background absent, necrosis rare | Monomorphic, inflammatory background frequent, necrosis common |
| Usual immunophenotype | CD3+, CD5−, CD4−, CD8−, CD56−, CD103+, CD30+/−, cytotoxic+, MATK- | CD3+, CD5−, CD4−, CD8+, CD56+, CD103+/−, CD30−, cytotoxic+, MATK+ |
| T-cell receptor expression | Usually absent | Frequent, usually gamma delta |
| Mutations | STAT3, JAK1 | STAT5B, JAK3, TP53, GNAI2 |
The term intestinal T-cell lymphoma, NOS is used for EBV-negative T-cell lymphomas arising in the intestine that do not meet the diagnostic criteria for EATL, MEITL and other peripheral T cell lymphoma (PTCL) entities, especially adult T-cell lymphoma/leukaemia.
Two groups of indolent LPDs with a limited propensity to infiltrate the gastrointestinal tract are recognized (Table 1): (i) the indolent clonal T-cell LPD of the gastrointestinal tract according to the ICC that has been renamed ‘indolent T-cell lymphoma of the gastrointestinal (GI) tract’ in the WHO-HAEM5. The WHO-HAEM5 justifies the change in terminology from ‘lymphoproliferative disorder’ to ‘lymphoma’ according to tumour morbidity and the capability of the disease to spread, while the term ‘indolent’ is kept to indicate the protracted clinical course of the pathological condition7, 49-51; and (ii) the indolent NK-cell LPD of the gastrointestinal tract (iNKLPD), a new entity that has been added in both the ICC and the WHO-HAEM552 (previously referred to as NK-cell enteropathy53 or lymphomatoid gastropathy54). Both entities are EBV-negative.
The indolent clonal T-cell LPD/lymphoma of the gastrointestinal tract is characterized by the variable expression CD4 and/or CD851, 55 and by the curious correlation of T-cell subsets with genomic alterations. In fact, cases with the CD4+, CD4+/CD8+ and CD4−/CD8− phenotype usually carry mutations in the JAK-STAT pathway genes and in epigenetic modifier genes (e.g., TET2 and KMT2D) respectively, although the CD4+ cases sometimes harbour STAT3::JAK2 fusions.56 Some CD8+ cases were found to carry alterations of the IL2 gene.51
The iNKLPD of the gastrointestinal tract, formerly thought to be a reactive condition was recently unravelled to be a neoplastic process carrying mutations of various genes, including JAK3.57 This concept is further supported by the immunophenotypic findings showing activation of the JAK3-STAT5 pathway.57 Despite its neoplastic nature, this entity is characterized by an excellent outcome with frequent spontaneous regressions, although lesions may persist or new lesions may develop over a period of years, justifying its designation as ‘lymphoproliferative disorder’.53, 54 Rarely, this tumour has been reported to involve gallbladder, adjacent lymph nodes and the vagina52, 58, 59 but is consistently EBV negative, helping in its differential diagnosis with extranodal NK/T-cell lymphoma which is usually EBV-associated.
Peripheral T-cell lymphoma, NOS
In both the ICC and the WHO-HAEM5, PTCL, NOS remains a heterogeneous category and a diagnosis of exclusion. Based on the transcriptional program, two major biological variants of PTCL, NOS are recognized60: (i) the PTCL-TBX21 subgroup that resembles T helper type 2 (Th2) cells and is characterized by better prognosis and more frequent mutations in genes that regulate DNA methylation and (ii) the PTCL-GATA3 subgroup that derives from Th1 cells and is associated with a worse outcome and greater genomic complexity.60 These subgroups can be recognized by immunostaining for TBX21, CXCR3, GATA3 and CCR4 or by gene expression profiling.61-64 Moreover, the expression of cytotoxic molecules identifies a subset of aggressive PTCLs, NOS, usually occurring in patients with impaired immunity.60, 65 Although gene expression studies have improved our knowledge of PTCL, there are not yet enough data to justify that these molecular variants represent entities, and other studies are warranted before they are incorporated into routine clinical practice.
Follicular helper T-cell lymphoma
T follicular helper (TFH) cells expressing the typical markers (CD10, BCL6, CXCL13, CCR5, PD1 and ICOS)66, 67 represent the normal cell counterpart of the neoplastic cells of angioimmunoblastic T-cell lymphoma (AITL).68, 69 It has also been found that a subset of nodal PTCLs (not diagnostic of AITL) express the immunophenotypic and gene expression features of normal TFH cells.66, 68, 70-74 Therefore, the WHO-HAEM48 created an umbrella category of ‘nodal lymphomas of TFH cells origin (nTFHL)’ (Figure 1) grouping three entities, i.e., AITL, follicular helper T-cell lymphoma and nodal PTCL with TFH phenotype showing a diffuse or T-zone pattern without follicular dendritic cell (FDC) expansion. This categorization was supported by molecular studies showing a common genetic pattern,66, 75 such as mutations of TET2 (about 80%)76-78 and/or DNMT3A (30%–40%) of cases77 and the evidence that AITL frequently develops in the context of a clonal haematopoiesis.79 Other recurrent genetic mutations involving RHOAG17V (about 60% of cases), genes involved in TCR signalling,66, 80 and IDH2R172 appear to define a unique subgroup of patients with AITL,81 including cases with large clear-cell morphology.67 Finally, several pathogenic fusions involving the CD28, ICOS and VAV1 genes were discovered.18 More recent studies have shown that TFH lymphoma angioimmunoblastic-type is characterized by a stepwise acquisition of TET2 and DNMT3A mutations occurring early in haematopoietic stem cells (clonal haematopoiesis), while RHOA and IDH2 mutations are detectable in the neoplastic TFH cell population.82 Search for RHOAG17V or IDH2R172 mutations is recommended, especially in AITL in the early phase of the disease, when neoplastic cells can represent a minority of the examined population.82, 83 Conversely, the mutation profiles of nTFHL-F and nTFHL-NOS are less defined.66, 84, 85 Notably, PTCL with TFH phenotype have been reported to respond better to histone deacetylase inhibitors than other PTCLs.86-88

Because of the similar clinical and immunophenotypic features, as well as TFH gene expression signature and mutation profiles, the ICC unifies systemic lymphomas of TFH origin as a single entity – follicular helper T-cell lymphoma (TFH lymphoma) that comprises three subtypes: angioimmunoblastic-type (AITL), follicular-type and NOS. By definition, primary cutaneous small or medium CD4+ T-cell LPDs or other specified subtypes of cutaneous lymphomas with a TFH phenotype are excluded from this category. Similarly, a common family terminology of nodal lymphomas TFH is adopted in the WHO-HAEM5, renamed nodal TFH lymphoma (nTFHL) including angioimmunoblastic-type (nTFHL-AI), follicular-type (nTFHL-F) and not otherwise specified (nTFHL-NOS). In spite of semantic differences, the criteria for distinguishing the three TFH lymphoma subtypes are unchanged and are mainly based on morphology, immunoarchitecture, expression of TFH markers, hyperplasia of high endothelial venules, and FDC expansion. In the ICC, a panel of five-marker (CD10, BCL6, CXCL13, PD1 and ICOS) is recommended for establishing the TFH phenotype,75 while in the WHO-HAEM5 two of these markers plus CD4 defines such phenotypic profile. The five markers recommended by the ICC are not specifically quoted but plausibly correspond to those most widely used. Conversely, the WHO-HAEM5 underlines that further studies are required to determine if the positivity for two TFH markers plus CD4 is robust enough in differentiating nTFHL-NOS from PTCL, NOS, as most cases of the former often express the less specific markers such as PD1 and ICOS.
Haepatosplenic T-cell lymphoma
The entity remains unchanged in the WHO-HAEM5 and ICC. Although this tumour is more common in adolescents and young adults, it may also occur in older people.89 Next-generation sequencing revealed frequent loss of function mutations of the SETD2 tumour suppressor gene (25%).90 Other commonly mutated genes involved in epigenetic regulation were INO80 (21%), TET3 (15%), and SMARCA2 (10%).90 Finally, mutations leading to the activation of the JAK/STAT and PI3K pathways have been reported in haepatosplenic T-cell lymphoma.91 Patients are frequently chemoresistant but can benefit from allogeneic stem cell transplantation.91, 92
Anaplastic large cell lymphoma (ALCL)
The WHO-HAEM4 category of ALK-negative ALCL (ALK− ALCL) is molecularly heterogeneous93 and its diagnostic criteria remain unchanged in the ICC and the WHO-HAEM5. This entity does not include primary cutaneous ALCL (characterized by highly favourable outcomes) and breast implant-associated ALCL. By definition, ALK- ALCL resembles morphologically to ALK+ ALCL (with the exception of small-cell and lymphohistiocytic variants) and shows strong uniform CD30 expression and negativity for ALK, often associated with defective expression of T-lineage markers. Rearrangement of DUSP22 is detectable by FISH in 19%–30% of ALK− ALCL and defines a genetic subtype94-97 that is often associated with 'doughnut cell’.94 Expression of the Lymphoid Enhancing Factor (LEF1) has been proposed as a surrogate marker for this molecular alteration.98 In the ICC, DUSP22 rearranged cases are recognized as genetic subtype of ALK− ALCL (although not a formal separate entity). While earlier data had shown a favourable prognosis of ALCL with DUSP22 rearrangement which was comparable to ALK+ ALCL,99 more recent data had made the issue more controversial.96, 100
Patients carrying concomitant TP63 and DUSP22 rearrangements have been reported.101 Interestingly, cases with aberrant ERBB4 protein expression exhibit a Hodgkin-like morphology,102 as do cases carrying JAK2 rearrangement, which is, however, richer in anaplastic large cells.103 ALK− ALCL with TP63 rearrangements,99 STAT3 and TP53 mutations104 and/or overexpression of IL-2Rα105 show a poor outcome.
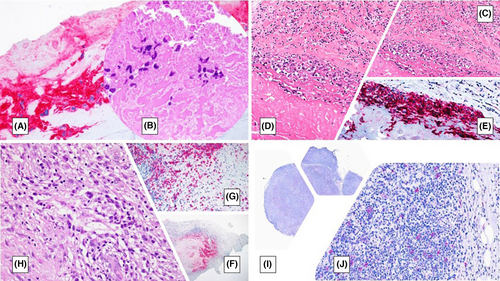
The breast implant-associated ALCL (BIA-ALCL), a provisional entity in WHO-HAEM4,8 has been upgraded to a distinct entity106-108 in both ICC and WHO-HAEM5 (Figure 2). This is usually a non-invasive tumour with good prognosis, arising in association with textured-surface breast implants.109 Deletions on chromosome 20q13.13 have been identified in about two-thirds of cases.110 Staging is critical to assess the prognosis and the need for chemotherapy. The presence of a mass lesion, capsular invasion and lymph node involvement are adverse prognostic factors.111, 112 Capsulectomy sampling and margin evaluation are important. The following TNM staging criteria are recommended: T1: in situ, tumour cells in seroma and/or on capsular luminal surface; T2: early capsule infiltration; T3: aggregates or sheets infiltrating capsule; and T4: the infiltration beyond capsule.111 Recently, a hypoxia signature,113 immune-evasion through amplification of 9p24.1, the overexpression of PD-L1, the constitutive activation of JAK-STAT pathway by somatic mutations of STAT3, STAT5B, JAK1 and JAK2,114-117 and the loss-of-function mutations of SOCS1 and SOCS3118 have been implicated in the pathogenesis of >50% of cases.
Primary cutaneous T-cell lymphoma
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL) is a cytotoxic T-cell lymphoma that occurs predominantly in younger patients, infiltrates the subcutaneous tissue and frequently associates with haemophagocytic lymphohistiocytosis,8 a life-threatening immune activation that adversely affects survival. There have not been changes in this entity, among ICC and WHO classifications. However, new interesting molecular data have recently been reported on SPTCL. In particular, many patients with SPTCL carry germline mutations in the HAVCR2 gene119-121 that encodes the T-cell immunoglobulin mucin 3 (TIM-3), predisposing to SPTCL. Biallelic missense mutations of HAVCR2 alter highly conserved residues in the extracellular immunoglobulin variable-like domain of the protein, leading to misfolding and to abrogate plasma membrane expression of TIM-3, a modulator of immune responses expressed on subsets of T and innate immune cells. These events then result in continuous immune activation and enhanced production of inflammatory cytokines (e.g., interleukin-1β and tumour necrosis factor-α), which lead to SPTCL and haemophagocytic lymphohistiocytosis. As compared to SPTCL patients with HAVCR2 wild-type, those carrying the very common HAVCR2-Y82C mutation were younger, carried UNC13D, PIAS3 and KMT2D mutations, were enriched in genes regulating IL6-JAK-STAT3 signalling and tumour necrosis factor-α signalling via NF-κB, developed more frequently haemophagocytic lymphohistiocytosis, and had shorter relapse-free survival.
The variants of mycosis fungoides (MF) are considered subtypes in the WHO-HAEM5 and the folliculotropic MF should be distinguished as either mild (early stage) or exuberant (advanced stage).122 The Sézary syndrome, although related to MF, in the WHO-HAEM5 is classified in mature T-cell and NK-cell leukaemia to highlight its clinical presentation. The mutational signatures reveal an important role of UV in its pathogenesis.123 There are no changes in MF/Sezary syndrome in the ICC. Distinctive genetic and epigenetic features of these cutaneous T-cell lymphomas have been recently reviewed, including the very frequent aberrant signalling of the JAK-STAT pathway.124
Primary cutaneous peripheral T-cell lymphomas, rare subtypes of the WHO-HAEM4 classification, included the following four provisional entities8: (i) Primary cutaneous gamma delta T-cell lymphoma; (ii) Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma; (iii) Primary cutaneous acral CD8+ T-cell lymphoma and (iv) Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder. Classification and diagnostic criteria of these entities, which are currently regarded as distinct, remained the same in ICC and WHO-HAEM5, with one exception. In particular, primary cutaneous acral CD8+ T-cell lymphoma of WHO-HAEM4, a tumour clinically characterized by preferential involvement of acral sites (e.g. ears), has been reclassified in both WHO-HAEM5 and ICC as primary cutaneous acral CD8+ T-cell lymphoproliferative disorder, mainly because of its indolent course and excellent outcome.125-128 This entity is distinguishable from other CD8+ cutaneous T-cell lymphomas because of the dot-like positivity of neoplastic cells for CD68.129, 130
Unlike ICC, the WHO-HAEM5 classification considers as a new entity the primary cutaneous peripheral T-cell lymphoma, not otherwise specified (pcPTCL-NOS); a poorly characterized group of T-cell lymphomas, which does not meet the criteria of any specifically defined primary cutaneous T-cell lymphoma entity. This is a diagnosis of exclusion.
Primary cutaneous CD30-positive T-cell lymphoproliferative disorders of the WHO-HAEM4 classification included the following two entities8: (i) Lymphomatoid papulosis; and (ii) Primary cutaneous ALCL. Classification and diagnostic criteria of these entities remain the same in the ICC and the WHO-HAEM5. Primary cutaneous ALCL characteristically lacks the genetic alterations found in systemic CD30+ ALCL but carries rearrangements of the IRF4/DUSP22 locus in about 20% of cases, mutations involving the IL6-JAK1-STAT3 pathway in 15%–30% of cases,131 and very rarely TP63132 or ALK rearrangements.133 Primary cutaneous ALCL with TP63 rearrangements exhibit an aggressive clinical behaviour similar to that of systemic ALCL with TP63 rearrangements.132 Moreover, whole-transcriptome sequencing has revealed the NPM1-TYK2 gene fusion in about 5% of primary cutaneous ALCL134, 135; these cases usually show nuclear STAT5 expression. Other genetic and epigenetic abnormalities in primary cutaneous ALCL are reviewed elsewhere.131, 135
The rare cases of ALK+ primary cutaneous ALCL show a favourable outcome.133 These cases should be staged accurately because skin lesions triggered by insect bites can be the first manifestation of systemic ALK+ ALCL.136 Insect bite-associated antigens have been hypothesized to attract to the skin lymphocytes carrying ALK translocations and to cause secondary release of different cytokines at the site of the bite, leading to activation and deregulated growth.136
TUMOUR-LIKE LESIONS WITH T-CELL PREDOMINANCE
This category included for the first time in the WHO-HAEM57 is not specifically quoted in WHO-HAEM41 and ICC.2 It comprises three entities: (i) indolent T-lymphoblastic proliferation (ITLP); (ii) Kikuchi-Fujimoto disease (KFD); and (iii) autoimmune lymphoproliferative syndrome (ALPS). In the WHO-HAEM4,1 ITLP – described with the same characteristics as in the WHO-HAEM57 – was discussed at the end of the chapter on T-lymphoblastic leukaemia/lymphoma, while ALPS was included among lymphoproliferative disorders associated with primary immune disorders by highlighting the same changes in genes involved in FAS-mediated apoptosis as well as morphologic and phenotypic abnormalities, as in the WHO-HAEM5.7
KFD137 is characterized by the co-expression of CD68 and myeloperoxidase by the macrophagic component in the absence of granulocytic infiltrate.138 The phenotypic profile of macrophages together with the presence of normal plasmacytoid dendritic cells, although not specific of KFD, may help in the microscopic differential diagnosis from PTCL.139 Clinically, KFD is characterized by auto-resolution usually without any therapy.137 Occasional recurrences have been reported, usually undergoing spontaneous regression.137
HISTIOCYTIC AND DENDRITIC CELL NEOPLASMS (HDCNs)
In the WHO-HAEM5, the chapter on HDCNs has been significantly modified by comparison with the WHO-HEAM4. Histiocytic sarcoma (HS), Langerhans cell histiocytosis/sarcoma (LCH/S), indeterminate dendritic cell tumour (IDCT), interdigitating dendritic cell sarcoma (IDCS), juvenile xanthogranuloma (JXG) and Erdheim-Chester disease (ECD) have been classified under myeloid neoplasms in recognition of their derivation from common myeloid progenitors, giving rise to monocytic/histiocytic/dendritic cell lineages.3 Key changes in the WHO-HAEM5 include: (i) inclusion of plasmacytoid dendritic cell neoplasms (pDCN) diseases in this category; (ii) moving follicular dendritic cell sarcoma (FDCS), fibroblastic reticular cell tumour (FRCT), and EBV+ inflammatory FDCS to a separate category termed ‘stroma-derived neoplasms of lymphoid tissues’ (discussed in the lymphoid Classification7); and (iii) addition of Rosai–Dorfman–Destombes disease (RDDD) and ALK+ histiocytosis as disease types. The rationale for such a framework is that HS, LCH/S, JXG, ECD and RDDD are characterized by mutually exclusive mutations of genes involved in the MAPK (BRAF, ARAF, NRAS, KRAS, and MAPK1/2) or PI3K (PIK3CA) pathways which may respond to treatment with BRAF and MEK inhibitors. ALK-positive histiocytosis shows a broad clinicopathologic spectrum unified by the presence of ALK translocation and response to ALK inhibitor therapy.
In the ICC, HS, LCH/S, IDCT, IDCS, disseminated JXG, ECD, FDCS, FRCT and EBV+ inflammatory FDC/fibroblastic tumour are included in a unique chapter (as in the WHO-HAEM4), with the adjunct of RDDD and ALK+ histiocytosis, regarded as new distinct entities. Moreover, they are discussed in the context of the lymphoma classification.2 The rationale for this organization is that all these conditions – similar to peripheral B-cell and T-cell lymphomas – stem from terminally differentiated cells, belonging to either the myelomonocytic or mesenchymal axis. Thus, BPDCN was not included in the ICC chapter on HDCNs, as it derives from a precursor of mature pDCs. None of the mutations of the myeloid family of HDCNs in WHO-HAEM5 is per se specific, since they can occur in many tumours of different histogenesis. For instance, FDCS can carry BRAF V600E mutations although it recognizes a mesenchymal derivation. For the authors of the ICC, the argument of the detection of similar mutations (e.g., BRAF) in neoplastic cells and haematopoietic precursors does not represent absolute proof for the reclassification of histiocytic tumours. They claim that, for example, the t (14;18) translocation, characteristic of follicular lymphoma, can also be detected in bone marrow precursors and circulating B lymphocytes favoring the development of FL, which nevertheless remains a peripheral B-cell neoplasm.
In the following, a brief description of ALK+ histiocytosis and RDDD will be reported, as both conditions have found an autonomous recognition in ICC and WHO-HAEM5.
ALK+ histiocytosis
The first three patients with systemic ALK+ histiocytosis were reported in 2008,140 and presented in early infancy with pallor, massive hepatosplenomegaly, anaemia and thrombocytopenia. About 40% of cases may present with localized disease involving nasal skin, foot, breast and intracranial cavernous sinus.141 The condition is characterized by large histiocytes, which do not show atypical features and morphologically and resemble those observed in disseminated JXG and at times in RDDD (large oval, foamy or spindle cells, some with multinucleation, including Touton giant cells, or emperipolesis). They strongly express CD68, CD163 and lysozyme, while they are negative for CD1a, CD207 and mutated BRAF. Immunostaining for the ALK protein is pathognomonic of the neoplastic nature of the condition. Thus, ALK immunostaining should be possibly performed in all cases of histiocytosis. Molecular studies revealed the KIF5B-ALK or COL1A2-ALK gene fusion in five or six cases investigated.141 In another study, one case carrying TPM3-ALK was identified. These cases are classified as ALK-positive histiocytosis in both the ICC and the WHO-HAEM5. Because rearrangements of ALK lead to the activation of signalling pathways,2, 3 chemoresistant cases are suitable for treatment with ALK inhibitors.141, 142
Rosai–Dorfman–Destombes disease (RDDD)
RDDD represents a disease entity in both the WHO-HAEM5 and the ICC. It is a rare histiocyte-derived disorder occurring mainly in children and young adults, frequently African and male. It most commonly presents with massive bilateral painless cervical lymphadenopathy that may be associated with B-symptoms. Extranodal involvement is observed in about 40% of cases but rarely without lymph-node involvement, with the exception of skin. Sites of disease are infiltrated by pale histiocytes with large, nucleolated, hypochromatic nuclei, positive for histiocytic markers (S100/fascin/CD68/CD163). Emperipolesis is characteristically present. Mutations of MAPK pathway genes (NRAS, KRAS, MAP2K1, and, rarely, BRAF) are observed in 20%–30% of cases and point to the neoplastic nature of RDDD.143-147 RDDD is often a self-limited disease associated with spontaneous regression, although a subset of patients may behave aggressively and require systemic therapies. Patients with organ- or life-threatening diseases might benefit from MEK inhibitors.143, 145
CONCLUSIONS
The contemporary proposal of two different classifications of haematolymphoid tumours prompted us to write the present review on T-cell lymphomas and histiocytic and dendritic tumours, with the following aims: (i) to assist pathologists and clinicians in their daily work that implies problem-solving and decision-making; (ii) to highlight areas of convergence and disagreement between the two schemes as a contribution to their future reconciliation. The fact that several parts of WHO-HAEM5 and ICC do not significantly diverge, should encourage the Bodies and Authorities interested in the classification management to sit around the same table and find a common path in the interests of the community.
AUTHOR CONTRIBUTIONS
Brunangelo Falini had the original idea and wrote the manuscript. Stefano Lazzi and Stefano Pileri gave their contribution to writing the manuscript.
ACKNOWLEDGEMENTS
This work was supported by the Associazione Umbra contro le Leucemie e Linfomi (AULL) and AIRC 5x1000 grant 21118.
CONFLICT OF INTEREST STATEMENT
BF and SP are co-signatory to the ICC classification of lymphoid neoplasms. SL is co-signatory to the 5th WHO classification of lymphoid neoplasms.