Outpatient transperineal prostate biopsy under local anaesthesia is safe, well tolerated and feasible
The corresponding author did not receive a research scholarship.
Abstract
Background
Transperineal biopsy (TPB) of the prostate has been increasingly utilized as it has reduced infection risks. Traditionally however, it is performed under general anaesthesia, thus it carries a differing set of risks. Recently, new studies have performed TPB under local anaesthesia with success. In the present study, we explored our experience of performing TPB under local anaesthesia in an Australian cohort.
Methods
In this prospective study based at a metropolitan outpatient clinic, patients were provided with TPB under local anaesthesia. We assessed prostate cancer detection rates, complication rates and patient tolerability. Pain tolerability was assess using patient reported pain score on the visual analogue scale. Follow up data was collected at days 7 and 30 post-biopsy via telephone interview.
Results
A total of 48 patients were enrolled in this study between June 2020 and March 2021. Median age was 65.5 years and median PSA was 6.95 ng/mL. Clinically significant prostate cancer was detected in 58% of patients. During the procedure, pain scores were rated the highest during infiltration of local anaesthetic agent with a median score of 5. By the conclusion of the procedure, median pain score was 1. Vast majority of patients (85.4%) would opt for a repeat TPB under local anaesthesia should the need for prostate biopsy arise again. Two of our patients experienced infectious complications, and one experienced urinary retention.
Conclusion
Our data is in line with currently available data and confirms that TPB under local anaesthesia can be achieved in a safe and tolerable manner.
Introduction
Prostate cancer is a common malignancy in men worldwide with the second highest incidence and mortality rate.1 Hence, timely diagnosis and treatment is vital. Detection of prostate cancer starts with PSA screening, MRI imaging followed by biopsy. Several biopsy techniques are available to the urologist. Transperineal biopsies (TPB) have grown in utility over the transrectal route due to lower infection risks,2 as well as the ability to sample the anterior portion of the prostate gland. Traditionally cited disadvantages of utilizing TPB include requirement for general anaesthesia and requirement for greater labour time.3 However, recently TPB under local anaesthesia (LA) have become increasingly used as this technique can be performed in the outpatient setting while retaining the advantages of the TPB technique.
A second challenge recently arisen from the COVID-19 pandemic is the redirection of hospital resources to combat this crisis. Where we can, we should consider use of outpatient facilities rather than the operating theatre and hospital beds. Moreover, concerns have been raised regarding the transmission risks of COVID-19 via the gastrointestinal tract, although this risk is not yet fully understood.4
In the present study, we explored our experience of performing TPB under local anaesthesia in an Australian cohort.
Methods
This is a prospective study involving patients from a single major metropolitan clinic. Approval was provided by the local ethics committee at Western Health Ethics (approval number: RES-19-0000757L-55398) and each patient was provided with written information prior to study recruitment. Patients who tolerated a DRE poorly were also provided with information and an opportunity to participate regardless. Informed consent was obtained prior to participation in the study. Consecutive patients without prior diagnosis of prostate cancer but with suspicions were selected for this study. All except one patient had a pre-biopsy mpMRI and offered a biopsy if a suspicious lesion was seen (PIRADS ≥3) or if PSA density was more than 0.15ng/ml.2 Patients excluded in this study were those on active surveillance, non-English speaking patients and patients who did not have adequate per rectal access (such as patients with rectal cancer or patients with anorectal malformations). Active surveillance patients were excluded as there is evidence some active surveillance patients experience significant levels of anxiety5 and this anxiety may exacerbate patients' experience of pain.6 This forms a confounder to pain assessment, thus active surveillance patients were excluded.
All procedures were performed by a senior urologist (HZ). Prior to conducting TPB under local anaesthesia for this study, the urologist performed 5 TP biopsies using the PrecisionPoint® system under a general anaesthetic to become acquainted, followed by another 5 biopsies in a theatre setting under local anaesthetic with the anaesthetist on standby in case conversion to general anaesthesia is necessary. No cases required conversion to general anaesthesia or sedation during the learning curve period. No formal learning curve analysis was performed. These 10 patients were excluded from our data analysis due to inability for patients under general anaesthesia to provide assessments of their pain levels during the procedure.
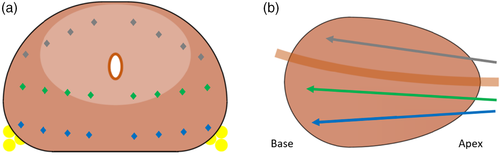
The step-by-step description of the technique has been previously published.7, 8 Patients were prepared in an outpatient procedural room with sterile set up. Patients did not undergo routine urine cultures and did not routinely receive antibiotics. Oral analgesia was also not routinely given. Procedures were performed on Transforma Gynae Couch, model 1261 (Dalcross Medical Equipment, NSW, Australia). Patients were positioned in low lithotomy position with the scrotum is held up by the patient's dominant hand under the sterile drapes. This task was given to the patient as a distraction technique during the procedure. Perineum is prepared with a betadine wash. Perineal skin at the site of intended needle entry infiltrated with 5 mL of 1% lignocaine solution with 1:200000 adrenaline. A biplanar transrectal ultrasound (TRUS) probe was used, mounted with a PrecisionPoint® Transperineal Access System (BXT-Accelyon, Slough, UK) to guide the biopsy needle. Once the TRUS probe was inserted, periprostatic nerve block was achieved by injecting 15 mL of 1% plain lignocaine followed by removal of the probe and 5 min allowance for block to take effect. Subsequently the ultrasound probe was reinserted, and needle guide placed in the perineum to sample ipsilateral prostate half. In majority of cases, the guide was repositioned for obtaining access to the contralateral half of the gland. The biopsies were performed in a free hand manner using a standard template for systematic biopsies according to Ginsburg Protocol9 (Fig. 1) and, where applicable, five cores of targeted samples were taken. At the conclusion of the procedure, patients were observed for at least 30 minutes and were required to void prior to leaving the outpatient clinic accompanied by their carer.
The primary endpoint included complications, pain scores and tolerability as rated by the patient. Secondary endpoints included detection of clinically significant prostate cancer (csPCa), lower urinary tract symptoms, erectile dysfunction and days of work missed. Data was collected prior to the biopsy (baseline), during the biopsy, at day seven post-biopsy and at day 30 post-biopsy. Clinical details collected include patients' demographic data, PSA, DRE stage, MRI results, pain scores, erectile function, lower urinary tract symptoms, post-operative complications and biopsy histopathology. Histopathology was graded according to the recommendations of the 2005 consensus conference of the International Society of Urological Pathology (ISUP).10 csPCa was defined as ISUP grade 2 or higher. Pain scores were specifically collected at baseline, at LA infiltration, TRUS probe insertion, first fire of the biopsy needle and post-procedurally. The visual analogue scale (VAS) with 0 representing no discomfort and 10 representing severe pain was used for patient-reported pain scores. Lower urinary tract symptoms were assessed using the International Prostate Symptom Score (IPSS). Erectile function was assessed using the erectile function subset of the international Index of Erectile Function (IIEF). Follow up data was collected via telephone calls at 7 days post procedure for IPSS and 30 days post procedure for IIEF. IIEF was collected at 30 days post procedure as there is evidence suggesting worsening erectile function at 1 month post biopsy,11 thus we assessed erectile dysfunction at day 30 to capture the maximal impact of this prostate biopsy technique. In patients who have had prior biopsies, data was also obtained comparing their TPB under local anaesthesia experience with prior biopsy, with patients asked to comment whether TPB under local anaesthesia was ‘better’, ‘comparable’ or ‘worse’.
Statistical analysis was performed using SPSS v. 26 (IBM Corp., Armonk, NY, USA). Statistical significance was determined by P-value <0.05. Continuous variables were expressed in median and interquartile ranges, with categorical variables are expressed as absolute numbers and percentages.
Results
A total of 48 patients were enrolled in this study between June 2020 and March 2021. Median age was 65 years old and median PSA was 6.95 ng/mL. All patients had undergone pre-biopsy prostate magnetic resonance imaging (MRI). MRI results were benign in 47.9% of patients, however these patients underwent a biopsy due to ongoing raised clinical suspicion. Median prostate size was 40 cc according to the MRI. Patient characteristics are summarized in Table 1.
| Patient characteristics | |||
|---|---|---|---|
| N | 48 | ||
| Age, years (IQR) | 65.50 (59–70) | ||
| PSA, ng/mL (IQR) | 6.95 (5.05–9.5) | ||
| DRE | Not recorded, n (%) | 41 (85.4%) | |
| Malignant, n (%) | 4 (8.3%) | ||
| Benign, n (%) | 3 (6.3%) | ||
| MRI lesions, n (%) | Benign, n (%) | 23 (47.9%) | |
| PI-RADS 3, n (%) | 3 (6.3%) | ||
| PI-RADS 4, n (%) | 7 (14.6%) | ||
| PI-RADS 5, n (%) | 14 (29.2%) | ||
| No MRI, n (%) | 1 (2.1%) | ||
| Prostate size, cc (IQR) | 40 (35.75–58.25) | ||
| IPSS, median (IQR) | Baseline, score (IQR) | 6 (3–10) | p = 0.012 |
| Day 7 post-biopsy, score (IQR) | 7 (5–11) | ||
| IIEF, median (IQR) | Baseline, score (IQR) | 10.5 (1–24) | p = 0.094 |
| Day 30 post-biopsy, score (IQR) | 2.5 (1–11) | ||
| Histopathology | |||
| Cores | 30 (24–36) | ||
| csPCa, n (%) | 28 (58.3%) | ||
| ISUP grade | Benign, n (%) | 13 (27.1%) | |
| ISUP 1, n (%) | 7 (14.6%) | ||
| ISUP 2, n (%) | 18 (37.5%) | ||
| ISUP 3, n (%) | 5 (10.4%) | ||
| ISUP 4, n (%) | 1 (2.1%) | ||
| ISUP 5, n (%) | 4 (8.3%) | ||
| Complications | |||
| Infections | 2 (4.2%) | ||
| Retention | 1 (2.1%) | ||
| Pain measured by VAS, score (IQR) | Baseline VAS score | 0 (0–2) | |
| VAS at LA infiltration | 5 (2–5.75) | ||
| VAS at US probe insertion | 3 (1–5) | ||
| VAS at first needle pass | 2 (1–4) | ||
| Day 0 post procedure | 1 (0–2.75) | ||
| Day 7 post procedure | 0 (0–0) | ||
| Day 30 post procedure | 0 (0–0) | ||
- Abbreviations: DRE: digital rectal exam; IQR: interquartile range; IPSS: International Prostate Symptom Score; IIEF: International Index of Erectile Function; csPCa: clinically significant prostate cancer; VAS: visual analogue scale.
While data on procedure duration was not formally recorded, typically the TPB procedure takes <30 min. Median number of cores assessed by the pathologist was 30. Histopathology analysis demonstrated csPCa in 28 (58.3%) patients. A further 7 (14.6%) patients were diagnosed with ISUP 1 disease, leading to an overall cancer detection rate of 72.9%. Out of the 25 patients with PIRADS 3–5 lesions found on MRI scans, targeted biopsies were performed with 18 (72.0%) demonstrating csPCa. Another 6 patients had ISUP 1 prostate cancer, leading to an overall cancer detection rate for targeted biopsies of 96.0% (Table 2).
| Biopsy results | PIRADS 3 (n = 3) | PIRADS 4 (n = 8) | PIRADS 5 (n = 14) |
|---|---|---|---|
| Benign | 1 | – | – |
| ISUP 1 | - | 4 | 2 |
| ISUP 2 | 2 | 2 | 7 |
| ISUP 3 | – | 2 | 1 |
| ISUP 4 | – | – | 1 |
| ISUP 5 | – | – | 3 |
Patient rated their pain response to the procedure at different steps. At baseline, 30 patients reported no pain with the median score on VAS being zero. Infiltration of LA elicited the highest pain score, with 98% of patients reporting pain and a median score of five. This was significantly different to baseline pain scores (p < 0.02). Median pain scores at TRUS probe insertion and first pass of biopsy needle three and two respectively. Both procedural steps were associated with a significant reduction in pain score compared to pain core of LA infiltration (p < 0.02). Immediately post procedure median pain score was one, with 45.8% of patients reporting no pain. At 7 and 30 day follow up time points, median pains scores were zero for both. Nine (18.8%) and three patients (6.2%) described any form of discomfort at the 7 and 30-day time points respectively,
Survey completion rates for IPSS at baseline and day 7 post-biopsy was 89.6%. Median IPSS score at baseline was 6 versus 7 at day seven post-biopsy (p = 0.012). Given there is very little difference between day 7 and baseline, no further IPSS data was collected. Survey completion rates for IIEF at baseline and day 30 post-biopsy was 85.4%. Erectile function score did not significantly differ between baseline and day 30 post-biopsy (median score 2.5 versus 10.5, respectively, p = 0.094).
There were two cases of infectious complications, both categorized as Clavien-Dindo class 2. One patient developed a urinary tract infection (UTI) requiring IV then oral antibiotics. The second patient developed systemic symptoms with a positive blood culture and was treated with IV antibiotics. There was also 1 case (2%) of urinary retention. No other complications were noted, specifically no patients described feeling light-headed, syncopal or suffered syncope.
In our cohort, eight patients had received prior prostate biopsies under GA, with six (75%) patients indicating that LATPB was ‘better’ than their prior biopsy. One patient rated LATPB as ‘comparable’ to the prior GA procedure and one patient rated LATPB as ‘worse’. Amongst 48 patients, 41 (85.4%) indicated that they would undergo another biopsy procedure under LA if further prostate biopsies are required. Days of work missed was recorded in 13 patients, with the remainder of patients describing a lack of employment. Of the 13 patients who did return to work, they did so after a median of 2 days.
Discussion
In our study, we assessed the feasibility, tolerability and safety of performing TPB under LA. We found that the detection rate of csPCa was 58.3% with TPB under LA. Indeed several recent studies have reported similar detection rates of 52% of csPCa.12-14 As our patients were not sedated, they maintained awareness throughout the procedure. Care needed to be taken to reduce their pain experience during the biopsy procedure. Our data shows the most painful stage of the procedure is when LA is infiltrated in all but one patient, with a median score of 5 on VAS. TRUS probe insertion and first passage of the biopsy needle was associated with a significant reduction in pain score, to three and two, respectively. This is logical, as one would expect the anaesthetic agent to be effective for the procedural steps following LA infiltration. No patient required additional analgesia or anaesthetic agent, nor was the procedure paused due to discomfort. Further adding evidence to good patient tolerability is the median pain scores post procedure of one, with 45% of patients describing no pain at all. Our study results in overall pain are favourable for TPB under LA. Several studies also evaluated pain, however using different measures, making it difficult to compare. Lopez et al. found that 64% of patients described the pain perception as either ‘not at all’ or ‘a little’ painful.12 Several studies reported median overall low pain score for the biopsy process,14, 15 but did not differentiate the step of the biopsy process. Gorin et al. showed most similar data, when patients experienced a significant increase in pain during the procedure, which returned to baseline upon conclusion of the TPB.16
Whilst pain is an important part of patient tolerability, there may be other factors important to a patient which we did not interview for. Thus, assessing patients' own perception of tolerability is important. In our study, the majority of patients (85.4%) considered their experience with TPB under LA tolerable and would choose to undergo the same technique again should future prostate biopsies be required. This is again in line with current literature reports. Smith et al. reports 96% of patients would have the procedure again,17 and Lopez et al. reported that 81% of patients describe the procedure as ‘tolerable’ under LA.12
We attempted to assess functional recovery using the days until return-to-work parameter. We found 13 (27.1%) patients to have returned to work after a median of 2 days post-procedure. The remainder of patients (72.9%) declared they did not have employment. While we did not formally collect data on reasons for lack of employment, 24 (50%) of our patient cohort had reached Australian retirement age. Our data collection also spans three periods of government imposed ‘lockdown’ restrictions during the COVID-19 pandemic, and this was thought to at least partially account for our results. While interpretation of our results may be limited due to the small population number, we think these results are noteworthy given there is currently no guideline on this matter.
Lower urinary tract symptomatology was assessed using the IPSS score. While there was a statistically significant change in IPSS score, the change was modest (6 at baseline versus 7 at day 7). Similarly, current literature suggests that almost 25% of patient experience worsening of lower urinary tract symptoms after prostate biopsy, although this tends to be a short-term complication.11 Our results also demonstrated no statistically significant reduction in erectile function. This is incongruent with current literature, where prostate biopsies, regardless of route, are believed to reduce erectile function.11, 18, 19 In studies with longer follow up durations, erectile function is seen to recover.11 Our results differ possibly due to our small sample size. Indeed we demonstrated several points reduction in erectile function scores at 30 days post-biopsy, albeit being statistically insignificant results.
A major concern of prostate biopsies is the potential to develop infectious complications after the procedure despite routine use of prophylactic antibiotic regimes. Infectious complications are not only burdensome for patients, but at a mean cost of AUD7362 per admission,20 it is also a costly experience. Rates of infection post TPB are much reduced compared to transrectal biopsies3, 21, 22 making them preferrable in this aspect. Indeed this very reason have led to calls for the transrectal biopsy technique to be abandoned worldwide.23
While prophylactic antibiotics are routinely used in several institutions, profuse use of fluoroquinolone worldwide has led to an increase in post-biopsy sepsis with resistant strains of Escherichia coli.24-26 In light of this, some clinicians have escalated to the use of carbapenems.27 Subsequent reports have suggested that fluoroquinolone, extended spectrum cephalosporins and carbapenem consumption has driven the emergence of carbapenem resistance pathogens.28-30 Interestingly, carbapenem-resistance can develop due to exposure to other antibiotics such as fluoroquinolones without carbapenem exposure, due to coresistance.29 Thus, while prolific use of antibiotics is a strategy for improving short term outcomes in infectious complications, clinicians contribute to a wider problem of multidrug resistant pathogens. To target this, recently some patients undergoing TPB have not been given prophylactic antibiotic altogether while maintaining low levels of infection related complications.13, 31 Given the improved infectious complication rates with TPB, and positive prior experience without prophylactic antibiotics, we adopted this approach for our biopsies. Indeed, there is recent systemic analysis suggesting that the rate of infectious complications post TPB with and without prophylactic antibiotics does not significantly differ.32
Reported rates of infectious complications post TPB are as low as 0%.3, 33 On the contrary, our infectious complications comprising of two out of 48 patients (4.2%), was remarkably high. However, we would argue that given our small cohort, the true significance of this is difficult to ascertain. For one patient, on repeated questioning at representation, he disclosed that he was experiencing symptoms suggesting he may have an UTI prior to the biopsy. Our routine protocol would exclude this patient from proceeding with TPB at that time should this have been flagged. This serves as a reminder that we should be diligent in our patient assessments and despite minimal infectious risks post-TPB it is still a possibility. Furthermore, one (2.1%) patient developed urinary retention. Finally, there were no reports of light-headedness, feeling syncopal, or syncopal events, and this could relate to the anaesthetic of choice being LA, rather than general anaesthesia.
A formal cost analysis was not performed as part of this study. However, a brief post hoc analysis of the outpatient TPB approach showed that savings are produced is in the use of theatre administration, anaesthetic services, theatre technician, recovery bedspace and additional nursing staff (theatre typically have two or more nursing staff, whereas outpatient TPB requires one nursing staff) amongst other domains. Latest available costs for these services for prostate biopsies were obtained from a major metropolitan hospital. The average costs of these domains per procedure was AUD1330.22. Comparatively, the PrecisionPoint® device costs AUD350. The biplanar ultrasound probe used is identical to that used in TPB under general anaesthesia and would not represent an additional cost. As such, TPB under general anaesthesia would cost at least AUD980.22 more than TPB under local anaesthesia. In our cohort alone, this reflected an estimated costs savings of AUD47,050.56. The second area of saving is patient time. Without general anaesthesia, 30 min of observation and voiding were what we required of our patients prior to departure from the clinic.
While our study is prospective in nature, it is limited by its small cohort. In addition, our results for days of work missed may not be representative as a large portion of patients was not holding employment at the time. Furthermore, we asked patients who previously had biopsies under general anaesthesia to compare using broad ‘better’, ‘comparable’, ‘worse’ ratings. This method subject to recall bias however it still serves as a useful measure of patient experience. This is a single centre, single operator series and thus may have biases limiting the ability to generalize our results. Finally, this study lacks a control group, making it difficult to draw definitive conclusions about superiority of this technique. These shortcomings notwithstanding, our study is the only Australasian series for outpatient TPB under local anaesthesia and supports the currently published literature.
Conclusion
TPB under LA in the outpatient setting is a safe and feasible practice. Our study adds to current literature supporting use of TPB under LA with high csPCa detection rates. It shows excellent patient tolerability while minimizing complications. Particularly during a time where hospital resources are redirected to manage the COVID-19 crisis, eliminating the need for operating theatre space and a hospital bed for the urology patient while still providing standard of care investigations is invaluable.
Conflict of interest
None declared.
Funding
The study was supported by an investigator-initiated grant provided by Mundipharma.
Acknowledgment
Open access publishing facilitated by The University of Melbourne, as part of the Wiley - The University of Melbourne agreement via the Council of Australian University Librarians.
Author contributions
Anne Hong: Data curation; formal analysis; writing – original draft; writing – review and editing. Sarah Hemmingway: Data curation; investigation; project administration. David Wetherell: Investigation; methodology; project administration; resources. Brendan Dias: Conceptualization; investigation; project administration; resources. Homayoun Zargar: Conceptualization; funding acquisition; investigation; methodology; project administration; resources; supervision; writing – review and editing.