Operative outcome of hernia repair with synthetic mesh in immunocompromised patients
L. D. Lee: MD; A. Stroux MSc; D. Nickisch MD; B. Weixler MD; M. E. Kreis MD; J. C. Lauscher MD.
Lucas D. Lee and Andrea Stroux contributed equally to this study.
Abstract
Background
The safety of synthetic mesh in elective hernia repair in the setting of immunosuppression lacks national and international consensus. The aim of our analysis was to explore the effects of immunosuppression on the rates of wound complications.
Methods
Comparative analysis of immunocompetent and immunocompromised patients with elective mesh repair of inguinal, femoral, primary ventral, incisional or parastomal hernia between January 2001 and December 2013. Immunosuppression included glucocorticoids, biologicals, chemotherapy and chemoradiotherapy. Primary outcome parameter was mesh infection rate. Follow-up questionnaires were completed in written form or by telephone interview.
Results
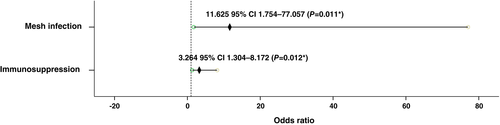
Questionnaire response rate was 59.5% (n = 194) with a median follow-up of 33 (interquartile range: 28–41) months. There were no differences between immunocompromised (n = 40, 20.6%) and immunocompetent patients (n = 154, 79.4%) based on hernia and patient characteristics. Immunosuppression was not associated with the rates of mesh infection (P = 1.000), surgical site infection (SSI, P = 0.330) or re-operation for SSI (P = 0.365), but with higher rates (P = 0.007) and larger odds for hernia recurrence (odds ratio 3.264, 95% confidence interval 1.304–8.172; P = 0.012). Mesh infection also increased the odds for hernia recurrence (odds ratio 11.625; 95% confidence interval 1.754–77.057; P = 0.011). Only in the subset of ventral/incisional hernias, immunocompromised (n = 8, 40%) patients had higher recurrence rates than immunocompetent patients (n = 5, 11.6%; P = 0.017). Patients with SSI reported more frequently moderate to severe dysesthesia at the surgical site (P = 0.013) and would less frequently re-consent to surgery (P = 0.006).
Conclusion
Immunosuppression does not increase the rate of wound infections after elective hernia repair with synthetic mesh. However, immunosuppression and mesh infection are risk factors for hernia recurrence.
Introduction
Hernia patients with immunosuppression represent a high-risk cohort for surgical complications, yet may still have the indication for elective hernia repair. However, current data about the value of synthetic mesh in an immunocompromising setting are limited. Adequate risk assessment for post-operative wound complications or hernia recurrence is currently not possible. Even the latest composite risk score model for surgical site infections (SSIs) after ventral hernia repair by Bernardi et al. does not consider immunosuppressive factors.1
Prior analyses of incisional ventral hernia repair suggested higher rates of 30-day SSI among immunocompromised patients.2 Affected patients often require interventional drainage, wound debridement and negative-pressure wound therapy in combination with long course antibiotic treatment. Indeed, immunosuppressive drugs such as steroids were identified as risk factors for the infection or explantation of synthetic meshes.3 Surgical mesh removal often implicates an array of serious health impairments (e.g. prolonged recovery, decrease in function, recurrence, pain) and social consequences (e.g. delayed return to daily and professional activity). Hence, should surgeons refrain from implanting synthetic mesh in immunocompromised hernia patients?
Inguinal hernia repair with synthetic mesh has been widely adopted as standard of care because of low recurrence rates.4, 5 Achievable 3-year recurrence rates have been reported as low as 24% compared to 43% for suture repairs.6 However, there exists no international consensus on the use of synthetic meshes in immunocompromised hernia patients.4, 5, 7
Thus, the aims of our study were to determine the rates of mesh infection, to identify risk factors for wound complications and hernia recurrence and to explore the long-term outcome among immunocompromised patients who underwent elective hernia repair with synthetic mesh.
Methods
Trial design and participants
The retrospective, comparative and single-centre protocol was approved by the ethics committee of the Charité – Medical University of Berlin (Application No. EA4/043/14). Patients (age ≥ 18 years) who underwent elective hernia repair with synthetic mesh were included. Those with emergent and/or suture repair or inability to answer the questionnaire were excluded. Types of hernia included (i) inguinal, femoral; (ii) primary ventral (epigastric, umbilical); and (iii) incisional, parastomal.
Immunosuppression included steroids, biologics, systemic chemotherapy or chemoradiotherapy for solid malignancy up to 6 months before surgery or for haematological malignancies up to 2 years before surgery. Immunosuppressive regimens were categorized into two subsets: (i) systemic chemotherapy/chemoradiotherapy (n = 10); and (ii) any combination of immunosuppressants (n = 30). The latter included agents such as prednisolone, infliximab, rituximab, adalimumab, ciclosporine and tacrolimus.
Hernia repair
Inguinal/femoral hernias were repaired either by open (Lichtenstein) or minimally invasive techniques, that is totally extraperitoneal (TEP) or transabdominal preperitoneal (TAPP). Pre-operatively, 2 g ampicillin/1 g sulbactam (Pfizer, Berlin, Germany) was given for Lichtenstein, but not for minimally invasive repair. Partially absorbable lightweight polypropylene-polyglecaprone mesh (ULTRAPRO, Ethicon, Norderstedt, Germany) was cropped to 15 × 12 cm for augmentation.
Same antibiotic was pre-operatively given for ventral, incisional and parastomal hernia repairs. Between 2001 and 2012, we implanted lightweight polypropylene-polyglactin mesh (Vypro, Ethicon, Norderstedt, Germany) during open repair. Afterwards, we switched to a lightweight polypropylene mesh (Optilene, Braun, Melsungen, Germany). The meshes were routinely positioned retromuscularly with minimum 5 cm overlap of the fascial defect and fixed with interrupted 2/0 polypropylene sutures (Prolene, Ethicon, Norderstedt, Germany). During minimally invasive intraperitoneal onlay mesh (IPOM), a non-absorbable polypropylene mesh (Proceed, Ethicon, Norderstedt, Germany) was fixed with four 2/0 polypropylene sutures (Prolene, Ethicon, Norderstedt, Germany) and absorbable tacks (Securestrap, Ethicon, Norderstedt, Germany) in double crown technique.
Outcome parameters
The primary outcome parameter was mesh infection and defined as detection of bacteria through microbial swab of the mesh, purulent drainage with direct mesh contact or documented mesh explantation due to bacterial infection.
Secondary outcome parameters were defined as SSI, re-operation for SSI, hernia recurrence, chronic pain assessed with numeric rating scale (mild 0–3 versus moderate to severe 4–10), chronic dysesthesia (mild 0–3 versus moderate to severe 4–10), post-operative recovery time (≤16 versus >16 weeks), cosmetic (dissatisfied 0–3 versus partly to completely satisfied 4–10), overall treatment (dissatisfied 0–3 and partly to completely satisfied 4–10), theoretically re-consent to original surgery.
Collection of clinical data
Patient and hernia characteristics at time of surgery were retrospectively obtained from chart review and included gender, age, immunosuppressants, diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), hernia type, body mass index (BMI), smoking status, current and/or past history of solid and/or haematological malignancies.
Long-term follow-up
Written follow-up questionnaires were distributed via postal mail. Patients who did not return the questionnaire were contacted by phone for an interview.
Statistical analysis
Sample size calculation was based on the assumption of 13% mesh infection rate for immunocompromised and 2% for immunocompetent patients.7-9 In order to reject the null-hypothesis (equal mesh infection rates with 80% power on a two-sided α-level of 0.05 by two group chi-squared test), 44 immunocompromised (case) and 176 immunocompetent patients (control) had to be analysed. Considering a drop-out rate of 10%, 48 immunocompromised and 194 immunocompetent patients (Ntotal = 242) needed to be recruited. Sample size calculation was done with nQuery 7.0 (Statistical Solutions Ltd., Cork, Ireland).
Descriptive analyses included absolute and relative frequencies for categorical variables, mean with standard deviation and median with interquartile range (IQR) for quantitative measurements. Pearson's chi-squared or Fisher's exact was used to test for independence of categorical variables. Non-parametric Mann–Whitney U-test was used to test for independence of two independent groups with a continuous dependent variable. Independent variables in the univariate analysis with P < 0.2 were included in multivariate logistic regression. Results of multivariate analyses are reported as odds ratio (OR) with 95% confidence interval (CI) and P-value. The level of significance was α = 0.05 with 95% CI. Statistical analysis was performed with IBM SPSS 25 software (IBM, Armonk, NY, USA).
Results
Study cohort and demographics
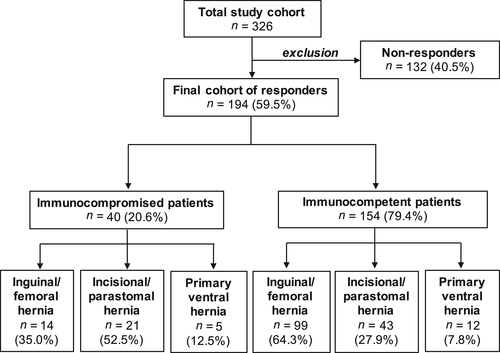
The questionnaire response rate was 59.5% with the majority of responders being male (74.7%) and 20.6% being immunocompromised (Fig. 1). There were no differences between questionnaire responders and non-responders based on gender, age, BMI, DM, COPD and type of hernia (data not presented). The median age was 60 (IQR: 44–70) years with a median BMI of 25.6 (IQR: 23.1–28.1) kg/m2 (Table 1). Median follow-up from surgery to questionnaire was 33 (IQR: 28–41) months. Among 194 patients, 41 (21.1%) patients were diabetic, while among 40 immunocompromised patients, 13 (32.5%) patients were diabetic.
| Patient and hernia characteristics | Final cohort, n = 194 |
|---|---|
| Gender, n (%) | |
| Female | 49 (25.3) |
| Male | 145 (74.7) |
| Age (years), median (IQR) | 60.50 (46.75–71.00) |
| BMI (kg/m2), median (IQR) | 25.60 (23.10–28.10) |
| Type of immunosuppression, n = 40, n (%) | |
| Systemic chemotherapy/chemoradiotherapy | 10 (25) |
| Any combination of immunosuppressants | 30 (75) |
| Diabetes mellitus, n (%) | 41 (21.1) |
| COPD, n (%) | 8 (4.1) |
| Smoking, yes, n (%) | 39 (20.1) |
| Cancer, yes, n (%) | 51 (26.3) |
| Type of hernia, n (%) | |
| Inguinal, femoral | 113 (58.2) |
| Primary ventral | 64 (33.0) |
| Incisional, parastomal | 17 (8.8) |
- BMI, body mass index; COPD, chronic obstructive pulmonary disease; IQR, interquartile range.
The percentages of hernia types among immunocompromised patients compared to immunocompetent patients are shown in Figure 1. Immunosuppression was not associated with gender (P = 0.714), age (P = 0.104), COPD (P = 0.365) or BMI (P = 0.661).
Hernia repair
Immunocompromised patients underwent Lichtenstein (n = 11, 27.5%), TEP (n = 3, 7.5%), TAPP (n = 1, 2.5%), sublay (n = 19, 47.5%), laparoscopic IPOM (n = 2, 5.0%), open IPOM (n = 1, 2.5%) and other (n = 3, 7.5%). Immunocompetent patients also underwent Lichtenstein (n = 43, 27.9%), TEP (n = 30, 19.5%), TAPP (n = 25, 16.2%), sublay (n = 52, 33.8%), laparoscopic IPOM (n = 2, 1.9%), onlay (n = 1, 0.6%) and other (n = 1, 0.6%).
Effects of immunosuppression on wound complications
The rates of mesh infection, SSI and re-operation for SSI were not significantly affected by immunosuppression (Table 2). The type of immunosuppression (immunosuppression versus chemotherapy/chemoradiotherapy) was not associated with the rates of SSI (P = 0.306), mesh infection (P = 0.250) or re-operation for SSI (P = 0.560). The overall 30-day post-operative mortality was zero.
| Immunocompromised (n = 40) | Immunocompetent (n = 154) | P-value | |
|---|---|---|---|
| Mesh infection, n (%) | 1 (2.5) | 4 (2.6) | 1.000 |
| SSI, n (%) | 5 (12.5) | 11 (7.1) | 0.330 |
| Re-operation for SSI, n (%) | 3 (7.5) | 5 (3.2) | 0.365 |
| Hernia recurrence, n (%) | 11/39 (28.2) | 16 (10.4) | 0.008* |
| Post-operative course, n (%) | |||
| Pain (NRS > 3) | 7 (17.5) | 18 (11.7) | 0.425 |
| Dysesthesia (NRS > 3) | 5 (12.5) | 22 (14.3) | 1.000 |
| Recovery (>16 weeks) | 7/38 (18.4) | 17/151 (11.3) | 0.275 |
| Cosmetic satisfaction (<4), n (%) | 8 (20) | 19/153 (12.4) | 0.212 |
| Treatment satisfaction (<4), n (%) | 4 (10) | 16 (10.4) | 1.000 |
| Re-consent to surgery: yes, n (%) | 35 (87.5) | 134/152 (88.2) | 1.000 |
- NRS, numeric rating scale; SSI, surgical site infection.
Predictors of mesh infection, SSI and hernia recurrence
In univariate analysis, SSI was associated with DM (P = 0.048) and hernia type (P = 0.033, Table 3), but not in multivariate analysis. Increased BMI was a risk factor for SSI (OR 1.115, 95% CI 1.002–1.242, P = 0.047).
| SSI (n = 16) | Non-SSI (n = 178) | P-value | |
|---|---|---|---|
| Patient and hernia characteristics | |||
| Age (years), median (IQR) | 61 (72–49) | 60 (71–46) | 0.477 |
| Gender, n (%) | |||
| Female | 6 (37.5) | 43 (24.2) | 0.241 |
| Male | 10 (62.5) | 135 (75.8) | |
| Immunosuppression, n (%) | 5 (31.3) | 11 (68.8) | 0.330 |
| Diabetes mellitus, n (%) | 7 (43.8) | 34 (19.1) | 0.048* |
| COPD, n (%) | 1 (6.3) | 7 (3.9) | 0.504 |
| BMI (kg/m2), median (IQR) | 25.6 (23.10–33.08) | 25.55 (23.13–28.00) | 0.309 |
| Smoking, n (%) | 3 (18.8) | 36 (20.2) | 1.000 |
| Malignancy, n (%) | 4 (25.0) | 47 (26.4) | 1.000 |
| Type of hernia, n (%) | |||
| Inguinal/femoral | 5 (31.1) | 108 (62.4) | 0.033* |
| Primary ventral | 1 (6.3) | 16 (9.0) | |
| Incisional/parastomal | 10 (62.5) | 54 (30.3) | |
| Operative outcome | |||
| Post-operative course, n (%) | |||
| Pain (NRS > 3) | 4 (25.0) | 21 (11.8) | 0.133 |
| Dysesthesia (NRS > 3) | 6 (37.5) | 22 (14.3) | 0.013* |
| Recovery (>16 weeks) | 3 (20.0) | 21 (12.1) | 0.412 |
| Cosmetic satisfaction (<4), n (%) | 3 (18.8) | 24 (13.6) | 0.474 |
| Treatment satisfaction (<4), n (%) | 4 (25.0) | 16 (9.0%) | 0.066 |
| Re-consent to surgery, yes, n (%) | 10 (62.5) | 159 (90.3) | 0.006* |
- BMI, body mass index; COPD, chronic obstructive pulmonary disease; IQR, interquartile range; NRS, numeric rating scale.
The rate of hernia recurrence was significantly higher among immunocompromised patients (28.2%, P = 0.008) and also associated with mesh infection (P = 0.020, Table 2). The OR for hernia recurrence was three times higher among all immunocompromised patients (P = 0.012) and nearly 12-fold for all patients (with and without immunosuppression) with post-operative mesh infection (P = 0.011, Fig. 2). Additionally, only in the subset of ventral/incisional hernias, immunocompromised (n = 8, 40%) patients had higher recurrence rates than immunocompetent patients (n = 5, 11.6%; P = 0.017).
Effects of SSI on post-operative course
Patients with SSI more frequently reported moderate to severe chronic dysesthesia (numeric rating scale > 3) at the surgical site (P = 0.013). However, SSIs did not impact the patients' post-operative pain, recovery and treatment satisfaction (Table 3). The majority of patients without any post-operative wound complications (90.3%) would re-consent to their original hernia surgery if given the choice again. Among those with post-operative wound complications, 62.5% would still re-consent (P = 0.006).
Discussion
In this retrospective study, we investigated the effects of immunosuppression on the safety of synthetic mesh during elective hernia repair. Because of insufficient and partially conflicting data, many surgeons face the challenge of adequate risk assessment for potential post-operative complications among immunocompromised hernia patients, particularly when synthetic mesh is going to be used. Yet, the surgical management of this subset of high-risk patients is not specifically considered in international guidelines. We included a comprehensive list of immunosuppressants to reflect the daily practice at a tertiary centre in Germany. Our results showed no effect of immunosuppression on the rates of mesh infection, SSI and re-operation for SSI. However, the rate of hernia recurrence among immunocompromised patients was significantly higher when compared to immunocompetent patients.
Prior data also suggested that synthetic mesh was safe in patients with incisional hernias after orthotopic liver transplantation. However, it should be noted that their statistical power may be compromised due to small sample size (n = 15).9 Another analysis found that polypropylene mesh repairs of infected herniation sites in kidney transplanted patients were safe with a 9.1% recurrence rate.8 Compared to our study, their recurrence rate may have been lower, but their cohort (n = 13) was smaller with a shorter follow-up (16 months). The recurrence rate in our study was 28.2% among 40 immunocompromised patients with a median follow-up of 33 months.
Another series of ventral hernia repairs in immunocompromised patients (n = 18, 21%) reported a 16% SSI rate with conservative management in the majority of cases. Only 3% required re-operation for SSI and the hernia recurrence rate was 5%. The conclusion was that synthetic mesh could be safely applied in high-risk patients.10 However, ventral hernia patients with ‘same-site concomitant surgery’ (hazard ratio = 6.3) or SSI (hazard ratio = 6.5) had significantly higher risk for mesh explantation regardless of the surgical procedure.11 Although details about the nature of ‘same-site concomitant surgery’ were not given, we presume significant bowel manipulation with increased risk for contamination.
Based on a retrospective analysis of ventral hernia repairs (n = 342) with 85% re-admission rate due to post-operative deep wound infection, the majority of cases could be successfully managed with negative pressure therapy.12 Our low rates of re-operation for SSI also support conservative management as first choice of therapy. However, it should be noted that in our study the rates of re-operation for SSI were slightly higher for the subset of immunocompromised patients, although statistical significance was not reached (Table 2). Also not statistically significant, but immunocompromised patients appeared to have more SSIs compared to immunocompetent patients: 12.5% versus 7.1%. This warrants further investigation in a larger cohort to analyse the potentially full effect of immunosuppression on post-operative wound complications.
The impact of surgical approach on wound complications was investigated in another retrospective analysis of immunocompromised liver transplant patients who underwent incisional hernia repair. The laparoscopic approach showed trends for shorter hospitalization, lower infection and recurrence rates.13 This study did not explicitly investigate the effect of immunosuppression on mesh infection rates. However, another retrospective study addressed this question in 31 laparoscopic incisional hernia repairs with synthetic mesh in immunocompromised patients with a history of solid-organ transplantation. Surprisingly, no post-operative wound infection occurred but 23% of the patients developed recurrent hernia.14
Further retrospective analysis of liver transplant patients with standard triple immunosuppression who underwent incisional hernia repair showed that immunosuppression and suture closure were independent risk factors for hernia recurrence.15 Our data also showed that immunocompromised patients had three times higher odds for recurrence (Fig. 2).
Compared to prior studies, our subset of immunocompromised patients is larger and the follow-up longer. In addition to molecular studies discovering the mechanism through which specific immunosuppressive drugs modulate wound healing,16 we further provide clinical data on the impact of immunosuppression on wound healing with synthetic mesh. Additionally, we analysed patient reported outcome parameters (Tables 2 and 3). These ‘subjective factors’ play an important role for the patient's well-being and quality of life. Less than 20% of patients were not satisfied with the cosmetic result of their surgical wound, regardless of SSI. Patients with SSI more frequently reported moderate to severe post-operative dysesthesia, which might be explained by nerve disturbances through prolonged secondary wound healing and/or surgical debridement. In a long-term follow-up study about the improvement of symptoms that were caused by incisional hernias, the majority benefitted from surgical repair. Still 18 months post-operatively, the rates of clinically relevant dysesthesia were 12.5% and 20.9% for oligosymptomatic and symptomatic patients, respectively. For post-operative pain, the rates were 7.5% and 14% among oligosymptomatic and symptomatic patients, respectively.17
In our study, immunosuppression had no effect on pain. Patients with SSI tended to be less satisfied with the overall treatment and would less re-consent to the original hernia repair. These data show that SSIs negatively impact the patients' perception of their post-operative course and have long-term sequelae.
Limitations of the study
This was a retrospective analysis of a prospectively kept database. The study cohort was heterogeneous in terms of immunosuppression, hernia type, hernia repair and duration of follow-up. The response rate to the questionnaire was only 59.5%, but without differences between responders and non-responders in terms of patient characteristics. Follow-up data are based on patient reported outcomes without physical examination and with its inherent limitations.
Conclusion
Our results indicate that the use of synthetic mesh in immunocompromised patients is not associated with higher rates of postoperative wound complications. However, immunocompromised patients may be at higher risk for recurrence.
Conflicts of interest
None declared.