Successful heart transplantation from donation after euthanasia with distant procurement using normothermic regional perfusion and cold storage
Vincent Tchana-Sato and Gregory Hans contributed equally to this work.
Didier Ledoux and Filip Rega share the senior authorship of this work.
Abstract
While euthanasia has been legalized in a growing number of countries, organ donation after euthanasia is only performed in Belgium, the Netherlands, Spain, and Canada. Moreover, the clinical practice of heart donation after euthanasia has never been reported before. We describe the first case of a heart donated after euthanasia, reconditioned with thoraco-abdominal normothermic regional perfusion, preserved using cold storage while being transported to a neighboring transplant center, and then successfully transplanted following a procurement warm ischemic time of 17 min. Heart donation after euthanasia using thoraco-abdominal normothermic regional perfusion is feasible, it could expand the heart donor pool and reduce waiting lists in countries where organ donation after euthanasia can be performed.
Abbreviations
-
- ACR
-
- acute cellular rejection
-
- CPB
-
- cardiopulmonary bypass
-
- CS
-
- cold storage
-
- DCD
-
- donation after circulatory death
-
- HT
-
- heart transplantation
-
- LVAD
-
- left ventricular assist device
-
- POD
-
- postoperative day
-
- SR
-
- sinus rhythm
-
- TA-NRP
-
- thoraco-abdominal normothermic regional perfusion
-
- VA-ECMO
-
- veno-arterial extracorporeal membrane oxygenation
1 INTRODUCTION
Transplantation of hearts donated after circulatory death (DCD) has emerged as a valuable strategy to expand the donor pool.1 To date, DCD heart procurement has been performed in type III Maastricht donors2 while heart donation following euthanasia (type V Maastricht donors) has not been reported yet. To our knowledge, organ donation following euthanasia is only practiced in Belgium, the Netherlands, Spain, and Canada. Our center published the first report on organ donation after euthanasia in 2008.3
In Belgium, DCD heart transplantation (HT) (type III Maastricht donors) is performed using in situ thoraco-abdominal normothermic regional perfusion (TA-NRP).4, 5 In the University Hospital of Liège, this protocol was amended to allow heart donation after euthanasia and was accepted by the hospital's Ethics Committee (Table 1). The authors describe a case of DCD heart procurement following euthanasia using TA-NRP and cold storage (CS), followed by successful HT in a distant center.
| DCD-III protocol | DCD-V protocol | |
|---|---|---|
| Location of WLST/Euthanasia | Operating room | Ward (patient's room) |
| Antemortem intervention |
Heparin Peripheral placement of ECMO cannula |
Heparin |
| Transportation to the OR | n/a | During the 5 min no-touch period |
| Death | Circulatory arrest +5 min | Circulatory arrest +5 min |
| Post-mortem interventions | Normothermic regional perfusion |
Central placement of CPB cannula Normothermic regional perfusion |
| Graft retrieval | NRP-SCS | NRP-SCS |
- Abbreviations: CPB, cardiopulmonary bypass; DCD, donation after circulatory death; n/a, not applicable; NRP-SCS, normothermic regional perfusion with static cold storage; OR, operating room; WLST, withdrawal of life-sustaining therapy.
2 CASE REPORT
2.1 Donation request
A 46-year-old man diagnosed with amyotrophic lateral sclerosis approached our center with a request for euthanasia. His medical history was otherwise unremarkable. The patient spontaneously and explicitly expressed his wish to donate his organs, and of the utmost importance to him, his heart. He was thoroughly examined by multiple independent specialists who confirmed the poor prognosis and that the patient's wish for euthanasia met the criteria of Belgian law. The patient's request was eventually accepted. We aimed for a strict separation between euthanasia and organ donation procedures. The patient's wish was to be admitted to the hospital only one day before euthanasia for a routine work-up. The DCD practical modalities following euthanasia including premortem administration of heparin, postmortem central cannulation, and initiation of TA-NRP, were explained and agreed to by the patient. The heart was allocated to a suitable 65-year-old female recipient with a left ventricular assist device (LVAD) in a distant center (University Hospitals) through Eurotransplant.
2.2 The euthanasia procedure
The euthanasia procedure was carried out in the presence of his relatives, in a private room. Loss of consciousness was induced using a combination of sufentanil 10 mcg, propofol 400 mg, and diazepam 100 mg. Once the patient became unresponsive, a bolus of 30.000 IU of heparin was given before induction of circulatory arrest by injection of 40 mEq potassium chloride. The clinical determination of cardiocirculatory arrest was based on the disappearance of heart sounds, femoral, and carotid arterial pulses, and was associated with the appearance of bilateral fixed mydriasis at 8 mm.
2.3 Organ procurement
According to our local DCD protocol, the no-touch period started at the time of the circulatory arrest. The patient was transported to the operating room during the 5-min no-touch period. The patient was then moved onto the operating table. Death was declared at the end of the 5-min no-touch period, shortly after his positioning. Surgical skin preparation and draping were performed.
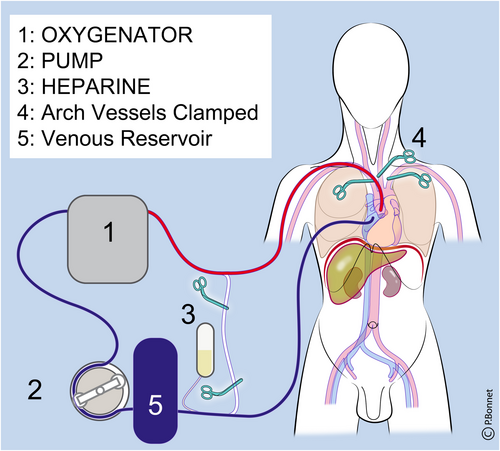
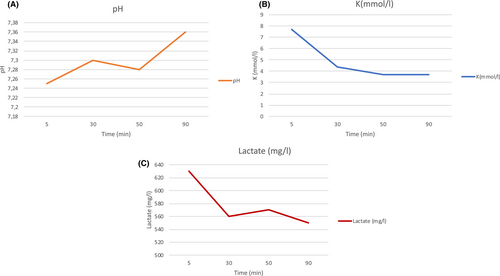
A rapid sternotomy was performed followed by clamping of all three supra-aortic vessels. A two-stage venous cannula was placed into the right atrium, and an arterial cannula was placed into the ascending aorta prior to the initiation of mechanical lung ventilation. Cannulas were connected to a cardiopulmonary bypass (CPB) circuit (Figure 1) and in situ TA-NRP was initiated after a warm ischemic interval of 17 min. Within 86 s of in situ reperfusion, the DCD heart spontaneously reverted to sinus rhythm (SR). We observed a rapid decrease in serum potassium and lactate after the initiation of TA-NRP, and the arterial pH gradually returned to normal (Figure 2). A femoral arterial line was inserted to allow measurement of the arterial pressure. Given the rapid and spontaneous reversion to SR, in addition to the excellent contractility of both ventricles observed on the transoesophageal echocardiography images,6 no inotrope infusion was required. After 42 min of TA-NRP, contractility sufficiently recovered to solely support regional perfusion of the thorax and the abdomen. There was a 52-minute preparation interval between cessation of TA-NRP and cross-clamping to allow the cold flush of the heart, the lungs, and the abdominal organs (Table 2).
| Donor | |
|---|---|
| Age (years) | 46 |
| Gender | Male |
| Height (cm) | 176 |
| Weight (kg) | 65 |
| Underlying disease motivating the euthanasia request | Amyotrophic lateral sclerosis |
| Euthanasia drugs administration to circulatory arrest (min) | 1 |
| pWIT (min) | 17 |
| Knife to skin to onset of NRP (min) | 9 |
| NRP duration (min) | 42 |
| Restoration of spontaneous sinus rhythm after NRP (Sec) | 86 |
| DCD donor heart functional assessment 30 min after NRP | |
| MAP (mm Hg) | 55 |
| LVEF | >60% |
| CO (L/min)/ CI (L/min/m2) | Not measured |
- Abbreviations: CI, cardiac index; CO, cardiac output; LVEF, left ventricular ejection fraction; MAP, mean arterial pressure; NRP, normothermic regional perfusion; pWIT, procurement warm ischemic time (time between the administration of the euthanasia drugs and restoration of normothermic regional perfusion).
Cardiectomy was carried out in a standard fashion. After procurement, the heart graft was stored on ice. The kidneys, lungs, pancreas, and liver were also recovered and successfully transplanted.
2.4 Transplantation
The heart was implanted using a bicaval technique with an implantation time of 49 min. The total ischemic time was 184 min (including the 17 min of warm ischemia prior to the onset of TA-NRP).
Thirty minutes after the onset of reperfusion, a hemodynamic stable situation was reached with moderate inotropic support and the patient could be weaned off CPB. The driveline from the LVAD was removed. Forty-five minutes after stopping CPB, the hemodynamic situation slowly deteriorated reflected by an increased inotropic support need and signs of right ventricular failure on echocardiography. The decision was made to start peripheral veno-arterial extracorporeal membrane oxygenation (VA-ECMO), resulting in improved hemodynamics. However, 1 h after installation of the VA-ECMO, the hemodynamic situation deteriorated further (increased inotropic and vasopressor support, declining mean arterial pressure). An Impella CP (Abiomed) was placed to further support the systemic circulation and unload the left ventricle. In the hours that followed in the intensive care unit, the hemodynamic situation continued to deteriorate with a clinical picture that was dominated by progressive hypotension responding to volume expansion, abdominal distention, and hemoglobin loss. Abdominal ultrasound revealed a significant intraperitoneal hemorrhage. A laparotomy was performed visualizing important bleeding of the right superior epigastric artery where the driveline was extracted.
On postoperative day (POD) six, the recipient was weaned from all mechanical circulatory support. On POD fourteen, the patient was extubated. She was subsequently transferred to the ward on POD twenty-seven. Grade 1R acute cellular rejection (ACR, ISHLT 2004) was diagnosed on routine biopsy 1 month after heart transplantation. The patient went home in good health on POD 65 and is currently doing well 225 days after her transplantation. On follow-up, the left ventricular ejection fraction was 60% with a cardiac output of 4.7 L/min. The last biopsy showed no signs of ACR (grade 0 [ISHLT 2004]).
3 DISCUSSION
To our knowledge, this report represents the first transplantation of a heart donated after euthanasia using TA-NRP followed by cold static storage (CS).
DCD heart donation increased overall heart transplant activity with no difference in survival in comparison with conventional donors in brain death heart transplantations thereby effectively expanding the donor pool.7 In Belgium, we choose TA-NRP followed by CS above direct procurement in this setting saving costs by avoiding expensive normothermic machine perfusion preservation.4
We cannot understate enough that our donor expressed the explicit will to donate. Separation of the donor and recipient procedure, careful informed consent, and independent confirmation of the patients' will are crucial.8
In our case, it was difficult to differentiate between primary graft dysfunction and vasoplegia resulting from the hemorrhage in the root cause analysis of the hemodynamic instability. After the laparotomy and finding out how much blood had accumulated in the abdomen we understood the importance of the hemorrhage in the clinical picture. Fortunately, the patient made a good recovery with normal heart function at 6 months.
4 CONCLUSION
The authors describe the successful clinical transplantation of a DCD heart recovered following euthanasia using TA-NRP. Heart donation after euthanasia might be a valuable resource for clinical transplantation and could contribute to reducing organ shortages in countries with an appropriate legal framework.
ACKNOWLEDGMENTS
The corresponding author would like to thank the transplant coordinators, as well as the health care professionals in the ICU, and in the OR of the CHU Liege and The University Hospitals of Leuven, for their contributions. Thanks to Dr Pierre Bonnet, for his help with the illustrations.
FUNDING INFORMATION
None.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this report are available from the corresponding author, VTS, upon reasonable request.